-
PDF
- Split View
-
Views
-
Cite
Cite
Evgeniya V Shalaeva, Hugo Saner, Bakhtiyor B Janabaev, Aleksandra V Shalaeva, Tenfold risk increase of major cardiovascular events after high limb amputation with non-compliance for secondary prevention measures, European Journal of Preventive Cardiology, Volume 24, Issue 7, 1 May 2017, Pages 708–716, https://doi.org/10.1177/2047487316687103
Close - Share Icon Share
Abstract
The aim of the study was to evaluate the impact of compliance with lifestyle recommendations and medication on 1-year prevention of major adverse cardiovascular events (MACE) in patients with type 2 diabetes (T2D) after trans-femoral amputation (TFA).
In this prospective single-center interventional cohort study, 179 consecutive T2D patients with symptomatic coronary artery disease (CAD) underwent 1-year follow-up examination after TFA in 2013. Lower limb and coronary artery CT angiography were provided before surgery; physical examination and laboratory tests were performed at baseline and every month after TFA for 1 year. A total of 77 patients (43%) were defined as compliant. They followed all recommendations, including >80% drug intake (anti-diabetic, antihypertensive drugs, dual antiplatelet and statin treatment), healthy diet, smoking cessation, physical exercise ≥30 min/day. A total of 102 patients (57%) were non-compliant (drug intake ≤80%, and did not fully follow lifestyle change recommendations).
There were no significant differences at baseline between the two groups. Fuster-BEWAT score in 1 year was 9.83 ± 3.1 in compliant and 7.74 ± 2.9 in non-compliant patients (p = 0.0001). At 1-year follow-up, there were 43 myocardial infarctions (40 patients (93%) were non-compliant) and 28 deaths (26 cases (92.8%) were non-compliant). Patients from the non-compliant group with three- and two-vessel obstructive CAD had higher 1-year MACE rate than those with one-vessel obstructive and non-obstructive CAD (95.24% and 70.5% versus 17.2% and 8.6%; p < 0.0001); more proximal coronary lesions were related to a worse prognosis.
Non-compliant diabetic patients had a tenfold increased risk for MACE within 1 year after TFA.
- antihypertensive agents
- myocardial infarction
- coronary arteriosclerosis
- coronary artery
- statins
- diabetes mellitus
- amputation
- diabetes mellitus, type 2
- smoking cessation
- physical examination
- exercise
- limb
- follow-up
- laboratory techniques and procedures
- life style
- surgical procedures, operative
- leg
- surgery specialty
- secondary prevention
- lifestyle changes
- cardiovascular event
- coronary lesions
- healthy diet
- prevention
Introduction
Patients with Type 2 diabetes (T2D) are at increased risk for the development of microvascular and macrovascular complications. The risk of lower extremity artery disease (LEAD) in T2D increases two- to four-fold with 20–30% prevalence.1 Three-year survival after an amputation in patients with T2D and LEAD is less than 50%.2
Compliance with recommendations for lifestyle changes and medication is essential for secondary prevention of major adverse cardiovascular events (MACE). In many cases, a cluster of cardiovascular risk factors including high blood pressure (BP), and dyslipidemia together with unfavorable lifestyle factors further increases this risk. Evidence from clinical studies indicates that MACE in patients with T2D may be reduced by rigorous control of three key modifiable risk factors, namely glycaemia, BP, and low-density lipoprotein cholesterol (LDL-C).3 However, non-compliance with medication and recommendations for lifestyle changes has turned out to be a major contributor to increased complication rates and impaired prognosis.
Major reasons for noncompliance include patients’ inability to pay for treatment,4 patients’ reluctance to take medication long term, in particular under asymptomatic conditions such as dyslipidemia,5 requirement to take medication with more than once-daily administration,6 and a poor provider–patient relationship.7 In addition, younger patients (<45 years) appear more likely to be non-compliant with treatment.8
Despite the fact that reducing LDL-C with statins is recommended as first-line therapy by current treatment guidelines,9,10 many patients fail to achieve recommended lipid levels in clinical practice.11 Indeed, EUROASPIRE IV survey showed that almost 81% had LDL-C ≥1.8 µmol/l.12
The aim of the study was to evaluate the impact of compliance with preventive recommendations and medication on 1-year prevention of MACE in patients with T2D after trans-femoral amputation (TFA).
Methods
This is a prospective single-center interventional cohort study. In 2013, we operated on 2354 diabetic patients with purulent necrotic complications. All patients were included in further follow-up examinations. Among 2354 patients, 389 T2D patients with symptomatic coronary artery disease (CAD) underwent TFA of one hip due to limb gangrene with intact second lower extremity. Patients who previously underwent amputation of one lower limb and at the time of admission had critical LEAD of the remaining lower limb requiring TFA were not included. In this study, we analyzed and interpreted 1-year follow-up data of 179/389 T2D patients without history of previous MACE (myocardial infarction (MI), and/or revascularization) or stroke, valvular heart disease, atrial fibrillation; and had no clinical picture and ECG findings of acute coronary syndrome, MI, elevated initial troponin level on admission. These patients also had no contraindications to lower limb arteries and coronary computed tomographic angiography (CCTA; including blood creatinine ≤1.5 mg/dl or 133 µmol/l), which was performed before surgery using a 64 detector rows CT scanner GE USA ‘Light speed’ VCT cardiac 72013287YA 2008.
CCTA was interpreted using an 18-segment coronary vascular model according to SCCT guidelines for the interpretation and reporting of CCTA. At least three contiguous pixels with a density of >130 HU were identified as calcium. Lesions greater than 1 mm2 within or adjacent to the vessel lumen were defined as plaques. The extent of CAD was assessed by the number of vessels with CAD (left anterior descending, left circumflex, and right coronary artery) as 1-vessel, 2-vessels and 3-vessel/left main disease, assuming that stenosis = 0 is not CAD, non-obstructive CAD had stenosis 50%, and obstructive CAD with coronary artery stenosis > 50% [13].
Baseline characteristics were retrieved on the day of the scans by dedicated research personnel. We defined systemic arterial hypertension as a systolic BP > 140 mmHg, diastolic BP > 90 mmHg, or diagnosis/treatment of hypertension. BP measurements were performed according to the 2013 ESH/ESC Guidelines for the management of arterial hypertension.14 Smoking was defined as current (tobacco products used within the last month) or never. Family history of premature CAD was defined as any first-degree family member with a history of clinical CAD prior to age 60. T2D was defined by a hemoglobin A1C ≥ 6.5%, physician-based diagnosis, and use of anti-diabetic medications.15
Physical examination and laboratory tests were performed at baseline and were repeated every month after TFA. Results are presented as findings at baseline, 7 days, 10–14 days, 1, 3, 6 months, and 1 year after operation.
Compliance initiatives
Compliance recommendations included diet (food table 9), smoking cessation (if smokers), physical exercise ≥30 min/day and >80% drug intake (anti-diabetic, antihypertensive drugs, dual antiplatelet and statin treatment). Patients were identified as compliant if they followed all recommendations, including >80% medication adherence, healthy diet, smoking cessation and physical exercise ≥30 min/day. Patients considered non-compliant if drug intake was ≤80%, and they did not fully follow lifestyle change recommendations.
Patients and relative caregivers (with patients’ permission) received a starter package containing an educational leaflet, details of the free phone patient helpline and website, and labels with a reminder to take the study medication, a notepad and calendar with detailed instructions of time, dosage and duration of prescribed treatment, and diaries for registering drug intake, physical exercise and diet. Patients and close relatives also received regular personalized letters and phone calls throughout the study. At every examination, patients and caregivers were asked to present their notepads with daily drug intake, redeemed prescriptions and blisters of prescribed medications. If the patient did not take the drugs as prescribed, we searched for reasons, conducted interviews and provided training to improve compliance. Local outpatient clinics provided anti-diabetic drugs and insulin, and some antihypertensive treatment for free. Particular attention was paid to dual antiplatelet therapy (aspirin 75–150 mg + clopidogrel 75 mg daily) and atorvastatin 80 mg daily, for which costs had to be covered by patients themselves after hospital discharge.
Clinical outcomes
The clinical endpoint in this study was MACE, which was defined as cardiovascular death or non-fatal MI. Cardiovascular death was identified as death due to MI, congestive heart failure, stroke or arrhythmias or any unknown causes of death not explained by non-cardiac etiologies. Diagnosis of MI was confirmed by two of three findings: chest pain or equivalent symptom complex; positive cardiac biomarkers; ECG changes typical of MI.16 In patients who had multiple cardiac events, only one was counted toward MACE. Follow-up cardiac events were investigated by chart review, telephone interview and confirmation with death certificate.
Fuster-BEWAT score (0 to 15) was used to describe the outcome in relation to compliance as a mean change in a composite score related to BP, exercise—physical activity (PA), weight, alimentation and tobacco (0 to 3 points each).17 No points for PA have been allocated at admission because of lower limb gangrene. If patients after amputation increased their PA to ≥30 minutes per day (exercise in bed, going for a walk on a mechanical wheelchair that requires active hands working), we added 1 point. If patients went for walks using the crutches with/without prostheses, we added 2 points.
Statistical analysis
Descriptive statistics for variables are presented as mean ± SD for normally distributed continuous variables, frequency as a percentage for categorical variables. Variables were compared with independent Student t tests for normally distributed continuous data, and chi-squared test for categorical data, Kaplan–Meier curves for event-free survival from cardiovascular death and nonfatal MI for CCTA results.
Research ethics and patient consent
Ethical approval was received from the Republican Center of Purulent Surgery and Complications of Diabetes and Tashkent Medical Academy Ethics Review Board. Medical care specialists maintain privacy and confidentiality of all medical records and data. Information about patients’ health conditions, follow-up examination, secondary and tertiary prevention strategies were also provided to family members and health care providers after patient’s permission and signed informed consent.
Results
The study cohort comprises of 179 T2D patients (109 male and 70 female) with symptomatic CAD undergoing TFA with a mean age of 60.4 ± 8.8 years. Female were significantly older than men (68.1 ± 5.9 versus 57.2 ± 6.2 years, p = 0.001). The majority of patients undergoing TFA had comorbidities and septic symptoms (septicemia was present in 27.9%, sepsis in 56.4% and severe sepsis in 14.5% of patients). All patients had dyslipidemia, 90% of patients suffered from arterial hypertension, 74.3% had congestive heart failure and 50% were obese (Table 1). There were no significant differences in baseline characteristics with regards to age, gender, disease severity, comorbidities and clinical CAD at the time of amputation) between the two groups (Table 1). Fuster-BEWAT score before operation was similar in both groups: 5.33 ± 2.7 in compliant and 5.48 ± 2.9 in non-compliant patients.
Baseline characteristics of 179 patients with type 2 diabetes undergoing surgery for lower limb amputation.
| Variable, n (%) . | Total (n = 179) . | Compliant (n = 77) . | Non-compliant (n = 102) . | p-value . |
|---|---|---|---|---|
| Age, years | 60.4 ± 8.8 | 58.9 ± 10.1 | 60.3 ± 8.5 | 0.316 |
| Gender, n (%) | ||||
| Male | 109 (60.9) | 46 (59.7) | 63 (61.8) | 0.877 |
| Female | 70 (39.1) | 31 (40.3) | 39 (38.2) | |
| Arterial hypertension | 161 (89.9) | 70 (90.9) | 91 (89.2) | 0.805 |
| Arterial hypotension (Systolic ˂90 mmHg) | 18 (10.3) | 7 (9.1) | 11 (10.8) | 0.805 |
| Obese | 93 (52) | 39 (50.6) | 54 (52.9) | 1.0 |
| Dyslipidemia | 179 (100) | 77 (100) | 102 (100) | 1.0 |
| Previous statin use | 30 (16.7) | 18 (23.4) | 12 (11.8) | 0.045 |
| Current smoking | 99 (55.3) | 42 (54.5) | 57 (55.9) | 0.88 |
| Family history of CAD | 140 (78.2) | 62 (80.5) | 78 (76.5) | 0.585 |
| Clinical CAD | 179 (100) | 77 (100) | 102 (100) | 1.0 |
| Congestive heart failure | 133 (74.3) | 60 (77.9) | 73 (71.6) | 0.389 |
| Septicemia | 50 (27.9) | 18 (23.3) | 32 (31.4) | 0.313 |
| Sepsis | 101 (56.4) | 54 (70.1) | 47 (46.1) | 0.0014 |
| Severe sepsis | 26 (14.5) | 7 (9.1) | 19 (18.6) | 0.088 |
| Variable, n (%) . | Total (n = 179) . | Compliant (n = 77) . | Non-compliant (n = 102) . | p-value . |
|---|---|---|---|---|
| Age, years | 60.4 ± 8.8 | 58.9 ± 10.1 | 60.3 ± 8.5 | 0.316 |
| Gender, n (%) | ||||
| Male | 109 (60.9) | 46 (59.7) | 63 (61.8) | 0.877 |
| Female | 70 (39.1) | 31 (40.3) | 39 (38.2) | |
| Arterial hypertension | 161 (89.9) | 70 (90.9) | 91 (89.2) | 0.805 |
| Arterial hypotension (Systolic ˂90 mmHg) | 18 (10.3) | 7 (9.1) | 11 (10.8) | 0.805 |
| Obese | 93 (52) | 39 (50.6) | 54 (52.9) | 1.0 |
| Dyslipidemia | 179 (100) | 77 (100) | 102 (100) | 1.0 |
| Previous statin use | 30 (16.7) | 18 (23.4) | 12 (11.8) | 0.045 |
| Current smoking | 99 (55.3) | 42 (54.5) | 57 (55.9) | 0.88 |
| Family history of CAD | 140 (78.2) | 62 (80.5) | 78 (76.5) | 0.585 |
| Clinical CAD | 179 (100) | 77 (100) | 102 (100) | 1.0 |
| Congestive heart failure | 133 (74.3) | 60 (77.9) | 73 (71.6) | 0.389 |
| Septicemia | 50 (27.9) | 18 (23.3) | 32 (31.4) | 0.313 |
| Sepsis | 101 (56.4) | 54 (70.1) | 47 (46.1) | 0.0014 |
| Severe sepsis | 26 (14.5) | 7 (9.1) | 19 (18.6) | 0.088 |
CAD, coronary artery disease.
Baseline characteristics of 179 patients with type 2 diabetes undergoing surgery for lower limb amputation.
| Variable, n (%) . | Total (n = 179) . | Compliant (n = 77) . | Non-compliant (n = 102) . | p-value . |
|---|---|---|---|---|
| Age, years | 60.4 ± 8.8 | 58.9 ± 10.1 | 60.3 ± 8.5 | 0.316 |
| Gender, n (%) | ||||
| Male | 109 (60.9) | 46 (59.7) | 63 (61.8) | 0.877 |
| Female | 70 (39.1) | 31 (40.3) | 39 (38.2) | |
| Arterial hypertension | 161 (89.9) | 70 (90.9) | 91 (89.2) | 0.805 |
| Arterial hypotension (Systolic ˂90 mmHg) | 18 (10.3) | 7 (9.1) | 11 (10.8) | 0.805 |
| Obese | 93 (52) | 39 (50.6) | 54 (52.9) | 1.0 |
| Dyslipidemia | 179 (100) | 77 (100) | 102 (100) | 1.0 |
| Previous statin use | 30 (16.7) | 18 (23.4) | 12 (11.8) | 0.045 |
| Current smoking | 99 (55.3) | 42 (54.5) | 57 (55.9) | 0.88 |
| Family history of CAD | 140 (78.2) | 62 (80.5) | 78 (76.5) | 0.585 |
| Clinical CAD | 179 (100) | 77 (100) | 102 (100) | 1.0 |
| Congestive heart failure | 133 (74.3) | 60 (77.9) | 73 (71.6) | 0.389 |
| Septicemia | 50 (27.9) | 18 (23.3) | 32 (31.4) | 0.313 |
| Sepsis | 101 (56.4) | 54 (70.1) | 47 (46.1) | 0.0014 |
| Severe sepsis | 26 (14.5) | 7 (9.1) | 19 (18.6) | 0.088 |
| Variable, n (%) . | Total (n = 179) . | Compliant (n = 77) . | Non-compliant (n = 102) . | p-value . |
|---|---|---|---|---|
| Age, years | 60.4 ± 8.8 | 58.9 ± 10.1 | 60.3 ± 8.5 | 0.316 |
| Gender, n (%) | ||||
| Male | 109 (60.9) | 46 (59.7) | 63 (61.8) | 0.877 |
| Female | 70 (39.1) | 31 (40.3) | 39 (38.2) | |
| Arterial hypertension | 161 (89.9) | 70 (90.9) | 91 (89.2) | 0.805 |
| Arterial hypotension (Systolic ˂90 mmHg) | 18 (10.3) | 7 (9.1) | 11 (10.8) | 0.805 |
| Obese | 93 (52) | 39 (50.6) | 54 (52.9) | 1.0 |
| Dyslipidemia | 179 (100) | 77 (100) | 102 (100) | 1.0 |
| Previous statin use | 30 (16.7) | 18 (23.4) | 12 (11.8) | 0.045 |
| Current smoking | 99 (55.3) | 42 (54.5) | 57 (55.9) | 0.88 |
| Family history of CAD | 140 (78.2) | 62 (80.5) | 78 (76.5) | 0.585 |
| Clinical CAD | 179 (100) | 77 (100) | 102 (100) | 1.0 |
| Congestive heart failure | 133 (74.3) | 60 (77.9) | 73 (71.6) | 0.389 |
| Septicemia | 50 (27.9) | 18 (23.3) | 32 (31.4) | 0.313 |
| Sepsis | 101 (56.4) | 54 (70.1) | 47 (46.1) | 0.0014 |
| Severe sepsis | 26 (14.5) | 7 (9.1) | 19 (18.6) | 0.088 |
CAD, coronary artery disease.
Within 24 hours of admission, we followed a specific protocol for patient preparation for surgery, including normalization of arterial and central venous pressure, adequate diuresis, electrolyte and acid–base balance and body temperature. We provided intravenous fluids, antibacterial and antifungal drugs, insulin and anticoagulant therapy, which were free of charge for patients. We immediately prescribed medication, including atorvastatin 80 mg daily (starting preoperatively), clopidogrel 1st day 300 mg, then 75 mg daily, antihypertensive, anti-ischemic drugs and heart failure treatment if required; aspirin 75 mg daily started 3–5 days after amputation for continuous use (minimum 1 year). A total of 143 patients (79.9%) spent only 1 day in the intensive care unit, 36 patients (20.1%) required 2 or more days after operation. There were no deaths during or within 4 days of operation. We tried to activate patients as early as possible to prevent thromboembolic complications (movement of stump, rotation in bed, sitting, breathing exercises, medical gymnastics and later walking on crutches).
During inpatient treatment and over the whole study period 77 patients (43%) were compliant. They followed a diet as prescribed, stopped smoking (if smoker), increased PA to ≥30 min/day, and had >90% drug intake (diabetic medications including insulin dosage adaptions, antihypertensive drugs, dual antiplatelet and statin treatment), instead of 80% cut point during inpatient treatment and 1-year follow up.
A total of 102 patients (57%) did not follow the prescribed regimen and were identified as non-compliant. Every patient in this group had <70% drug adherence (mostly related to statin and dual antiplatelet treatment, and some with antihypertensive drugs). Nobody in the non-compliance group who smoked before surgery quit smoking. A total of 86 patients (84.3%) had records of diet violation inquiring increased dosages of insulin. Most of patients did not follow recommendations of regular PA. However, all patients used insulin in prescribed time and dose. Arterial pressure measured at examination days was mostly within required limits.
Due to medication intake for non-compliant patients, forgetfulness was the most commonly cited reason in 58 patients (56.8%); lack of financial support to buy medicaments was cited by 42 patients (41.2%). Reluctance to take medication for a long time was cited in nine cases (8.8%). Six patients (5.9%) had serious psychical problems (severe depression), and they did not wish to live with disability after TFA; 11 patients (10.8%) had wrong beliefs about treatment (harmful, not necessary). Almost all patients had difficulties with the complexity of medication regime. Adverse effects related to stopping drug intake were recorded in 12 patients (11.8%). Among them, five patients stopped atorvastatin and clopidogrel because of severe stomach pain, nausea and vomiting, six had gastrointestinal bleeding, one patient had severe liver damage (alcohol abuse history). Almost all patients in both groups after TFA suffered from lower limbs/muscle pain (28/179 had phantom pain) which was relieved by non-steroidal anti-inflammatory drugs. There were no detected cases of rhabdomyolysis, or stopping statins because of muscle pain.
At 1-year follow-up, Fuster-BEWAT score was significantly higher in the compliant (9.83 ± 3.12; n = 75) versus the non-compliant group (7.74 ± 2.9; n = 76). The mean difference between both groups was 2.09 with a 95% confidence interval (CI) ranging from 1.1248 to 3.0552, p = 0.0001. The increase in the overall score from baseline was greater in compliant compared with non-compliant patients (p = 0.0001). The most significant difference was found for lower smoking cessation rates in the non-compliant group. BP decreased and PA increased in the non-compliant patients (p = 0.0001), therefore contributing to a lesser increase of the Fuster-BEWAT score (Table 2).
Fuster-BEWAT score in patients with type 2 diabetes at baseline and in 1 year after trans-femoral amputation.
| Criteria . | Compliant . | p-value . | Non-compliant . | p-value . | ||
|---|---|---|---|---|---|---|
| Baseline (n = 77) . | 1 year (n = 75) . | Baseline (n = 102) . | 1 year (n = 76) . | |||
| Blood pressure | 0.67 ± 0.88 | 1.65 ± 0.91 | 0.0001 | 0.83 ± 0.89 | 1.95 ± 1.09 | 0.0001 |
| Exercise | 0 | 1.97 ± 0.72 | 0.0001 | 0 | 0.73 ± 0.77 | 0.0001 |
| Weight | 0.84 ± 1.0 | 1.12 ± 1.04 | 0.0927 | 0.83 ± 0.99 | 1.01 ± 1.05 | 0.2439 |
| Alimentation | 2.17 ± 0.8 | 2.21 ± 0.78 | 0.7555 | 2.19 ± 0.76 | 2.09 ± 0.72 | 0.3758 |
| Tobacco | 1.65 ± 1.29 | 2.88 ± 0.32 | 0.0001 | 1.63 ± 1.28 | 1.96 ± 1.17 | 0.0794 |
| Total Score | 5.33 ± 2.73 | 9.83 ± 3.12 | 0.0001 | 5.48 ± 2.9 | 7.74 ± 2.9 | 0.0001 |
| Criteria . | Compliant . | p-value . | Non-compliant . | p-value . | ||
|---|---|---|---|---|---|---|
| Baseline (n = 77) . | 1 year (n = 75) . | Baseline (n = 102) . | 1 year (n = 76) . | |||
| Blood pressure | 0.67 ± 0.88 | 1.65 ± 0.91 | 0.0001 | 0.83 ± 0.89 | 1.95 ± 1.09 | 0.0001 |
| Exercise | 0 | 1.97 ± 0.72 | 0.0001 | 0 | 0.73 ± 0.77 | 0.0001 |
| Weight | 0.84 ± 1.0 | 1.12 ± 1.04 | 0.0927 | 0.83 ± 0.99 | 1.01 ± 1.05 | 0.2439 |
| Alimentation | 2.17 ± 0.8 | 2.21 ± 0.78 | 0.7555 | 2.19 ± 0.76 | 2.09 ± 0.72 | 0.3758 |
| Tobacco | 1.65 ± 1.29 | 2.88 ± 0.32 | 0.0001 | 1.63 ± 1.28 | 1.96 ± 1.17 | 0.0794 |
| Total Score | 5.33 ± 2.73 | 9.83 ± 3.12 | 0.0001 | 5.48 ± 2.9 | 7.74 ± 2.9 | 0.0001 |
Fuster-BEWAT score in patients with type 2 diabetes at baseline and in 1 year after trans-femoral amputation.
| Criteria . | Compliant . | p-value . | Non-compliant . | p-value . | ||
|---|---|---|---|---|---|---|
| Baseline (n = 77) . | 1 year (n = 75) . | Baseline (n = 102) . | 1 year (n = 76) . | |||
| Blood pressure | 0.67 ± 0.88 | 1.65 ± 0.91 | 0.0001 | 0.83 ± 0.89 | 1.95 ± 1.09 | 0.0001 |
| Exercise | 0 | 1.97 ± 0.72 | 0.0001 | 0 | 0.73 ± 0.77 | 0.0001 |
| Weight | 0.84 ± 1.0 | 1.12 ± 1.04 | 0.0927 | 0.83 ± 0.99 | 1.01 ± 1.05 | 0.2439 |
| Alimentation | 2.17 ± 0.8 | 2.21 ± 0.78 | 0.7555 | 2.19 ± 0.76 | 2.09 ± 0.72 | 0.3758 |
| Tobacco | 1.65 ± 1.29 | 2.88 ± 0.32 | 0.0001 | 1.63 ± 1.28 | 1.96 ± 1.17 | 0.0794 |
| Total Score | 5.33 ± 2.73 | 9.83 ± 3.12 | 0.0001 | 5.48 ± 2.9 | 7.74 ± 2.9 | 0.0001 |
| Criteria . | Compliant . | p-value . | Non-compliant . | p-value . | ||
|---|---|---|---|---|---|---|
| Baseline (n = 77) . | 1 year (n = 75) . | Baseline (n = 102) . | 1 year (n = 76) . | |||
| Blood pressure | 0.67 ± 0.88 | 1.65 ± 0.91 | 0.0001 | 0.83 ± 0.89 | 1.95 ± 1.09 | 0.0001 |
| Exercise | 0 | 1.97 ± 0.72 | 0.0001 | 0 | 0.73 ± 0.77 | 0.0001 |
| Weight | 0.84 ± 1.0 | 1.12 ± 1.04 | 0.0927 | 0.83 ± 0.99 | 1.01 ± 1.05 | 0.2439 |
| Alimentation | 2.17 ± 0.8 | 2.21 ± 0.78 | 0.7555 | 2.19 ± 0.76 | 2.09 ± 0.72 | 0.3758 |
| Tobacco | 1.65 ± 1.29 | 2.88 ± 0.32 | 0.0001 | 1.63 ± 1.28 | 1.96 ± 1.17 | 0.0794 |
| Total Score | 5.33 ± 2.73 | 9.83 ± 3.12 | 0.0001 | 5.48 ± 2.9 | 7.74 ± 2.9 | 0.0001 |
In the compliant group, TC level decreased during follow-up with a maximal dose of 80 mg atorvastatin from 10.8 ± 2.7 to 5.8 ± 0.5 µmol/l (95% CI 4.374–5.626, p = 0.0001). A reduction of LDL-C of ≥50% was found in 71/77 (92.2%) of the compliant patients (p = 0.0001). In non-compliant patients, TC decreased also significantly from 10.9 ± 2.5 to 7.9 ± 1.7 µmol/l (95% CI 2.587–3.813, p = 0.0001), although the majority of these patients did not regularly follow prescribed treatment.
At 1-year follow-up, there were 43 MIs in total, 40 of them (93%) in non-compliant patients, and 28 death in total, 26 of them (92.8%) in non-compliant patients (Table 3). Absolute risk reduction (ARR) for MI in the compliant versus non-compliant group was 35.3% (95% CI for this difference 24.9–45.7%). ARR for cardiovascular death was 22.9% (95% CI 13.7–32.1%). There was no statistically significant difference in the incidence of ischemic stroke with an ARR of 4.9% (95% CI 0.7–9.1%, p = 0.0712). ARR for fatal pulmonary embolism was 9.8% (95% CI 4.0–15.6%).
Clinical outcomes during 1-year postoperative period in 179 patients with type 2 diabetes after trans-femoral amputation of one lower limb.
| Clinical outcomes, n (%) . | Compliant (n = 77) . | Non-compliant (n = 102) . | p-value . |
|---|---|---|---|
| 10 days postoperative mortality | − | 10 (9.8%) | 0.0054 |
| 1 year postoperative mortality | 2 (2.6%) | 26 (25.5%) | 0.0001 |
| 10 days postoperative MI | 3 (3.9%) | 16 (15.6%) | 0.0133 |
| Total 1-year MI | 3 (3.9%) | 40 (39.2%) | 0.0001 |
| Fatal myocardial infarction | − | 13 (12.7%) | 0.0007 |
| Fatal acute cardiovascular insufficiency | 1 (1.3%) | 12 (11.8%) | 0.0076 |
| Ischemic stroke | − | 5 (4.9%) | 0.0712 |
| Fatal ischemic stroke | − | 3 (2.9%) | 0.2605 |
| Fatal pulmonary embolism | − | 10 (9.8%) | 0.0054 |
| Fatal hypoglycemic coma | 1 (1.3%) | − | 0.4302 |
| Gastrointestinal bleeding | 1 (1.3%) | 6 (5.9%) | 0.0712 |
| Surgical complications of previously amputated lower extremity | |||
| Thrombosis of stump with hip disarticulation | 1 (1.3%) | 3 (2.9%) | 0.6356 |
| Surgical complications of previously intact lower extremity | |||
| Balloon angioplasty of single lower limb artery(s) | 17 (22.1%) | 24 (23.5%) | 0.8591 |
| Amputation of one or two toes | 2 (2.6%) | 16 (15.7%) | 0.046 |
| Partial foot amputation | 1 (1.3%) | 10 (9.8%) | 0.025 |
| Metatarsal amputation | 2 (2.6%) | 7 (6.9%) | 0.3035 |
| Single lower limb hip amputation | 1 (1.3%) | 3 (2.9%) | 0.6356 |
| Disarticulation of amputated hip | 1 (1.3%) | 3 (2.9%) | 0.6356 |
| Clinical outcomes, n (%) . | Compliant (n = 77) . | Non-compliant (n = 102) . | p-value . |
|---|---|---|---|
| 10 days postoperative mortality | − | 10 (9.8%) | 0.0054 |
| 1 year postoperative mortality | 2 (2.6%) | 26 (25.5%) | 0.0001 |
| 10 days postoperative MI | 3 (3.9%) | 16 (15.6%) | 0.0133 |
| Total 1-year MI | 3 (3.9%) | 40 (39.2%) | 0.0001 |
| Fatal myocardial infarction | − | 13 (12.7%) | 0.0007 |
| Fatal acute cardiovascular insufficiency | 1 (1.3%) | 12 (11.8%) | 0.0076 |
| Ischemic stroke | − | 5 (4.9%) | 0.0712 |
| Fatal ischemic stroke | − | 3 (2.9%) | 0.2605 |
| Fatal pulmonary embolism | − | 10 (9.8%) | 0.0054 |
| Fatal hypoglycemic coma | 1 (1.3%) | − | 0.4302 |
| Gastrointestinal bleeding | 1 (1.3%) | 6 (5.9%) | 0.0712 |
| Surgical complications of previously amputated lower extremity | |||
| Thrombosis of stump with hip disarticulation | 1 (1.3%) | 3 (2.9%) | 0.6356 |
| Surgical complications of previously intact lower extremity | |||
| Balloon angioplasty of single lower limb artery(s) | 17 (22.1%) | 24 (23.5%) | 0.8591 |
| Amputation of one or two toes | 2 (2.6%) | 16 (15.7%) | 0.046 |
| Partial foot amputation | 1 (1.3%) | 10 (9.8%) | 0.025 |
| Metatarsal amputation | 2 (2.6%) | 7 (6.9%) | 0.3035 |
| Single lower limb hip amputation | 1 (1.3%) | 3 (2.9%) | 0.6356 |
| Disarticulation of amputated hip | 1 (1.3%) | 3 (2.9%) | 0.6356 |
MI, myocardial infarction.
Clinical outcomes during 1-year postoperative period in 179 patients with type 2 diabetes after trans-femoral amputation of one lower limb.
| Clinical outcomes, n (%) . | Compliant (n = 77) . | Non-compliant (n = 102) . | p-value . |
|---|---|---|---|
| 10 days postoperative mortality | − | 10 (9.8%) | 0.0054 |
| 1 year postoperative mortality | 2 (2.6%) | 26 (25.5%) | 0.0001 |
| 10 days postoperative MI | 3 (3.9%) | 16 (15.6%) | 0.0133 |
| Total 1-year MI | 3 (3.9%) | 40 (39.2%) | 0.0001 |
| Fatal myocardial infarction | − | 13 (12.7%) | 0.0007 |
| Fatal acute cardiovascular insufficiency | 1 (1.3%) | 12 (11.8%) | 0.0076 |
| Ischemic stroke | − | 5 (4.9%) | 0.0712 |
| Fatal ischemic stroke | − | 3 (2.9%) | 0.2605 |
| Fatal pulmonary embolism | − | 10 (9.8%) | 0.0054 |
| Fatal hypoglycemic coma | 1 (1.3%) | − | 0.4302 |
| Gastrointestinal bleeding | 1 (1.3%) | 6 (5.9%) | 0.0712 |
| Surgical complications of previously amputated lower extremity | |||
| Thrombosis of stump with hip disarticulation | 1 (1.3%) | 3 (2.9%) | 0.6356 |
| Surgical complications of previously intact lower extremity | |||
| Balloon angioplasty of single lower limb artery(s) | 17 (22.1%) | 24 (23.5%) | 0.8591 |
| Amputation of one or two toes | 2 (2.6%) | 16 (15.7%) | 0.046 |
| Partial foot amputation | 1 (1.3%) | 10 (9.8%) | 0.025 |
| Metatarsal amputation | 2 (2.6%) | 7 (6.9%) | 0.3035 |
| Single lower limb hip amputation | 1 (1.3%) | 3 (2.9%) | 0.6356 |
| Disarticulation of amputated hip | 1 (1.3%) | 3 (2.9%) | 0.6356 |
| Clinical outcomes, n (%) . | Compliant (n = 77) . | Non-compliant (n = 102) . | p-value . |
|---|---|---|---|
| 10 days postoperative mortality | − | 10 (9.8%) | 0.0054 |
| 1 year postoperative mortality | 2 (2.6%) | 26 (25.5%) | 0.0001 |
| 10 days postoperative MI | 3 (3.9%) | 16 (15.6%) | 0.0133 |
| Total 1-year MI | 3 (3.9%) | 40 (39.2%) | 0.0001 |
| Fatal myocardial infarction | − | 13 (12.7%) | 0.0007 |
| Fatal acute cardiovascular insufficiency | 1 (1.3%) | 12 (11.8%) | 0.0076 |
| Ischemic stroke | − | 5 (4.9%) | 0.0712 |
| Fatal ischemic stroke | − | 3 (2.9%) | 0.2605 |
| Fatal pulmonary embolism | − | 10 (9.8%) | 0.0054 |
| Fatal hypoglycemic coma | 1 (1.3%) | − | 0.4302 |
| Gastrointestinal bleeding | 1 (1.3%) | 6 (5.9%) | 0.0712 |
| Surgical complications of previously amputated lower extremity | |||
| Thrombosis of stump with hip disarticulation | 1 (1.3%) | 3 (2.9%) | 0.6356 |
| Surgical complications of previously intact lower extremity | |||
| Balloon angioplasty of single lower limb artery(s) | 17 (22.1%) | 24 (23.5%) | 0.8591 |
| Amputation of one or two toes | 2 (2.6%) | 16 (15.7%) | 0.046 |
| Partial foot amputation | 1 (1.3%) | 10 (9.8%) | 0.025 |
| Metatarsal amputation | 2 (2.6%) | 7 (6.9%) | 0.3035 |
| Single lower limb hip amputation | 1 (1.3%) | 3 (2.9%) | 0.6356 |
| Disarticulation of amputated hip | 1 (1.3%) | 3 (2.9%) | 0.6356 |
MI, myocardial infarction.
CCTA and CACS findings and MACE rate at 1-year follow-up are shown in Table 4. During the study period, three incidences of non-fatal MI were detected in non-compliant patients with non-obstructive CAD. Patients with three- and two-vessel obstructive stenosis had higher 1-year MACE rate than those with 1-vessel obstructive and non-obstructive CAD, and more proximal coronary lesions were related to a worth prognosis. Non-compliant patients with two- and three-vessel obstructive CAD had sixfold increased incidence of MACE compared with compliant patients. Higher CACS correlated with increased risk of MACE during 1-year follow-up (Table 4). After TFA we directed patients for cardiac revascularization surgery in different Centers of our Republic, but none of 179 patients did aortal bypass grafting or cardiac vessels stenting during 1-year follow-up.
CCTA and CACS findings and MACE rate in patients with type 2 diabetes at 1-year follow-up after trans-femoral amputation.
| Number of events/Number of total patients (event rate %) . | Total (n = 179) . | Compliant (n = 77) . | Non-compliant (n = 102) . |
|---|---|---|---|
| No CAD | 0/7 (0%) | 0/4 (0%) | 0/3 (0%) |
| Non-obstructive CAD | 3/46 (6.5%) | 0/11 (0%) | 3/35 (8.6%) |
| 1-vessel obstructive CAD | 6/57 (10.5%) | 0/36 (0%) | 6/21 (28.7%) |
| 2-vessel obstructive CAD | 14/41 (34.1%) | 1/17 (5.9%) | 13/24 (54.2%) |
| 3-vessel obstructive CAD | 20/28 (71.4%) | 2/9 (22.2%) | 18/19 (94.7%) |
| CACS = 0 | 0/6 (0%) | 0/3 (0%) | 0/3 (0%) |
| CACS 1–99 | 2/20 (10%) | 0/7 (0%) | 2/13 (15.4%) |
| CACS 100–399 | 6/44 (13.6%) | 0/19 (0%) | 6/25 (24%) |
| CACS 400–999 | 14/84 (16.6%) | 1/43 (2.3%) | 13/41 (31.7%) |
| CACS > 1000 | 21/25 (84%) | 2/5 (40%) | 19/20 (95%) |
| Number of events/Number of total patients (event rate %) . | Total (n = 179) . | Compliant (n = 77) . | Non-compliant (n = 102) . |
|---|---|---|---|
| No CAD | 0/7 (0%) | 0/4 (0%) | 0/3 (0%) |
| Non-obstructive CAD | 3/46 (6.5%) | 0/11 (0%) | 3/35 (8.6%) |
| 1-vessel obstructive CAD | 6/57 (10.5%) | 0/36 (0%) | 6/21 (28.7%) |
| 2-vessel obstructive CAD | 14/41 (34.1%) | 1/17 (5.9%) | 13/24 (54.2%) |
| 3-vessel obstructive CAD | 20/28 (71.4%) | 2/9 (22.2%) | 18/19 (94.7%) |
| CACS = 0 | 0/6 (0%) | 0/3 (0%) | 0/3 (0%) |
| CACS 1–99 | 2/20 (10%) | 0/7 (0%) | 2/13 (15.4%) |
| CACS 100–399 | 6/44 (13.6%) | 0/19 (0%) | 6/25 (24%) |
| CACS 400–999 | 14/84 (16.6%) | 1/43 (2.3%) | 13/41 (31.7%) |
| CACS > 1000 | 21/25 (84%) | 2/5 (40%) | 19/20 (95%) |
CAD, coronary artery disease; CACS, coronary artery calcium score.
CCTA and CACS findings and MACE rate in patients with type 2 diabetes at 1-year follow-up after trans-femoral amputation.
| Number of events/Number of total patients (event rate %) . | Total (n = 179) . | Compliant (n = 77) . | Non-compliant (n = 102) . |
|---|---|---|---|
| No CAD | 0/7 (0%) | 0/4 (0%) | 0/3 (0%) |
| Non-obstructive CAD | 3/46 (6.5%) | 0/11 (0%) | 3/35 (8.6%) |
| 1-vessel obstructive CAD | 6/57 (10.5%) | 0/36 (0%) | 6/21 (28.7%) |
| 2-vessel obstructive CAD | 14/41 (34.1%) | 1/17 (5.9%) | 13/24 (54.2%) |
| 3-vessel obstructive CAD | 20/28 (71.4%) | 2/9 (22.2%) | 18/19 (94.7%) |
| CACS = 0 | 0/6 (0%) | 0/3 (0%) | 0/3 (0%) |
| CACS 1–99 | 2/20 (10%) | 0/7 (0%) | 2/13 (15.4%) |
| CACS 100–399 | 6/44 (13.6%) | 0/19 (0%) | 6/25 (24%) |
| CACS 400–999 | 14/84 (16.6%) | 1/43 (2.3%) | 13/41 (31.7%) |
| CACS > 1000 | 21/25 (84%) | 2/5 (40%) | 19/20 (95%) |
| Number of events/Number of total patients (event rate %) . | Total (n = 179) . | Compliant (n = 77) . | Non-compliant (n = 102) . |
|---|---|---|---|
| No CAD | 0/7 (0%) | 0/4 (0%) | 0/3 (0%) |
| Non-obstructive CAD | 3/46 (6.5%) | 0/11 (0%) | 3/35 (8.6%) |
| 1-vessel obstructive CAD | 6/57 (10.5%) | 0/36 (0%) | 6/21 (28.7%) |
| 2-vessel obstructive CAD | 14/41 (34.1%) | 1/17 (5.9%) | 13/24 (54.2%) |
| 3-vessel obstructive CAD | 20/28 (71.4%) | 2/9 (22.2%) | 18/19 (94.7%) |
| CACS = 0 | 0/6 (0%) | 0/3 (0%) | 0/3 (0%) |
| CACS 1–99 | 2/20 (10%) | 0/7 (0%) | 2/13 (15.4%) |
| CACS 100–399 | 6/44 (13.6%) | 0/19 (0%) | 6/25 (24%) |
| CACS 400–999 | 14/84 (16.6%) | 1/43 (2.3%) | 13/41 (31.7%) |
| CACS > 1000 | 21/25 (84%) | 2/5 (40%) | 19/20 (95%) |
CAD, coronary artery disease; CACS, coronary artery calcium score.
We evaluated the prognostic performance of CCTA using a Kaplan–Meier curve analysis. Overall, patients with more severe CCTA stenosis had lower MACE-free survival rates (p < 0.0001), whereas those with normal and non-obstructive CCTA had a significantly higher MACE-free survival rate than patients with 2- and 3-vessels obstructive CAD (Figure 1).
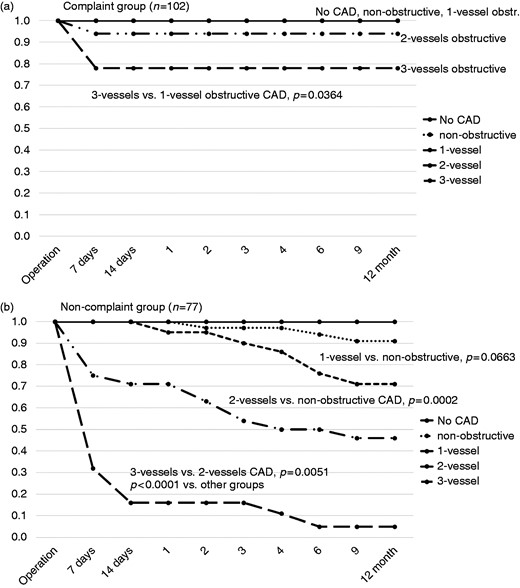
Kaplan–Meier curves for event-free survival from death, fatal and nonfatal myocardial infarction for CCTA in patients with type 2 diabetes undergoing trans-femoral amputation of lower limb. (a) Compliant group. (b) Non-compliant group.
1-, 2- or 3-vessels, number of obstructive coronary arteries; CAD, coronary artery disease.
During 1-year follow-up we found that patients with low compliance had higher incidence of critical ischemia of the remaining lower limb and required amputation of one or two toes or partial foot amputation more often than those who followed prescribed treatment (15.6% versus 2.6%, p = 0.046; and 9.8% versus 1.3%, p = 0.025; respectively) (Table 3).
Discussion
Our study results confirm the particular importance of compliance with secondary prevention interventions including lifestyle changes and medication in T2D patients after TFA representing a population at very high cardiovascular risk. An important finding is the fact that although arterial pressure and blood glucose levels have been found to be reasonably well controlled during regular examinations at our outpatient clinic in compliant as well as in non-compliant patients, the incidence of MACE was much higher in the non-compliant group. This difference can be related to a great extent to non-compliance with double antiplatelet therapy and statin use as well as lifestyle changes including diet, smoking cessation and PA.
The atherogenic dyslipidemia seen in T2D patients is characterized by a complex of elevated serum triglycerides, low HDL-C, preponderance of small dense LDL particles and elevated apoprotein B.18 This certainly contributes to the very high risk for cardiovascular complications in our patients with critical LEAD and CAD [10]. Therefore, it is an important finding that the goal of >50% LDL-C reduction was reached on 80 mg atorvastatin in 92.2% of patients in our compliant group.
Compliance with dual antiplatelet therapy is a major challenge if patients have to pay for it fully or partially by themselves. A combination of aspirin and clopidogrel therapy was associated with a 20% relative risk reduction for MI, stroke, or cardiovascular death in patients with acute coronary syndromes.19 The CHARISMA trial did not show a benefit of combined aspirin and clopidogrel treatment versus aspirin alone in a combined cohort of subjects with established vascular disease and subjects at high risk, although dual antiplatelet therapy was marginally better in subgroup with already established vascular disease.20 The Antiplatelet Trialists’ Collaboration found a 30% reduction in the rate of lower arterial occlusion by aspirin compared with no additional medical intervention.21 In our country, ticagrelor and prasugrel are still not available. However, we used a loading dose of 300 mg and a 75 mg daily dose of clopidogrel plus 75–150 mg aspirin daily on the 3rd–5th day after amputation which showed to significantly decrease the risk of MI, cardiac death, pulmonary embolism with very low risk of bleeding.
Our study patients had several important comorbidities and had to take many drugs for T2D and CAD, and LEAD. Problems with compliance in our study were mostly related to difficulties with the complexity of the medication regime, dosage frequency, forgetfulness, inability to buy medications for continuous use, adverse effects, or combinations of these factors. The percentage of noncompliant patients was similar in both genders in our study, and there was no difference between age groups.
The benefits of smoking cessation have a large evidence base. Stopping smoking after an MI is potentially the most effective of all preventive measures: a systematic review and meta-analysis showed reductions in MIs and in the composite endpoints of death/MI (relative risk 0.57 and 0.74, respectively) compared with continued smoking.10,22 Smoking cessation was also the most important lifestyle change reflected in the Fuster-BEWAT score in our patients. Non-compliant patients had a tenfold increased risk for MACE within 1-year after TFA. Our results underline the importance of recommendations to facilitate behavior changes and the adoption of continuous patterns of a healthy lifestyle, to undertake special efforts for patients’ motivation and commitment and to use principles of effective communication. Furthermore, particular attention has to be given to the fact that lack of coverage of cost for medication is a main driver of non-compliance with treatment and secondary prevention measures.
Study limitations
In this manuscript, we did not include 210/389 diabetic patients with symptomatic CAD (54%) undergoing TFA with diabetic nephropathy, acute coronary syndrome, previous MI or limb amputation. Therefore, interpretation of our results cannot be extended to these patients’ groups. We regularly provided education, information and physical examination support for all patients including those in the non-compliant group; many patients started to follow the treatment regimen and later stopped for different reasons. The study design does not allow any conclusions about the possible benefits of compliance over the longer 1-year period. We did not pay enough attention to the socioeconomic status of patients and family members; educational level, race, societal, individual disparities among patients, behavioral problems and mental health, which could have an impact on patient’s compliance.
Conclusions
Our results show a tenfold decrease of MACE in the compliant versus non-compliant patient group. Compliance initiatives are of upmost importance in particular in high-risk diabetic patients with clinical CAD after limb amputation to decrease the risk of MI, cardiac death, pulmonary embolism and the incidence of gangrene of the remaining single lower extremity, preventing partial foot amputation. Our study underlines the need to further elucidate adequate strategies to improve patients’ long-term adherence to secondary prevention recommendations and the importance of coverage of costs for secondary prevention medication in particular in high-risk patients.
Author contribution
ES, HS and BJ contributed to the conception or design of the work. ES, HS and AS contributed to the acquisition, analysis or interpretation of data for the work. All authors drafted the manuscript. ES and HS critically revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.




Comments