-
PDF
- Split View
-
Views
-
Cite
Cite
Johanna Granström, Pontus Lantz, Matthias Lidin, Maria Wahlström, Carolin Nymark, Perceptions of delay when afflicted by an acute myocardial infarction during the first wave of the COVID-19 pandemic, European Journal of Cardiovascular Nursing, Volume 22, Issue 1, January 2023, Pages 89–97, https://doi.org/10.1093/eurjcn/zvac021
Close - Share Icon Share
Abstract
To describe the perceptions of delay in medical care-seeking, when afflicted by an acute myocardial infarction (AMI) during the first wave of the pandemic.
A qualitative descriptive study with an inductive approach. Fourteen semi-structured interviews were conducted, analysed by qualitative content analysis with a manifest approach. One category and six sub-categories emerged. The decision was reached when the health threat was perceived as critical, which made the earlier thoughts of the pandemic fade away. The risk of infection during medical visits caused fear of contracting the disease. This resulted in hesitation, neglect of symptoms, and avoidance of healthcare visits. Following recommendations from authorities and media about personal responsibility was motivated by fear, affecting the care-seeking.
It appears that the COVID-19 pandemic raised the threshold for deciding to seek medical care when presenting with an AMI. The pandemic led to increased patient delay due to several reasons among which fear of contracting the disease was prominent. The emotion of fear was related to the external threat to one's own health, due to COVID-19, and not fear of symptoms related to an AMI. The media reporting the healthcare system as overloaded increased insecurity and may have had an influence on delay.

The emotion of fear of acquiring COVID-19 at in-hospital settings maybe the main reason to delay the decision to seek medical care.
It is important that healthcare professionals collaborate with the media to spread information that is consistent with the current healthcare capacity during the pandemic.
Introduction
Ischaemic cardiovascular disease is the most common cause of mortality in the world.1 Early contact with the medical healthcare service for diagnosis of symptoms and to receive time-sensitive coronary interventions can be crucial for the patient's prognostic future when afflicted by an acute myocardial infarction (AMI).2 The personal experience of AMI is multifaceted, where the symptom interpretation is often affected by the individual's own experiences.3 Symptoms such as fear and anxiety are common.4,5 Also, symptoms could be difficult to interpret due to underestimation of their severity and may delay the medical care-seeking, which could result in negative prognostic outcomes.6,7 The European Society of Cardiology defines patient delay as the time between symptom start to first medical contact with the healthcare system.2 Age, gender, ethnicity, low education level, chronical disease, and insufficient knowledge are well-known factors influencing increased delay time.8,9 Moreover, perceived inability to act and symptom assessment have a large impact on patient delay.10
In December 2019, the coronavirus SARS-CoV2 (COVID-19) disease was first detected and in November 2021, the disease has affected nearly 260 million persons, resulting in 5 million deaths.11 Risk factors such as older age, male gender, being overweight or obese, and comorbidities such as coronary artery disease and diabetes type II have led to an increased probability for a more severe disease pattern, and thereby an increase in morbidity and mortality.12,13 Media coverage worldwide, with headlines of the COVID-19 pandemic, has had a negative effect on mental health, and the most common reasons for negative stress were reading and hearing about the contagiousness and the seriousness of the disease, the uncertainty about the time limit for quarantine, and demands for social distancing.14,15 In parallel to this a national and international decreased trend of seeking medical care for AMI was observed.16,17 A British study revealed that patient delay was clearly affected by the pandemic, with an increased delay from 119 to 227 min.18 In a preceding recently published study by Lidin et al.,19 individuals with AMI increased their delay, caused by fear of COVID-19, particularly in women and immigrants. This fear was based on thoughts of overcrowded hospitals due to COVID-19 and fear of being infected by the coronavirus at the hospital or in the ambulance.
However, there is a need for more in-depth knowledge of the individual perceptions of the influence of COVID-19 when afflicted by symptoms of AMI to gain a deeper understanding of the individuals’ care-seeking behaviour. This study aimed to describe the perceptions of delay in medical care-seeking when afflicted by an AMI during the first wave of the pandemic.
Methods
Design
This was a qualitative descriptive interview study with an inductive approach conducted by 14 telephone interviews between November and December 2020.
Sample
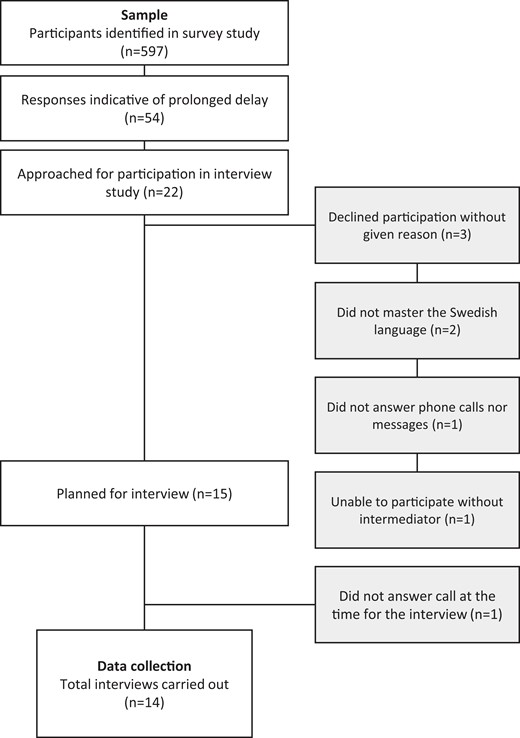
Participants were identified through a previous survey study.19 A total of 597 persons afflicted by an AMI between 1 March and 30 June 2020 were identified through the Swedish national registry (SWEDEHEART), a registry of all patients hospitalized for acute coronary syndromes.20 The participants were selected in the region of Stockholm. They were asked to fill in a psychometric evaluated questionnaire entitled ‘Patients appraisal, emotions, and action tendencies preceding care-seeking in AMI’ (PA-AMI).9 Designed for the study, additional questions were asked regarding care-seeking due to COVID-19. The main question was ‘Would you have sought medical care earlier if the COVID-19 pandemic had not occurred?’ As an inclusion criterion in the present study, the participants who, through their answers, indicated an increased delay due to the COVID-19 pandemic were contacted by phone and asked to participate. The participants had to be able to speak Swedish and be able to participate without any kind of intermediary. By criterion sampling, a total of 22 participants were approached, 15 men and 7 women, and a broad in age and sex was sought (Figure 1).
Data collection
The data collection was carried out by two of the main authors (P.L. and J.G.) using semi-structured individual interviews. An interview guide was used with open-ended questions for the purpose of focusing on the subject whilst still allowing the participants to freely describe their experience of the event. The interview guide consisted of questions where the participant was asked for example to elaborate on their perceptions when presenting with an AMI, from symptom onset to the decision to seek medical care and action when they sought medical care and transport to the hospital. The opening question was ‘Can you tell me briefly about when you sought medical care for your AMI?’ With follow up questions such as ‘What made you decide to seek medical care?’ and ‘Would you have sought medical care earlier if the COVID-19 pandemic had not existed?’.
Initially, four pilot interviews were conducted at which both main authors attended to ensure that the subsequent interviews would be performed using a similar interview technique. The pilot interviews were included in the analysis. Participants were enrolled as the interviews continued until saturation was achieved (similar descriptions of the phenomenon occurred).21 Additionally, two more interviews were conducted to ensure saturation, providing a total of 14 interviews.
The interviews were carried out over the phone and were voice-recorded. At the time, interviews by phone were considered preferable to interviews in person due to restrictions associated with the ongoing COVID-19 pandemic.22 Video interviews were considered, but due to technical issues, were not performed. The interviews lasted 7–36 min (mean 20 ± 9 min).
Data analysis
The interviews were analysed using qualitative content analysis with a manifest approach.23 The recorded interviews were transcribed verbatim by the author who performed the interview. The transcripts were then read simultaneously whilst listening to the recordings to ensure coherence.
The identification, condensation, and coding of the meaning units were done by the main authors individually. The meaning units were condensed without altering their content or context. The condensed meaning units were coded and grouped together based on similarities and differences, forming sub-categories. The initial coding and sub-categorization outlined by the main authors were further discussed between all the authors, who all had access to the interview transcripts for reference. When processing the sub-categories, a common thread was identified, and a category was formed. Discussions were held throughout the entire process where the codes, sub-categories, and the category were revised several times before consensus was reached.
Ethics
The study was carried out in accordance with the principles outlined in the 1964 Declaration of Helsinki.24 The study was approved by the Swedish Ethical Review Authority (2020-03785). The participants received written information about the study in advance of the interview by mail, and verbal information when they were contacted by phone and asked to participate, as well as at the time of the interview. The study information emphasized voluntary participation and confidentiality. The transcribed interviews were provided with a participant-specific code number. The first authors as well as the responsible author (C.N.) and author (M.L.) had access to the identifying code list.
Results
Six sub-categories and one category emerged, describing how the COVID-19 pandemic raised the threshold for deciding to seek medical care (Table 1). When perceiving symptoms of an AMI, the pandemic affected the participants’ care-seeking process. These experiences were in some cases described clearly, where the participants gave a rich picture of how the pandemic had an influence on their care-seeking, whereas others had difficulty in describing these experiences in depth. In both cases, personal interpretations, decision-making processes, and subsequent actions were affected, and the participants’ thoughts about COVID-19 were described as being in the back of their minds. The participants’ characteristics are shown in Table 2.
Sub-categories and examples of meaning units, condensed meaning units, and codes of the category ‘the COVID-19 pandemic raised the threshold for deciding to seek medical care’
| Meaning units . | Condensed meaning units . | Codes . | Sub-categories . |
|---|---|---|---|
| You didn't know much then, it felt as you were a little bit scared though… you had high blood pressure, age was not on your side, you were not in good condition, obesity… and… very overweight… so, you were a little bit worried, you didn't know how it worked… so//I kept away as much as possible, I didn't want to go there [to the emergency room]… | Being scared. Having high blood pressure, older age, no good condition, and obesity. Being worried and keeping away from healthcare | Fear of exposure Risk factors and exposure | The influence of the risk of exposure |
| You were a little bit afraid//so I kept away//I had a medical appointment checking my blood pressure which I cancelled because of… I didn't feel to be in the waiting room, because of the risk… we work for the government, so we had to follow recommendations since the beginning of March | Being afraid, keeping away | General recommendations (from work) | Following recommendations |
| Medical appointment was cancelled due to the risk of exposure and due to follow recommendations | |||
| I thought it was a sort of COVID-thing and I thought it was odd that I didn't have fever and then I didn't need to go to the hospital ond uhm… be in the hospital unnecessarily | Thought it was COVID with no fever, and no need to go to the hospital | Symptoms as COVID-19 | Perceiving symptoms as COVID-19 |
| I think most of all that, I had a picture that it was enormously overloaded in the health care system//… there would be crowds and [I] would be there with a lot of poor people being super sick, I felt they [health professionals] had a lot to do anyway… they didn't need me there too… | Picture of the overloaded healthcare system with crowds of very sick people | Overloaded healthcare | The media's influence |
| My wife is a physiotherapist//So, I had a well-qualified person that said to me that no we should not… take the risk or burden, the health care system, but instead wait for a while | The wife (physiotherapist) said not to burden the healthcare | Advice to wait | The influence of significant others |
| When I was there, with that pain, I could barely make it, I was nearly fainting. Then you didn't think of COVID | I could not barely make the pain and didn't think of COVID | The symptoms were superior | The decision to seek medical care |
| Meaning units . | Condensed meaning units . | Codes . | Sub-categories . |
|---|---|---|---|
| You didn't know much then, it felt as you were a little bit scared though… you had high blood pressure, age was not on your side, you were not in good condition, obesity… and… very overweight… so, you were a little bit worried, you didn't know how it worked… so//I kept away as much as possible, I didn't want to go there [to the emergency room]… | Being scared. Having high blood pressure, older age, no good condition, and obesity. Being worried and keeping away from healthcare | Fear of exposure Risk factors and exposure | The influence of the risk of exposure |
| You were a little bit afraid//so I kept away//I had a medical appointment checking my blood pressure which I cancelled because of… I didn't feel to be in the waiting room, because of the risk… we work for the government, so we had to follow recommendations since the beginning of March | Being afraid, keeping away | General recommendations (from work) | Following recommendations |
| Medical appointment was cancelled due to the risk of exposure and due to follow recommendations | |||
| I thought it was a sort of COVID-thing and I thought it was odd that I didn't have fever and then I didn't need to go to the hospital ond uhm… be in the hospital unnecessarily | Thought it was COVID with no fever, and no need to go to the hospital | Symptoms as COVID-19 | Perceiving symptoms as COVID-19 |
| I think most of all that, I had a picture that it was enormously overloaded in the health care system//… there would be crowds and [I] would be there with a lot of poor people being super sick, I felt they [health professionals] had a lot to do anyway… they didn't need me there too… | Picture of the overloaded healthcare system with crowds of very sick people | Overloaded healthcare | The media's influence |
| My wife is a physiotherapist//So, I had a well-qualified person that said to me that no we should not… take the risk or burden, the health care system, but instead wait for a while | The wife (physiotherapist) said not to burden the healthcare | Advice to wait | The influence of significant others |
| When I was there, with that pain, I could barely make it, I was nearly fainting. Then you didn't think of COVID | I could not barely make the pain and didn't think of COVID | The symptoms were superior | The decision to seek medical care |
Sub-categories and examples of meaning units, condensed meaning units, and codes of the category ‘the COVID-19 pandemic raised the threshold for deciding to seek medical care’
| Meaning units . | Condensed meaning units . | Codes . | Sub-categories . |
|---|---|---|---|
| You didn't know much then, it felt as you were a little bit scared though… you had high blood pressure, age was not on your side, you were not in good condition, obesity… and… very overweight… so, you were a little bit worried, you didn't know how it worked… so//I kept away as much as possible, I didn't want to go there [to the emergency room]… | Being scared. Having high blood pressure, older age, no good condition, and obesity. Being worried and keeping away from healthcare | Fear of exposure Risk factors and exposure | The influence of the risk of exposure |
| You were a little bit afraid//so I kept away//I had a medical appointment checking my blood pressure which I cancelled because of… I didn't feel to be in the waiting room, because of the risk… we work for the government, so we had to follow recommendations since the beginning of March | Being afraid, keeping away | General recommendations (from work) | Following recommendations |
| Medical appointment was cancelled due to the risk of exposure and due to follow recommendations | |||
| I thought it was a sort of COVID-thing and I thought it was odd that I didn't have fever and then I didn't need to go to the hospital ond uhm… be in the hospital unnecessarily | Thought it was COVID with no fever, and no need to go to the hospital | Symptoms as COVID-19 | Perceiving symptoms as COVID-19 |
| I think most of all that, I had a picture that it was enormously overloaded in the health care system//… there would be crowds and [I] would be there with a lot of poor people being super sick, I felt they [health professionals] had a lot to do anyway… they didn't need me there too… | Picture of the overloaded healthcare system with crowds of very sick people | Overloaded healthcare | The media's influence |
| My wife is a physiotherapist//So, I had a well-qualified person that said to me that no we should not… take the risk or burden, the health care system, but instead wait for a while | The wife (physiotherapist) said not to burden the healthcare | Advice to wait | The influence of significant others |
| When I was there, with that pain, I could barely make it, I was nearly fainting. Then you didn't think of COVID | I could not barely make the pain and didn't think of COVID | The symptoms were superior | The decision to seek medical care |
| Meaning units . | Condensed meaning units . | Codes . | Sub-categories . |
|---|---|---|---|
| You didn't know much then, it felt as you were a little bit scared though… you had high blood pressure, age was not on your side, you were not in good condition, obesity… and… very overweight… so, you were a little bit worried, you didn't know how it worked… so//I kept away as much as possible, I didn't want to go there [to the emergency room]… | Being scared. Having high blood pressure, older age, no good condition, and obesity. Being worried and keeping away from healthcare | Fear of exposure Risk factors and exposure | The influence of the risk of exposure |
| You were a little bit afraid//so I kept away//I had a medical appointment checking my blood pressure which I cancelled because of… I didn't feel to be in the waiting room, because of the risk… we work for the government, so we had to follow recommendations since the beginning of March | Being afraid, keeping away | General recommendations (from work) | Following recommendations |
| Medical appointment was cancelled due to the risk of exposure and due to follow recommendations | |||
| I thought it was a sort of COVID-thing and I thought it was odd that I didn't have fever and then I didn't need to go to the hospital ond uhm… be in the hospital unnecessarily | Thought it was COVID with no fever, and no need to go to the hospital | Symptoms as COVID-19 | Perceiving symptoms as COVID-19 |
| I think most of all that, I had a picture that it was enormously overloaded in the health care system//… there would be crowds and [I] would be there with a lot of poor people being super sick, I felt they [health professionals] had a lot to do anyway… they didn't need me there too… | Picture of the overloaded healthcare system with crowds of very sick people | Overloaded healthcare | The media's influence |
| My wife is a physiotherapist//So, I had a well-qualified person that said to me that no we should not… take the risk or burden, the health care system, but instead wait for a while | The wife (physiotherapist) said not to burden the healthcare | Advice to wait | The influence of significant others |
| When I was there, with that pain, I could barely make it, I was nearly fainting. Then you didn't think of COVID | I could not barely make the pain and didn't think of COVID | The symptoms were superior | The decision to seek medical care |
| Characteristics . | N = 14 . |
|---|---|
| Demographics | |
| Age (years) | |
| ȃMedian (IQR) | 64 (56–71) |
| ȃRange | 51–81 |
| Sex | |
| ȃMale | 12 |
| ȃFemale | 2 |
| Risk factors | |
| ȃDiabetes | 5 |
| ȃHypertension | 9 |
| ȃBody mass index [median (IQR)] | 28.1 (25.5–31.0) |
| ȃCurrently smoking | 3 |
| ȃCeased smoking | 6 |
| ȃNever smoked | 5 |
| History | |
| ȃPrevious AMI | 6 |
| ȃPrevious PCI | 6 |
| AMI classification | |
| ȃSTEMI | 4 |
| ȃNSTEMI | 10 |
| Delay [median (IQR)] | |
| ȃPatient delaya (h) | 3.0 (2.2–66.5) |
| ȃPatient assessed delayb (h) | 44.5 (21.8–96.0) |
| Characteristics . | N = 14 . |
|---|---|
| Demographics | |
| Age (years) | |
| ȃMedian (IQR) | 64 (56–71) |
| ȃRange | 51–81 |
| Sex | |
| ȃMale | 12 |
| ȃFemale | 2 |
| Risk factors | |
| ȃDiabetes | 5 |
| ȃHypertension | 9 |
| ȃBody mass index [median (IQR)] | 28.1 (25.5–31.0) |
| ȃCurrently smoking | 3 |
| ȃCeased smoking | 6 |
| ȃNever smoked | 5 |
| History | |
| ȃPrevious AMI | 6 |
| ȃPrevious PCI | 6 |
| AMI classification | |
| ȃSTEMI | 4 |
| ȃNSTEMI | 10 |
| Delay [median (IQR)] | |
| ȃPatient delaya (h) | 3.0 (2.2–66.5) |
| ȃPatient assessed delayb (h) | 44.5 (21.8–96.0) |
Data collected from SWEDEHEART registry.
Self-assessed delay from PA-AMI questionnaire.
| Characteristics . | N = 14 . |
|---|---|
| Demographics | |
| Age (years) | |
| ȃMedian (IQR) | 64 (56–71) |
| ȃRange | 51–81 |
| Sex | |
| ȃMale | 12 |
| ȃFemale | 2 |
| Risk factors | |
| ȃDiabetes | 5 |
| ȃHypertension | 9 |
| ȃBody mass index [median (IQR)] | 28.1 (25.5–31.0) |
| ȃCurrently smoking | 3 |
| ȃCeased smoking | 6 |
| ȃNever smoked | 5 |
| History | |
| ȃPrevious AMI | 6 |
| ȃPrevious PCI | 6 |
| AMI classification | |
| ȃSTEMI | 4 |
| ȃNSTEMI | 10 |
| Delay [median (IQR)] | |
| ȃPatient delaya (h) | 3.0 (2.2–66.5) |
| ȃPatient assessed delayb (h) | 44.5 (21.8–96.0) |
| Characteristics . | N = 14 . |
|---|---|
| Demographics | |
| Age (years) | |
| ȃMedian (IQR) | 64 (56–71) |
| ȃRange | 51–81 |
| Sex | |
| ȃMale | 12 |
| ȃFemale | 2 |
| Risk factors | |
| ȃDiabetes | 5 |
| ȃHypertension | 9 |
| ȃBody mass index [median (IQR)] | 28.1 (25.5–31.0) |
| ȃCurrently smoking | 3 |
| ȃCeased smoking | 6 |
| ȃNever smoked | 5 |
| History | |
| ȃPrevious AMI | 6 |
| ȃPrevious PCI | 6 |
| AMI classification | |
| ȃSTEMI | 4 |
| ȃNSTEMI | 10 |
| Delay [median (IQR)] | |
| ȃPatient delaya (h) | 3.0 (2.2–66.5) |
| ȃPatient assessed delayb (h) | 44.5 (21.8–96.0) |
Data collected from SWEDEHEART registry.
Self-assessed delay from PA-AMI questionnaire.
The influence of the risk of exposure
The fear of being exposed to COVID-19 overruled the healthcare-seeking, even though the participants did not feel the same as usual.
When the participants thought of seeking medical care for their symptoms, they also considered a possible subsequent stay in hospital. The participants expressed concerns and fears about being exposed to a risk of infection in the healthcare setting, leading to an unwillingness to seek medical care and a delay in doing so. The feelings of fear, anxiety, and uncertainty due to COVID-19 and its severity led to symptoms being neglected and a hope that the symptoms would pass.
Also, the participants said that they cancelled planned healthcare visits such as examinations or follow-ups as they thought there was a high risk of being infected by COVID-19, even if they understood there was a necessity for these, considering their symptoms.… it will pass, you know and then… you didn't dare to go to the hospital//the pandemic had started. (P7)
The participants with risk factors such as hypertension, obesity, and older age stated that these factors strongly contributed to the decision not to seek medical care. Acquiring COVID-19 was thought to be synonymous with a severe course of the disease, which resulted in the avoidance of seeking medical care.
Moreover, beyond the situation-specific fear related to symptoms, becoming ill, and the potential need for hospital care, the participants described a more general fear and even panic relating to being infected by COVID-19, where the infection was equated to a death sentence.You didn't know much then, it felt as you were a little bit scared though… you had high blood pressure, age was not on your side, you were not in good condition, obesity… and… very overweight… so, you were a little bit worried, you didn't know how it worked… so//I kept away as much as possible, I didn't want to go there [to the emergency room]… (P6)
All the time, I had a constant fear of getting infected by COVID-19… I felt panicky about this, praising God every morning when I woke up and I was not in a tube in a respirator at the hospital… because I knew that I was in a super high-risk group. (P12)
Following recommendations
The participants said there was a general recommendation from the Swedish Public Health Agency, government, and community as well as from the participants’ workplaces about personal responsibility, and not to risk being exposed to COVID-19, which affected their care-seeking.
The participants were strongly motivated by fear to follow these recommendations. Also, when they were away from home, they experienced being shaky and cold sweats, which was explained by the fear of being in public places. These feelings were avoided as long as possible, contributing to delay in seeking medical care. Moreover, as prescribed by the authorities, the participants said that as they had not met anyone for a long time; therefore, to suddenly be in public places and exposed to possible infection demanded an effort.
It was because of corona and so… you didn't want to go to places where there were a lot of people//We hadn't met any other people at all since the beginning of March. (P9)
Perceiving symptoms as COVID-19
The participants related their perceived symptoms to the symptoms of COVID-19 such as difficulties breathing and discomfort in the chest. These symptoms could occur for example when exercising but were related to their breathing and therefore understood as COVID-19. Some participants said they had a feeling that it was just a matter of time before they would become ill with COVID-19. Moreover, as they thought that symptoms were related to COVID-19, the lack of fever and a sense of not being critically ill, delayed them from seeking medical care.
I did not understand what it was before that, I had no fever and therefore there was no reason to go to the emergency room considering COVID//I had just been waiting to become ill with COVID. (P4)
The media's influence
There were general perceptions among the participants that the healthcare system was seriously overloaded, which caused worries and insecurity. The media reported that the in-hospital care was overcrowded with patients and therefore it was understood that the healthcare system had reached its maximum capacity and was inaccessible, which contributed to delay among the participants. The consequences of these assumptions were that the participants further re-evaluated their symptoms and judged them not to be serious enough to warrant taking up a hospital bed. Also, they did not want to burden the already overloaded healthcare system or be in an overcrowded waiting room at the emergency room with others that were very sick.
Even if the participants experienced alarming symptoms this was set against the fact that there were others that might need the healthcare system more than themselves. This reasoning could persist for a long time and the participants could find themselves very ill with serious symptoms before these were judged to be untenable and the need to seek medical care became clear. Beyond the assumption that the healthcare system was overloaded and inaccessible, there was a desire not to burden the healthcare services unnecessarily as there were others with a higher need for healthcare resources. This was done through rescheduling pre-arranged healthcare meetings and consequently avoiding seeking medical care.I think most of all that, I had a picture that it was enormously overloaded in the health care system//… there would be crowds and [I] would be there with a lot of poor people being super sick, I felt they [health professionals] had a lot to do anyway… they didn't need me there too… (P13)
You read that it was overloaded with work at the intensive care units, it was overcrowded, the original health care system would not work. Then you didn't want to go to your ordinary health care meetings. There were people who need health care more you thought then; that was my personal opinion anyway. (P6)
The influence of significant others
The significant others were used as talking partners when symptoms were noted, and these discussions could result in a decision to seek medical care or a delay. Usually, the significant others recognized the need to seek medical care at an earlier stage than the participants. Therefore, they persuaded or in another way brought the participants into contact with the healthcare services even if the participants strongly expressed their unwillingness to seek medical care due to the pandemic. This persuasion demanded repeated exhortations, resulting in the participants finally calling the emergency number, or the significant other made the call against the participant's instructions.
The discussions between the participants and significant other could also lead to self-care or advice to delay seeking medical care. The reasons were the fear of being exposed to COVID-19 and/or concerns about an overloaded healthcare system.
My wife is a physiotherapist and has worked as an instruction therapist and stuff, and she is pretty qualified… but she thought, or she wanted to think, that it was a muscle spasm I felt when I had to sit down, and not a heart problem. And that is pretty common… that it is difficult to interpret… in the body between muscles and heart. So, I had a well-qualified person that said to me that no we should not… take the risk or burden, the health care system, but instead wait for a while. (P14)
The decision to seek medical care
When the symptoms were perceived as a serious threat or as a worsening of earlier symptoms, the participants’ thoughts and considerations regarding COVID-19 decreased or disappeared. The fear of COVID-19 was not an obstacle in the acute situation where the symptoms were thought to be unbearable. The symptoms themselves entailed strong worries and/or anxiety that were superior to the fear of COVID-19. The thoughts of COVID-19 faded away and the participants did not care about it to the same extent as before.
When I was there, with that pain, I could barely make it, I was nearly fainting. Then you didn't think of COVID. (P5)
Discussion
This study aimed to describe the perceptions of COVID-19 in medical care-seeking when afflicted by an AMI during the first wave of the pandemic. The findings illustrate the impact COVID-19 had on the care-seeking process where the possibility of infection and perceiving the healthcare system as inaccessible were important reasons for not seeking medical care.
The COVID-19 pandemic was a huge stress-triggering factor in the population in general,14,15 and our participants expressed this view clearly. To experience stress or perceive issues as threatening/dangerous happens when there is no belief in having adequate resources to cope with the triggering factor.25 The participants in our study used avoidance coping strategies such as not seeking medical care and denial, in line with previous studies of patients afflicted by an AMI, and of medical care-seeking when afflicted by an AMI.26,27 However, the avoidance coping strategy was due to the triggering factor, COVID-19, and not to the symptoms per se.
Among the participants in the present study, a main contributing factor to the hesitation in seeking medical care was insecurity following the mass media reports about the healthcare system being overcrowded and overloaded with patients afflicted by COVID-19. There were reports from the media about the intensive care units (ICUs) being overloaded with patients, leading to a public awareness of the burden in the in-hospital settings.28 One speculation about these reports is that when the media described the situation at the ICUs, where the patients with COVID-19 were treated, it might have been difficult for the public to differentiate an ICU from an intensive coronary care unit and also ordinary medical and surgical wards. The general public might have believed the reports about overcrowded ICUs applied to all in-hospital care. In fact, during the first wave of the pandemic, the decline in the number of patients with AMI and other cases led to empty beds in cardiac units.17 That the healthcare system was perceived as inaccessible was reported by the participants in our study. There were thoughts that others needed the bed more or that they did not want to be in a setting with other diseased persons. However, a considerable number of the media reports were not entirely correct.29
Also, information from the Swedish Public Health Agency about personal responsibility, such as staying home, avoiding crowded settings, limiting any new close contacts, and working from home, had an impact on the care-seeking process.30 As the healthcare system was viewed as overloaded by the participants, the participants avoided seeking medical care as they thought someone else might need it more. These settings were also considered to pose a potential risk of being exposed to infection, which the participants avoided to the very last, and fear of acquiring the COVID-19 has been proposed as an explanation for not seeking medical care in patients with AMI.17,31 However, this study also highlights the effect of the media reporting on overloaded hospitals. A study by Nymark et al.32 showed that the number of patients cared for at departments of cardiology, heart surgery, vascular surgery, neurology, and neurosurgery was the same during the first wave as before the pandemic when comparing the data. Therefore, it is important that healthcare professionals collaborate with the media to spread information that is consistent with the current healthcare capacity when afflicted by an AMI.
Participants with risk factors expressed a fear of acquiring COVID-19 as it was considered to lead to a severe course of the disease. This is in line with another study where patients with risk factors such as cardiovascular diseases expressed more fear in relation to the pandemic than the general population.31 Moreover, in a previous study by Lidin et al.,19 they also highlighted this assumption. In their study, women and/or immigrants with AMI and risk factors, such as smoking and diabetes type II, to a greater extent answered that they would have sought medical care earlier if the pandemic had not existed.
Furthermore, in the mentioned study by Lidin et al.,19 there was a belief among the participants that the healthcare system was already overcrowded with patients with COVID-19, followed by a fear of becoming infected themselves at the hospital. In addition, in earlier studies, emotions such as fear, anxiety, and embarrassment contributed to delay, and these emotions have their origin in the perceived symptoms.3,4,33 It is notable that there is not an agreed scientific definition of the concept of emotion, although in its everyday use the meaning of ‘emotion’ is obvious.34 The concept of an emotional episode covers the dynamic unfolding of emotion and includes the changes in the appraisal of what can/or should be done to preserve or restore one's threatened well-being and integrity.35,36 Appraisal theories view emotions as adaptive responses reflecting perceptions, interpretations, and evaluations of features of the environment and events.36 Our study considers questions about emotions due to COVID-19 in relation to care-seeking. It seems that the emotion of fear was related to the external threat due to COVID-19 to one's own health, and not for the fear of symptoms related to an AMI, as reported in other studies.26,37 Moreover, the results highlight that as a consequence of these emotions, the pre-arranged healthcare meetings were cancelled and/or the medical care-seeking delayed, in line with previous studies.4,38 However, whether these delays were even more prolonged than delays before the pandemic, and the eventual consequences, such as a more severe illness after the AMI, are questions that must be probed in more detail.
Methodological considerations
The interviews were performed 5–9 months after the subject had been afflicted by an AMI. One limitation is that other aspects might have been captured if the interviews had been performed earlier as the memories and feelings may have been affected by the ongoing pandemic and the time that had passed since the cardiac event. However, the time delay should not affect the result significantly as the patients had clear memories from the event and could describe them in depth.
Conducting the interviews by phone may be no different to conducting them face-to-face, as it is important to ensure the participant feels that their answers are appreciated and their experiences are at the centre of the interview.39 There were discussions about conducting the interviews via video link. However, there were technical and confidentiality difficulties, and some of the participants declined, or could not manage such technology.
A strength of the study was the composition of the group of researchers, which contributed to a deeper understanding of the derived data through their profound and broad knowledge of nursing as well as their scientific knowledge. The knowledge in the group enriched the procedure of analysing the transcripts through a process of reflection and discussion,40 resulting in the presented sub-categories and categories. To be true to the participants’ descriptions and stay close to the data was of the utmost importance during the process.23 The back and forth process among authors, between the parts and the whole, further confirmed the trustworthiness. To support the trustworthiness of the results and address credibility and transferability, the results consist of rich descriptions and are supported by citations.23
Conclusions
The COVID-19 pandemic led to an increased patient delay when presenting with an AMI due to several reasons, among which fear of contracting the disease was prominent. It seems that the emotion of fear was related to the external threat to one's own health, due to COVID-19, and not the fear of symptoms related to an AMI, prolonging the medical care-seeking. Also, the media reporting the healthcare system as overloaded, the Swedish Public Health Agency recommendations about personal responsibility, as well as recommendations from other authorities, may have an influence on delay. It appears that the pandemic raised the threshold for deciding to seek medical care.
Funding
None declared.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Author notes
Johanna Granström and Pontus Lantz should be considered joint first authors.
Conflict of interest: The authors declare that there are no conflicts of interest.




Comments