-
PDF
- Split View
-
Views
-
Cite
Cite
Ekaterini Lambrinou, Martha Kyriakou, Ioanna Lakatamitou, Neil Angus, Rani Khatib, Ercole Vellone, Abigail Barrowcliff, Tina Birgitte Hansen, Geraldine A Lee, An integrative review on facilitators and barriers in delivering and managing injectable therapies in chronic conditions: A part of the ACNAP project ‘injectable medicines among patients with cardiovascular conditions’, European Journal of Cardiovascular Nursing, Volume 19, Issue 8, 1 December 2020, Pages 663–680, https://doi.org/10.1177/1474515120939007
Close - Share Icon Share
Although preventive health and therapeutics have benefited from advances in drug development and device innovation, translating these evidence-based treatments into real-world practice remains challenging.
The current integrative review aims to identify facilitators and barriers and perceptions in delivering and managing injectable therapies from patient perspectives.
An integrative review was conducted in the databases of PubMed, CINAHL, PsycINFO and Cochrane. Keywords were used “Injectable therapy”, “IV therapy”, “SC therapy”, “long term injectable therapies”, “self-administered injectable therapy”, “patients”, “caregivers”, “family”, “carers”, “facilitators”, “barriers”, “perspectives”, “needs”, “expectations”, “chronic disease”, “cardiovascular disease” linked with the words “OR” and “AND”. The search was limited from January 2000 to July 2019. Inclusion and exclusion criteria were used.
Twenty studies were identified from the literature search. Studies followed qualitative, quantitative methodology and mixed methods. Facilitators included: health improvement, prevention of disease complications, taking control of their disease, effectiveness of the medication and convenience in management. Barriers included: fear of needles, insulin will cause harm, poor perception of the benefits of injectable therapies on their quality of life, inconvenience in self-management, social stigma, impact on daily living, financial barriers, lack of education. Perceptions included: ‘treatment of last resort’, ‘life becomes less flexible’, ‘injectables were punishment/restriction’, ‘personal failure of self-management’.
Evidence shows how to create effective communication and shared decision-making relationships to provide best possible care to patients who need injectable therapy and support for self-management. Future research might help guide response to the fears and barriers of the patients using patients’ perspectives.
Introduction
Chronic diseases are characterised by an important reduction in mortality that has led to a substantial increase in life expectancy in the past 40 years.1 More specifically, although mortality from cardiovascular disease (CVD) is decreasing, CVD still remains the most common cause of death worldwide.1,2
It has been shown that most of the mortality incidence in type 2 diabetes mellitus (DM) is due to cardiovascular complications.3,4 DM affects life expectancy by approximately 10 years, with the main cause of death accounted for by CVD complications.5 In fact, in 2015, approximately 5.0 million patients were estimated to have died from diabetes, the majority of them as a result of cardiovascular complications. Although there is a lack of information regarding the exact epidemiological data of the comorbidity of DM and CVD, the International Diabetes Federation refers to the fact that in high and middle-income countries, the prevalence of all CVDs ranged from 14.8% to 40.5% in studies of people with DM types 1 and type 2.5 Adding to that, a recent systematic review concluded that CVD is a major cause of comorbidity and death among patients with DM, with CVD having the highest prevalence.6 Peripheral arterial disease is one of the most common first presentations of CVD, and has been shown to have the strongest association with type 2 DM, with an adjusted hazard ratio (HR) of 2.98 (95% confidence interval (CI) 2·76–3·22).7 Cardiovascular risk reduction through lipid lowering and management of DM represents one of the most evidence-rich areas of cardiology, and clinical medicine more broadly.4,8,–10
CVD and DM share modifiable risk factors and require a balanced approach that incorporates both prevention and treatment.5 There is a growing number of therapies with cardiovascular benefit that use the self-injectable form. These injectables are used by patients to manage a variety of conditions including hypercholesterolemia and diabetes.8,11,–13 Recent therapeutic developments in the area of injectable drug therapies include protease proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors (for lipid lowering) and incretin-based therapies (for diabetes). The uptake of these injectables has not been optimal to date. For instance, in the UK, the uptake is 70–80% below target. The low uptake is an important issue as patients eligible for these therapies need to be offered them in the first instance, and if this is not occurring the barriers to offering them need to be explored.
Long-acting injectable (LAI) therapies should not be considered by health professionals as a last resort in persistently ill patients; studies have shown that patients, when informed about injectable therapies from the beginning of diagnosis, showed increased medication adherence when these were prescribed.14,–16 Although prescribing rates have increased, frequently, people with DM or hypercholesterolemia or CVD do not adhere to medication resulting in poor clinical outcomes.17 Several studies have explored the use and adherence of patients using anti-psychotic injectable therapies. A review conducted in 2016 focusing on barriers to the use of LAI anti-psychotics, concluded that detecting and overcoming the principal barriers to the use of LAIs can lead to a personalised, shared decision management programme, helpful to achieve the optimal outcome for each patient.18
In the context of chronic diseases with multiple comorbidities and the issue of polypharmacy, the challenge of medication adherence is increasingly important.19,20 Medication adherence is undoubtedly vital for obtaining optimal CVD morbidity and mortality benefit, but it is also essential to develop an enhanced understanding about why patients are unable or unwilling to take prescribed medications.13,21 Adherence is defined as the extent to which patients follow agreed recommendations.22,23 Attention is turning to ways in which long-term adherence to medication to reduce the risk of recurrent events can be supported.17 Health professionals, especially nurses and pharmacists, need to be able to listen and understand patients’ needs and fears about these new therapies.
Undoubtedly, patients have concerns about starting on a new medication, especially ones that are injectable and therefore there is a need to identify these clearly. Assessing individual needs and identifying and reducing physical and psychological barriers to injectable medication has the potential to facilitate the earlier successful introduction of therapy into the treatment plan and thereby assist patients and their families to achieve optimal control of their chronic condition and increase adherence to these new therapies.24,–26 The current integrative review was conducted by Association of Cardiovascular Nursing and Allied Professionals (ACNAP) members aiming to identify facilitators, barriers and perceptions to injectable therapy to support the development of approaches able to respond to their needs and empower adherence to novel injectable therapies and better management of their chronic health conditions.
Aim of the current study
A review of the relevant literature using an integrative approach was used to determine the facilitators, barriers and perceptions in delivering and managing injectable therapies. The review was conducted by ACNAP members and examines injectables only from patient perspectives as part of the ACNAP project ‘Injectable medicines among patients with cardiovascular conditions’.
Methods
Study design
An integrative review was conducted regarding injectable therapies in an effort to identify the possible facilitators, barriers and perceptions in delivering and managing injectable therapies from patients’ perspectives. Integrative review is an approach that includes methodologically diverse studies and aims to influence or even change evidence-based practice as it is a synthesis of knowledge from available research.27 This approach was deemed appropriate to answer the research question.
Search methodology
A search was conducted in the databases of PubMed, CINAHL, PsycINFO and Cochrane. The following keywords were used as a search strategy as illustrated above: “Injectable therapy” OR “IV therapy” OR “SC therapy” OR “long term injectable therapies” OR “self-administered injectable therapy” AND “patients” OR “caregivers” OR “family” OR “carers” AND “facilitators” OR “barriers” OR “perspectives” OR “needs” OR “expectations” AND “chronic disease” OR “cardiovascular disease”. In order to obtain recent data, the search was limited to January 2000 to July 2019. In addition, the search was expanded to eligible articles from the reference lists of literature reviewed and from research studies not identified in the databases searched.
Inclusion and exclusion criteria were predefined before conducting the search. Articles examining facilitators and/or barriers and/or perceptions for injectable therapies were eligible to be included in the review. Articles had to be in English and including adult patients and any study methodology design was accepted. Studies in languages other than English or studies focusing on a paediatric (<18 years) population were excluded as were studies undertaken before January 2000. The literature to be included in this review was established independently by two reviewers based on the inclusion and exclusion criteria. A third reviewer adjudicated in the case of disagreement.
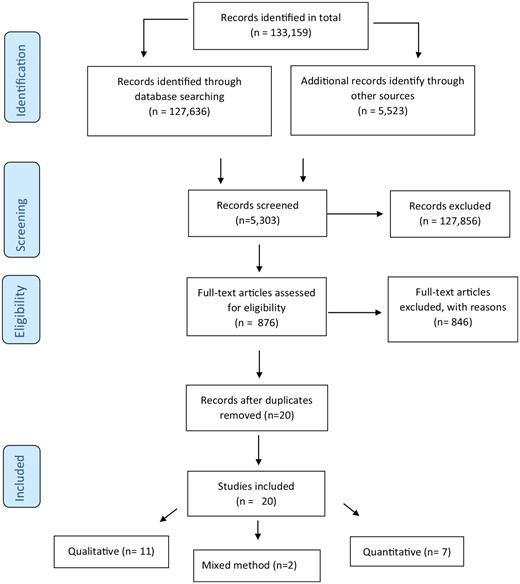
Based on the inclusion and exclusion criteria described a total of 133,159 potentially relevant articles were identified, from which 127,636 were identified through the electronic databases and the remaining 5523 from the citation tracking. A total of 127,856 articles were excluded after reading the title/abstract and the remaining 5303 were screened for eligibility. Researchers screened the full text of 876 articles from which 846 articles were excluded based on the predefined criteria and after duplicates were removed. The final review included 20 articles; 11 qualitative, seven quantitative and two mixed methods studies. A flow diagram of the selection procedure and results is illustrated in Figure 1 based on preferred reporting items for systematic reviews and meta-analyses (PRISMA).
As the purpose of this study was to synthesise all available findings of facilitators, barriers and perceptions regarding injectable therapies in studies utilising diverse methodologies, a quality appraisal was not conducted. Nevertheless, the main characteristics of the studies and an evidence-based ranking have been undertaken for each study in an effort to weigh the rigor and characteristics of each study.27,28 The main figures of each study are presented in Table 1.
| Author/year . | Study purpose . | Methods . | Findings . | Level of evidence . |
|---|---|---|---|---|
| Campbell et al., 201728 | To understand better the impact that financial barriers have on patients with diabetes and the strategies that they use to cope with them | Population: 24 patients (10 men and 14 women) including 10 who used insulin Mean age men 59.1 years Mean age women 56.5 years Methods: Secondary analysis of 24 interviews of patients with diabetes and perceived financial barriers Semi-structured interviews were undertaken either face-to-face or by telephone Data analysis was performed using inductive thematic analysis. Measures: Qualitative data: Personal interviews exploring the following domains: Experience of living with diabetes Experience of having financial barriers erceived reasons for financial barriers Perceived consequences of financial barriers Mechanisms for overcoming financial barriers | The predominant aspects of care to which participants described financial barriers were medications, diabetes supplies and healthy food. Participants described that health professionals had the potential to either play an important supporting role; or alternatively, that they could also worsen the impacts of financial barriers. | Level 6 |
| Taylor et al., 201729 | To document in people with DM attitudes and beliefs that may result in psychological insulin resistance | Population: 117 patients Women 80 Mean age 66 years Methods: Quantitative through an interview administrated questionnaire Telephone interviews Measures: Attitudes and beliefs towards insulin (ITAS questionnaire) | Negative perceptions about insulin use 1. Meant a worsening of diabetes (68%) 2. Would worry family (63%) 3. Feared self-injection (58%) 4. Meant a failure in self-management (57%) 5. Injections were painful (54%) 6. Would be seen as being sicker (46%) 7. Increased hypoglycaemia risk (38%) 8. Required effort (34%) 9. Causes weight gain (27%) 10. Causes a deterioration in health (14%) 11. Would have to give up enjoyable activities (10%) Positive perceptions • Helps good glycaemic control (78%) • Would prevent complications (61%) • Improves health (58%) Patients using insulin had fewer negative perceptions than those not on insulin. | Level 6 |
| Taylor et al., 201630 | To explore self-reported knowledge and attitudes to insulin treatment among a group of adults with poorly controlled diabetes | Population: 29 patients Women 14 Methods: Quantitative study Cross-sectional study Measures: Insulin treatment Appraisal scale (ITAS) and barriers to insulin treatment Questionnaire (BITQ) scores related to knowledge and attitudes to insulin treatment, clinical and demographic measures | Perceived barriers are higher among older patients with fewer years of formal education. Low score in ‘knowledge’ items in the ITAS. | Level 6 |
| Victor Spain et al., 201614 | To explore the barriers that adult Americans experience when taking injectable medications for type 2 diabetes, from the time of filling the initial prescription through the decision to discontinue the medication | Population: 1190 patients Women 986 Methods: Quantitative using self-administrated questionnaire developed for the survey and DES Internet-based survey. Measures: Patients were asked: 1. If they filled the medication of interest when first prescribed, time until filling the prescription and if filled, how long until they started taking it 2. About their reactions to being prescribed an injectable 3. For those initiating the medication of interest, if they discontinued using it 4. For those discontinuing the medication of interest, the reasons for discontinuing use and the decision-making process for discontinuation 5. If still taking the medication of interest, what barriers (if any) to taking it they experienced | Among patients who delayed filling their prescription by more than one week, cost was a common reason for delay. The most commonly reported barrier to maintaining injectable medication was injection concerns (42%) such as aversion to needles, pain or needle size. Lack of perceived need was the most common reason for discontinuation for basal (47%) and prandial/premixed (44%) insulin. For liraglutide, the most common reason for discontinuation was experiencing an adverse event (33%), for exenatide once weekly, it was injection concerns such as aversion to needles, pain, or needle size (38%). | Level 6 |
| Papaspurou et al., 201531 | To investigate the health needs and self-management problems faced by patients with diabetes daily | Population: 15 patients Women 9 Methods: Qualitative study Sem-structured interviews (interpretative phenomenological approach) Measures: Health needs and self-management problems faced by patients with DM | Patients face fears and have unaddressed needs related to the diagnosis, treatment, expected impacts, prognosis and the daily management of the disease. Patients have several care needs; need of psychological support and education to recognize and prevent hypoglycaemia. Need of continuous education and communication with health professionals. | Level 6 |
| Patel et al., 201515 | To explore attitudes towards insulin acceptance an ethnically diverse population of people with type 2 diabetes | Population: 18 patients Women 9 Methods: Qualitative study Semi-structured interviews Purposive sampling Measures: Concerns, views and beliefs about the necessity of insulin | Decisions about accepting insulin involved balancing concerns against the perceived necessity of insulin (generally, inadequacy of oral medication). | Level 6 |
| Brod et al., 201432 | To identify patients’ beliefs as well as clinical realities about insulin that may be barriers to type 2 diabetes patients initiating insulin treatment | Population: 87 patients Women 37 Mean age: 52.9 years Methods: Purposive sample Mixed methods study 13 focus group in 5 different countries Measures: Qualitative data on attitudes through focus groups. Quantitative data were collected to understand better the factors influencing participants’ decisions about initiating insulin and patient-held beliefs regarding the process through the developed educational tool ‘questions about starting insulin: information on the myths, misconceptions and clinical realities about insulin’. | Patients’ reported the following key barriers to initiating insulin Treatment: 1.Insulin as a treatment of last resort 2. Insulin as evidence of personal failure to self-manage diabetes 3. Risk of long-term complications from insulin 4. Side effects of insulin 5. Treatment convenience 6. Needles and injections 7. Weight gain from insulin | Level 4 |
| Simon et al., 201433 | To identify experiences with and barriers to self-monitoring of blood glucose, insulin injection, and insulin titration among patients with type 2 diabetes | Population: 20 patients Group A: Patients who had never used computer-assisted insulin self-titration system Women 4 Mean age 53.9 years Group B: Patients who were enrolled in a 4-week pilot involving computer-assisted insulin self-titration system Women 4 Mean age 56.9 years Sampling method: In-depth, semi-structured interviews Face to face interviews for group A and telephone interviews for group B Design: Qualitative study Measures: Experiences with and barriers to insulin Self-management | Patients fear the lifelong commitment to insulin therapy and disease progression Barriers when implementing insulin therapy (e.g. perceived usefulness, physical impact, fear of injection) Difficulties increasing the insulin dose (fear of hypoglycaemia) Association of higher insulin doses with disease progression Ignorant of treatment targets Patients who never used a computer-assisted insulin self-titration system felt they had enough knowledge to know when their insulin should be adjusted, but still believed that the system advice would be useful to confirm their reasoning. | Level 6 |
| Iyer et al., 201334 | To investigate perceptions of and attitudes towards long-acting (once every 2 weeks) injectable antipsychotics among patients | Population: 34 patients Women 7 Methods: Qualitative study Focus groups Measures: Experiences with and attitudes toward LAI antipsychotic medication | 1. Awareness of and knowledge about LAI antipsychotics: Some patients had never heard about LAI antipsychotics, some others reported not having understood what was discussed with them regarding LAI antipsychotics and some patients had typically heard about. 2. Perceptions about LAI antipsychotics: Positive perceptions: Relapse prevention and reduced effort in ensuring adherence Negative perceptions: Financial costs and the inconvenience of appointments to receive injections a. Cost and convenience considerations b. Issues arising from the coercive context under which LAI antipsychotics were often prescribed | Level 6 |
| Potkin et al., 201311 | To understand better prescriber, patient and caregiver perspectives about LAI antipsychotics (administered once every 2 or 4 weeks) therapy and how these perspectives affect their use | Population: 22 patients Women 13 Mean age 45.7 years Methods: Qualitative Ethnographic information of non-random sample of prescriber–patient conversations. Also, in-person observations in mental health centres including home visits Telephone in-depth interviews for additional information Measures: Perspectives about LAI antipsychotic therapy How perspectives affect LAI use | Involvement of patients in treatment decisions was greater when discussing LAI antipsychotics versus oral antipsychotic treatment. LAI antipsychotics -naïve patients expressed neutral rather than favorable or unfavorable responses. Patient resistance was often related to negative feelings about injections. Patient-described benefits of LAI antipsychotics versus orals included perceived rapid symptom improvement and greater overall efficacy. | Level 6 |
| Tan et al., 201135 | To determine the issues relating to insulin initiation for diabetes patients managed in primary care polyclinics | Population: 11 patients Women 5 Methods: Qualitative study, focus groups Purposive sample (doctors and nurses from different training backgrounds and years of experience; poorly controlled diabetes patients who refused insulin therapy despite being on maximum oral hypoglycaemic drugs and patients who were on insulin therapy). Measures: Barriers to insulin commencement | 1. Launching the topic and doctor-patient communication on insulin therapy were key issues in insulin initiation. 2. Patient barriers to insulin commencement included: refusal to acknowledge the need for insulin therapy, its perception as a social stigma, an inconvenient mode of treatment or punishment for failure and fear of needles, side effects and complications and the healthcare professionals’ attitude and experience with insulin therapy. | Level 6 |
| Jenkings et al., 201036 | To explore patients and health professionals’ experiences of initiating insulin as part of the treating to target in DM | Population: 45 patients and 21 health professionals Women 16 Mean age 64.7 years Methods: Qualitative through interviews Purposive sample Measures: Interviews which explored participants understandings and experiences of insulin initiation | Patients reported the key factors that fostered resistance to insulin initiation: 1. Engagement with disease progression. Patients felt that they personally failed with diabetes management. 2. Managing anxieties about insulin therapy. Patients were anxious about the prospect of injecting but frequently they surprised when they discover that they can use insulin pens. | Level 6 |
| Karter et al., 201016 | To investigate barriers to insulin initiation following a new prescription | Population: 169 patients Adherent patients mean age 58 years Women 47% Non-adherent patients mean age 61 years 35% women Methods: Mixed methods Telephone interviews and self-administered survey Patients receiving a new electronic prescription for insulin. Random sample from pharmacy records Measures: Barriers to insulin initiation among non-adherent and adherent patients newly prescribed insulin | Non-adherent patients: Reasons for failing to initiate insulin included: the patient planned to change health behaviours instead of starting insulin, injection phobia, negative impact on work, concerns about long-term medication use, inconvenience and not believing insulin was needed. Believed that people who require insulin ‘have not taken care of themselves in the past’ and that ‘taking insulin can cause. . .’ other consequences. They believed insulin causes harm. Expressed significantly more concern about their inability to adjust insulin dosage, the impact on social life and work, injection pain, and side effects. Reported problems learning about their medical condition because of difficulty understanding written information and claimed providers failed to adequately explain insulin’s risk and benefits. Fewer non-adherent patients reported receiving insulin self-management training from their doctor, nurse, health educator, or a class. | Level 4 |
| Peyrot et al., 201037 | To access factors associated with patient frequency of intentionally skipping insulin injections | Population: 502 patients Women 226 Mean age 55 years Methods: Quantitative study Internet survey with a questionnaire developed for the particular survey. Measures: Disease type, duration, complications and treatment Perceived burden of insulin injections The experience of injections Negative affect toward insulin injections Frequency of skipping insulin injections | Patients who are not managing their diabetes are significantly more likely to see insulin therapy as potentially beneficial. Most nurses and general practitioners delay insulin therapy until absolutely necessary, but specialists and opinion leaders are less likely to do so. Delay of insulin therapy is significantly less likely when physicians and nurses see their patients as more adherent to medication or appointment regimens, view insulin as more efficacious, and when they are less likely to delay oral diabetes medications. | Level 6 |
| Rubin et al., 200910 | To compare patients’ perceptions of injection-related problems with clinicians estimates of those problems | Population: 501 patients Women 225 Mean age 54.9 years Methods: Quantitative through interviews Internet survey of self-identified patients with diabetes Measures: 1. Perceived burden of insulin injections 2. Effect of injections on quality of life 3. Effect of injection problems on adherence to treatment 4. Patient-provider injection-related communication 5. Injection-related support from provider 6. Interest in and knowledge of products to ease injection burden | The majority of patients would like to reduce the number of injections they take each day. Almost half said that they would be more likely to take their insulin injections regularly if a product were available to ease the pain. Patients also reported: 1. Injections were a serious burden 2. They were dissatisfied with the way they took insulin 3. Injections had a substantial negative impact on quality of life 4. They skipped injections they should take or 5. Injection-related problems affected the number of injections they were willing to take. Half of the patients said they mentioned injection-related problems to their provider; a similar number reported that their providers had not given them a solution to problems with injection-related pain and bruising. | Level 6 |
| Khan et al., 200838 | To determine the prevalence and reasons for refusal to commence insulin in Bangladeshi patients with type 2 diabetes | Population: 212 patients Women 100 Mean age 55.3 years Methods: Qualitative study through focus groups Data were analysed by thematic content analysis using the constant comparative method. Measures: Reasons of insulin refusal | Patients refused insulin due to: 1. Disease severity: perceptions that requirement for insulin was an indicator of a more serious stage of their condition 2. Insulin leading to premature death: common suggestion that commencing insulin led to early death 3. Loss of control: fear of hypoglycaemia, weight gain, loss of independence and reliance on others to give insulin or look for signs of hypoglycaemia 4. Lack of perception of benefits: poor perception of the benefits of improved glycaemic control on quality of life and cardiovascular risk 5. Needle anxiety: concern over frequent injections. | Level 6 |
| Larkin et al., 200839 | To explore the attitudes that contribute to psychological insulin resistance (PIR) in insulin-naive patients with type 2 diabetes and to identify predictors of PIR | Population: 100 patients Women 39 Mean age 62 years Methods: Quantitative study Self-administrative questionnaires Measures: 1. Survey for people who do not take insulin: reasons why people are reluctant to start insulin, including risk of side effects or complications and changes in lifestyle 2. ITAS: assessment of patients’ perceptions of insulin treatment 3. HADS: depression screening questionnaire | The most commonly expressed negative attitudes were concern regarding hypoglycaemia, permanent need for insulin therapy, less flexibility, and feelings of failure. Less than 40% expressed fear of self-injection or thought that injections were painful. Poorer general health and higher depression scores also correlated with PIR. | Level 6 |
| Hayes et al., 200640 | To explore diabetes medication experiences of patients with type 2 diabetes | Population: 138 patients Women 94 61% were using insulin Methods: Qualitative study through focus groups Measures: How patients experience their diabetes drug treatment What they dislike about treatment What makes it inconvenient or inflexible, intolerable, or unacceptable What factors contribute to their treatment satisfaction and treatment preference | Patients expressed: 1. Inconvenience and inflexibility of the timing and frequency of administrations of many diabetes medication regimens. 2. Avoidance of injections and/or insulin therapy 3. The physical and emotional side effects of diabetes medications. Treatment preferences: Participants would weigh the convenience and flexibility, route of administration, side effects, and cost of the medications. | Level 6 |
| Morris et al., 200541 | To elucidate the range of subjective experiences of men and women with type 2 diabetes who have recently gone on to insulin | Population: Six patients Women 3 Methods: Qualitative study Semi-structured interviews which were audiotape-recorded and transcribed. Transcripts were analysed together with the researcher’s observational notes and documentary evidence (phenomenological analysis) Purposive sample Measures: Experiences of patients with DM | Patients experienced a range of initial reactions (from shock and anger, to relief) and perceptions of insulin, sometimes resulting in an altered self-image. Perceptions for insulin were shown to change over time, with some patients eventually accepting insulin and becoming empowered. | Level 6 |
| Mollema et al., 200142 | To define clinically relevant cut-off points for severe fear of self-injecting and self-treated phobia in insulin-treated patients with diabetes and to estimate the magnitude of these phobias in our research population | Population: 24 insulin-treated adult diabetes patients Women 17 Mean age 44.5 years Methods: Quantitative study Cross-sectional survey Purposive sample (high-scorers on FSI and/or FST) Measures: Relevance of fear of self-injecting (FSI) and self-testing (FST) (phobia) in insulin-treated patients with diabetes D-FISQ and BAT questionnaires | Severe FSI and FST, characterised by emotional distress and avoidance behaviour, seems to occur in a small group of insulin-treated patients with diabetes | Level 6 |
| Author/year . | Study purpose . | Methods . | Findings . | Level of evidence . |
|---|---|---|---|---|
| Campbell et al., 201728 | To understand better the impact that financial barriers have on patients with diabetes and the strategies that they use to cope with them | Population: 24 patients (10 men and 14 women) including 10 who used insulin Mean age men 59.1 years Mean age women 56.5 years Methods: Secondary analysis of 24 interviews of patients with diabetes and perceived financial barriers Semi-structured interviews were undertaken either face-to-face or by telephone Data analysis was performed using inductive thematic analysis. Measures: Qualitative data: Personal interviews exploring the following domains: Experience of living with diabetes Experience of having financial barriers erceived reasons for financial barriers Perceived consequences of financial barriers Mechanisms for overcoming financial barriers | The predominant aspects of care to which participants described financial barriers were medications, diabetes supplies and healthy food. Participants described that health professionals had the potential to either play an important supporting role; or alternatively, that they could also worsen the impacts of financial barriers. | Level 6 |
| Taylor et al., 201729 | To document in people with DM attitudes and beliefs that may result in psychological insulin resistance | Population: 117 patients Women 80 Mean age 66 years Methods: Quantitative through an interview administrated questionnaire Telephone interviews Measures: Attitudes and beliefs towards insulin (ITAS questionnaire) | Negative perceptions about insulin use 1. Meant a worsening of diabetes (68%) 2. Would worry family (63%) 3. Feared self-injection (58%) 4. Meant a failure in self-management (57%) 5. Injections were painful (54%) 6. Would be seen as being sicker (46%) 7. Increased hypoglycaemia risk (38%) 8. Required effort (34%) 9. Causes weight gain (27%) 10. Causes a deterioration in health (14%) 11. Would have to give up enjoyable activities (10%) Positive perceptions • Helps good glycaemic control (78%) • Would prevent complications (61%) • Improves health (58%) Patients using insulin had fewer negative perceptions than those not on insulin. | Level 6 |
| Taylor et al., 201630 | To explore self-reported knowledge and attitudes to insulin treatment among a group of adults with poorly controlled diabetes | Population: 29 patients Women 14 Methods: Quantitative study Cross-sectional study Measures: Insulin treatment Appraisal scale (ITAS) and barriers to insulin treatment Questionnaire (BITQ) scores related to knowledge and attitudes to insulin treatment, clinical and demographic measures | Perceived barriers are higher among older patients with fewer years of formal education. Low score in ‘knowledge’ items in the ITAS. | Level 6 |
| Victor Spain et al., 201614 | To explore the barriers that adult Americans experience when taking injectable medications for type 2 diabetes, from the time of filling the initial prescription through the decision to discontinue the medication | Population: 1190 patients Women 986 Methods: Quantitative using self-administrated questionnaire developed for the survey and DES Internet-based survey. Measures: Patients were asked: 1. If they filled the medication of interest when first prescribed, time until filling the prescription and if filled, how long until they started taking it 2. About their reactions to being prescribed an injectable 3. For those initiating the medication of interest, if they discontinued using it 4. For those discontinuing the medication of interest, the reasons for discontinuing use and the decision-making process for discontinuation 5. If still taking the medication of interest, what barriers (if any) to taking it they experienced | Among patients who delayed filling their prescription by more than one week, cost was a common reason for delay. The most commonly reported barrier to maintaining injectable medication was injection concerns (42%) such as aversion to needles, pain or needle size. Lack of perceived need was the most common reason for discontinuation for basal (47%) and prandial/premixed (44%) insulin. For liraglutide, the most common reason for discontinuation was experiencing an adverse event (33%), for exenatide once weekly, it was injection concerns such as aversion to needles, pain, or needle size (38%). | Level 6 |
| Papaspurou et al., 201531 | To investigate the health needs and self-management problems faced by patients with diabetes daily | Population: 15 patients Women 9 Methods: Qualitative study Sem-structured interviews (interpretative phenomenological approach) Measures: Health needs and self-management problems faced by patients with DM | Patients face fears and have unaddressed needs related to the diagnosis, treatment, expected impacts, prognosis and the daily management of the disease. Patients have several care needs; need of psychological support and education to recognize and prevent hypoglycaemia. Need of continuous education and communication with health professionals. | Level 6 |
| Patel et al., 201515 | To explore attitudes towards insulin acceptance an ethnically diverse population of people with type 2 diabetes | Population: 18 patients Women 9 Methods: Qualitative study Semi-structured interviews Purposive sampling Measures: Concerns, views and beliefs about the necessity of insulin | Decisions about accepting insulin involved balancing concerns against the perceived necessity of insulin (generally, inadequacy of oral medication). | Level 6 |
| Brod et al., 201432 | To identify patients’ beliefs as well as clinical realities about insulin that may be barriers to type 2 diabetes patients initiating insulin treatment | Population: 87 patients Women 37 Mean age: 52.9 years Methods: Purposive sample Mixed methods study 13 focus group in 5 different countries Measures: Qualitative data on attitudes through focus groups. Quantitative data were collected to understand better the factors influencing participants’ decisions about initiating insulin and patient-held beliefs regarding the process through the developed educational tool ‘questions about starting insulin: information on the myths, misconceptions and clinical realities about insulin’. | Patients’ reported the following key barriers to initiating insulin Treatment: 1.Insulin as a treatment of last resort 2. Insulin as evidence of personal failure to self-manage diabetes 3. Risk of long-term complications from insulin 4. Side effects of insulin 5. Treatment convenience 6. Needles and injections 7. Weight gain from insulin | Level 4 |
| Simon et al., 201433 | To identify experiences with and barriers to self-monitoring of blood glucose, insulin injection, and insulin titration among patients with type 2 diabetes | Population: 20 patients Group A: Patients who had never used computer-assisted insulin self-titration system Women 4 Mean age 53.9 years Group B: Patients who were enrolled in a 4-week pilot involving computer-assisted insulin self-titration system Women 4 Mean age 56.9 years Sampling method: In-depth, semi-structured interviews Face to face interviews for group A and telephone interviews for group B Design: Qualitative study Measures: Experiences with and barriers to insulin Self-management | Patients fear the lifelong commitment to insulin therapy and disease progression Barriers when implementing insulin therapy (e.g. perceived usefulness, physical impact, fear of injection) Difficulties increasing the insulin dose (fear of hypoglycaemia) Association of higher insulin doses with disease progression Ignorant of treatment targets Patients who never used a computer-assisted insulin self-titration system felt they had enough knowledge to know when their insulin should be adjusted, but still believed that the system advice would be useful to confirm their reasoning. | Level 6 |
| Iyer et al., 201334 | To investigate perceptions of and attitudes towards long-acting (once every 2 weeks) injectable antipsychotics among patients | Population: 34 patients Women 7 Methods: Qualitative study Focus groups Measures: Experiences with and attitudes toward LAI antipsychotic medication | 1. Awareness of and knowledge about LAI antipsychotics: Some patients had never heard about LAI antipsychotics, some others reported not having understood what was discussed with them regarding LAI antipsychotics and some patients had typically heard about. 2. Perceptions about LAI antipsychotics: Positive perceptions: Relapse prevention and reduced effort in ensuring adherence Negative perceptions: Financial costs and the inconvenience of appointments to receive injections a. Cost and convenience considerations b. Issues arising from the coercive context under which LAI antipsychotics were often prescribed | Level 6 |
| Potkin et al., 201311 | To understand better prescriber, patient and caregiver perspectives about LAI antipsychotics (administered once every 2 or 4 weeks) therapy and how these perspectives affect their use | Population: 22 patients Women 13 Mean age 45.7 years Methods: Qualitative Ethnographic information of non-random sample of prescriber–patient conversations. Also, in-person observations in mental health centres including home visits Telephone in-depth interviews for additional information Measures: Perspectives about LAI antipsychotic therapy How perspectives affect LAI use | Involvement of patients in treatment decisions was greater when discussing LAI antipsychotics versus oral antipsychotic treatment. LAI antipsychotics -naïve patients expressed neutral rather than favorable or unfavorable responses. Patient resistance was often related to negative feelings about injections. Patient-described benefits of LAI antipsychotics versus orals included perceived rapid symptom improvement and greater overall efficacy. | Level 6 |
| Tan et al., 201135 | To determine the issues relating to insulin initiation for diabetes patients managed in primary care polyclinics | Population: 11 patients Women 5 Methods: Qualitative study, focus groups Purposive sample (doctors and nurses from different training backgrounds and years of experience; poorly controlled diabetes patients who refused insulin therapy despite being on maximum oral hypoglycaemic drugs and patients who were on insulin therapy). Measures: Barriers to insulin commencement | 1. Launching the topic and doctor-patient communication on insulin therapy were key issues in insulin initiation. 2. Patient barriers to insulin commencement included: refusal to acknowledge the need for insulin therapy, its perception as a social stigma, an inconvenient mode of treatment or punishment for failure and fear of needles, side effects and complications and the healthcare professionals’ attitude and experience with insulin therapy. | Level 6 |
| Jenkings et al., 201036 | To explore patients and health professionals’ experiences of initiating insulin as part of the treating to target in DM | Population: 45 patients and 21 health professionals Women 16 Mean age 64.7 years Methods: Qualitative through interviews Purposive sample Measures: Interviews which explored participants understandings and experiences of insulin initiation | Patients reported the key factors that fostered resistance to insulin initiation: 1. Engagement with disease progression. Patients felt that they personally failed with diabetes management. 2. Managing anxieties about insulin therapy. Patients were anxious about the prospect of injecting but frequently they surprised when they discover that they can use insulin pens. | Level 6 |
| Karter et al., 201016 | To investigate barriers to insulin initiation following a new prescription | Population: 169 patients Adherent patients mean age 58 years Women 47% Non-adherent patients mean age 61 years 35% women Methods: Mixed methods Telephone interviews and self-administered survey Patients receiving a new electronic prescription for insulin. Random sample from pharmacy records Measures: Barriers to insulin initiation among non-adherent and adherent patients newly prescribed insulin | Non-adherent patients: Reasons for failing to initiate insulin included: the patient planned to change health behaviours instead of starting insulin, injection phobia, negative impact on work, concerns about long-term medication use, inconvenience and not believing insulin was needed. Believed that people who require insulin ‘have not taken care of themselves in the past’ and that ‘taking insulin can cause. . .’ other consequences. They believed insulin causes harm. Expressed significantly more concern about their inability to adjust insulin dosage, the impact on social life and work, injection pain, and side effects. Reported problems learning about their medical condition because of difficulty understanding written information and claimed providers failed to adequately explain insulin’s risk and benefits. Fewer non-adherent patients reported receiving insulin self-management training from their doctor, nurse, health educator, or a class. | Level 4 |
| Peyrot et al., 201037 | To access factors associated with patient frequency of intentionally skipping insulin injections | Population: 502 patients Women 226 Mean age 55 years Methods: Quantitative study Internet survey with a questionnaire developed for the particular survey. Measures: Disease type, duration, complications and treatment Perceived burden of insulin injections The experience of injections Negative affect toward insulin injections Frequency of skipping insulin injections | Patients who are not managing their diabetes are significantly more likely to see insulin therapy as potentially beneficial. Most nurses and general practitioners delay insulin therapy until absolutely necessary, but specialists and opinion leaders are less likely to do so. Delay of insulin therapy is significantly less likely when physicians and nurses see their patients as more adherent to medication or appointment regimens, view insulin as more efficacious, and when they are less likely to delay oral diabetes medications. | Level 6 |
| Rubin et al., 200910 | To compare patients’ perceptions of injection-related problems with clinicians estimates of those problems | Population: 501 patients Women 225 Mean age 54.9 years Methods: Quantitative through interviews Internet survey of self-identified patients with diabetes Measures: 1. Perceived burden of insulin injections 2. Effect of injections on quality of life 3. Effect of injection problems on adherence to treatment 4. Patient-provider injection-related communication 5. Injection-related support from provider 6. Interest in and knowledge of products to ease injection burden | The majority of patients would like to reduce the number of injections they take each day. Almost half said that they would be more likely to take their insulin injections regularly if a product were available to ease the pain. Patients also reported: 1. Injections were a serious burden 2. They were dissatisfied with the way they took insulin 3. Injections had a substantial negative impact on quality of life 4. They skipped injections they should take or 5. Injection-related problems affected the number of injections they were willing to take. Half of the patients said they mentioned injection-related problems to their provider; a similar number reported that their providers had not given them a solution to problems with injection-related pain and bruising. | Level 6 |
| Khan et al., 200838 | To determine the prevalence and reasons for refusal to commence insulin in Bangladeshi patients with type 2 diabetes | Population: 212 patients Women 100 Mean age 55.3 years Methods: Qualitative study through focus groups Data were analysed by thematic content analysis using the constant comparative method. Measures: Reasons of insulin refusal | Patients refused insulin due to: 1. Disease severity: perceptions that requirement for insulin was an indicator of a more serious stage of their condition 2. Insulin leading to premature death: common suggestion that commencing insulin led to early death 3. Loss of control: fear of hypoglycaemia, weight gain, loss of independence and reliance on others to give insulin or look for signs of hypoglycaemia 4. Lack of perception of benefits: poor perception of the benefits of improved glycaemic control on quality of life and cardiovascular risk 5. Needle anxiety: concern over frequent injections. | Level 6 |
| Larkin et al., 200839 | To explore the attitudes that contribute to psychological insulin resistance (PIR) in insulin-naive patients with type 2 diabetes and to identify predictors of PIR | Population: 100 patients Women 39 Mean age 62 years Methods: Quantitative study Self-administrative questionnaires Measures: 1. Survey for people who do not take insulin: reasons why people are reluctant to start insulin, including risk of side effects or complications and changes in lifestyle 2. ITAS: assessment of patients’ perceptions of insulin treatment 3. HADS: depression screening questionnaire | The most commonly expressed negative attitudes were concern regarding hypoglycaemia, permanent need for insulin therapy, less flexibility, and feelings of failure. Less than 40% expressed fear of self-injection or thought that injections were painful. Poorer general health and higher depression scores also correlated with PIR. | Level 6 |
| Hayes et al., 200640 | To explore diabetes medication experiences of patients with type 2 diabetes | Population: 138 patients Women 94 61% were using insulin Methods: Qualitative study through focus groups Measures: How patients experience their diabetes drug treatment What they dislike about treatment What makes it inconvenient or inflexible, intolerable, or unacceptable What factors contribute to their treatment satisfaction and treatment preference | Patients expressed: 1. Inconvenience and inflexibility of the timing and frequency of administrations of many diabetes medication regimens. 2. Avoidance of injections and/or insulin therapy 3. The physical and emotional side effects of diabetes medications. Treatment preferences: Participants would weigh the convenience and flexibility, route of administration, side effects, and cost of the medications. | Level 6 |
| Morris et al., 200541 | To elucidate the range of subjective experiences of men and women with type 2 diabetes who have recently gone on to insulin | Population: Six patients Women 3 Methods: Qualitative study Semi-structured interviews which were audiotape-recorded and transcribed. Transcripts were analysed together with the researcher’s observational notes and documentary evidence (phenomenological analysis) Purposive sample Measures: Experiences of patients with DM | Patients experienced a range of initial reactions (from shock and anger, to relief) and perceptions of insulin, sometimes resulting in an altered self-image. Perceptions for insulin were shown to change over time, with some patients eventually accepting insulin and becoming empowered. | Level 6 |
| Mollema et al., 200142 | To define clinically relevant cut-off points for severe fear of self-injecting and self-treated phobia in insulin-treated patients with diabetes and to estimate the magnitude of these phobias in our research population | Population: 24 insulin-treated adult diabetes patients Women 17 Mean age 44.5 years Methods: Quantitative study Cross-sectional survey Purposive sample (high-scorers on FSI and/or FST) Measures: Relevance of fear of self-injecting (FSI) and self-testing (FST) (phobia) in insulin-treated patients with diabetes D-FISQ and BAT questionnaires | Severe FSI and FST, characterised by emotional distress and avoidance behaviour, seems to occur in a small group of insulin-treated patients with diabetes | Level 6 |
LAI: long-acting injectable; ITAS: insulin treatment appraisal scale; BITQ: barriers to insulin treatment questionnaire; DES: diabetes empowerment scale; DM: diabetes mellitus; HADS: hospital anxiety and depression scale; D-FISQ: diabetes fear of injecting and self-testing questionnaire; BAT: behavioural avoidance test.
| Author/year . | Study purpose . | Methods . | Findings . | Level of evidence . |
|---|---|---|---|---|
| Campbell et al., 201728 | To understand better the impact that financial barriers have on patients with diabetes and the strategies that they use to cope with them | Population: 24 patients (10 men and 14 women) including 10 who used insulin Mean age men 59.1 years Mean age women 56.5 years Methods: Secondary analysis of 24 interviews of patients with diabetes and perceived financial barriers Semi-structured interviews were undertaken either face-to-face or by telephone Data analysis was performed using inductive thematic analysis. Measures: Qualitative data: Personal interviews exploring the following domains: Experience of living with diabetes Experience of having financial barriers erceived reasons for financial barriers Perceived consequences of financial barriers Mechanisms for overcoming financial barriers | The predominant aspects of care to which participants described financial barriers were medications, diabetes supplies and healthy food. Participants described that health professionals had the potential to either play an important supporting role; or alternatively, that they could also worsen the impacts of financial barriers. | Level 6 |
| Taylor et al., 201729 | To document in people with DM attitudes and beliefs that may result in psychological insulin resistance | Population: 117 patients Women 80 Mean age 66 years Methods: Quantitative through an interview administrated questionnaire Telephone interviews Measures: Attitudes and beliefs towards insulin (ITAS questionnaire) | Negative perceptions about insulin use 1. Meant a worsening of diabetes (68%) 2. Would worry family (63%) 3. Feared self-injection (58%) 4. Meant a failure in self-management (57%) 5. Injections were painful (54%) 6. Would be seen as being sicker (46%) 7. Increased hypoglycaemia risk (38%) 8. Required effort (34%) 9. Causes weight gain (27%) 10. Causes a deterioration in health (14%) 11. Would have to give up enjoyable activities (10%) Positive perceptions • Helps good glycaemic control (78%) • Would prevent complications (61%) • Improves health (58%) Patients using insulin had fewer negative perceptions than those not on insulin. | Level 6 |
| Taylor et al., 201630 | To explore self-reported knowledge and attitudes to insulin treatment among a group of adults with poorly controlled diabetes | Population: 29 patients Women 14 Methods: Quantitative study Cross-sectional study Measures: Insulin treatment Appraisal scale (ITAS) and barriers to insulin treatment Questionnaire (BITQ) scores related to knowledge and attitudes to insulin treatment, clinical and demographic measures | Perceived barriers are higher among older patients with fewer years of formal education. Low score in ‘knowledge’ items in the ITAS. | Level 6 |
| Victor Spain et al., 201614 | To explore the barriers that adult Americans experience when taking injectable medications for type 2 diabetes, from the time of filling the initial prescription through the decision to discontinue the medication | Population: 1190 patients Women 986 Methods: Quantitative using self-administrated questionnaire developed for the survey and DES Internet-based survey. Measures: Patients were asked: 1. If they filled the medication of interest when first prescribed, time until filling the prescription and if filled, how long until they started taking it 2. About their reactions to being prescribed an injectable 3. For those initiating the medication of interest, if they discontinued using it 4. For those discontinuing the medication of interest, the reasons for discontinuing use and the decision-making process for discontinuation 5. If still taking the medication of interest, what barriers (if any) to taking it they experienced | Among patients who delayed filling their prescription by more than one week, cost was a common reason for delay. The most commonly reported barrier to maintaining injectable medication was injection concerns (42%) such as aversion to needles, pain or needle size. Lack of perceived need was the most common reason for discontinuation for basal (47%) and prandial/premixed (44%) insulin. For liraglutide, the most common reason for discontinuation was experiencing an adverse event (33%), for exenatide once weekly, it was injection concerns such as aversion to needles, pain, or needle size (38%). | Level 6 |
| Papaspurou et al., 201531 | To investigate the health needs and self-management problems faced by patients with diabetes daily | Population: 15 patients Women 9 Methods: Qualitative study Sem-structured interviews (interpretative phenomenological approach) Measures: Health needs and self-management problems faced by patients with DM | Patients face fears and have unaddressed needs related to the diagnosis, treatment, expected impacts, prognosis and the daily management of the disease. Patients have several care needs; need of psychological support and education to recognize and prevent hypoglycaemia. Need of continuous education and communication with health professionals. | Level 6 |
| Patel et al., 201515 | To explore attitudes towards insulin acceptance an ethnically diverse population of people with type 2 diabetes | Population: 18 patients Women 9 Methods: Qualitative study Semi-structured interviews Purposive sampling Measures: Concerns, views and beliefs about the necessity of insulin | Decisions about accepting insulin involved balancing concerns against the perceived necessity of insulin (generally, inadequacy of oral medication). | Level 6 |
| Brod et al., 201432 | To identify patients’ beliefs as well as clinical realities about insulin that may be barriers to type 2 diabetes patients initiating insulin treatment | Population: 87 patients Women 37 Mean age: 52.9 years Methods: Purposive sample Mixed methods study 13 focus group in 5 different countries Measures: Qualitative data on attitudes through focus groups. Quantitative data were collected to understand better the factors influencing participants’ decisions about initiating insulin and patient-held beliefs regarding the process through the developed educational tool ‘questions about starting insulin: information on the myths, misconceptions and clinical realities about insulin’. | Patients’ reported the following key barriers to initiating insulin Treatment: 1.Insulin as a treatment of last resort 2. Insulin as evidence of personal failure to self-manage diabetes 3. Risk of long-term complications from insulin 4. Side effects of insulin 5. Treatment convenience 6. Needles and injections 7. Weight gain from insulin | Level 4 |
| Simon et al., 201433 | To identify experiences with and barriers to self-monitoring of blood glucose, insulin injection, and insulin titration among patients with type 2 diabetes | Population: 20 patients Group A: Patients who had never used computer-assisted insulin self-titration system Women 4 Mean age 53.9 years Group B: Patients who were enrolled in a 4-week pilot involving computer-assisted insulin self-titration system Women 4 Mean age 56.9 years Sampling method: In-depth, semi-structured interviews Face to face interviews for group A and telephone interviews for group B Design: Qualitative study Measures: Experiences with and barriers to insulin Self-management | Patients fear the lifelong commitment to insulin therapy and disease progression Barriers when implementing insulin therapy (e.g. perceived usefulness, physical impact, fear of injection) Difficulties increasing the insulin dose (fear of hypoglycaemia) Association of higher insulin doses with disease progression Ignorant of treatment targets Patients who never used a computer-assisted insulin self-titration system felt they had enough knowledge to know when their insulin should be adjusted, but still believed that the system advice would be useful to confirm their reasoning. | Level 6 |
| Iyer et al., 201334 | To investigate perceptions of and attitudes towards long-acting (once every 2 weeks) injectable antipsychotics among patients | Population: 34 patients Women 7 Methods: Qualitative study Focus groups Measures: Experiences with and attitudes toward LAI antipsychotic medication | 1. Awareness of and knowledge about LAI antipsychotics: Some patients had never heard about LAI antipsychotics, some others reported not having understood what was discussed with them regarding LAI antipsychotics and some patients had typically heard about. 2. Perceptions about LAI antipsychotics: Positive perceptions: Relapse prevention and reduced effort in ensuring adherence Negative perceptions: Financial costs and the inconvenience of appointments to receive injections a. Cost and convenience considerations b. Issues arising from the coercive context under which LAI antipsychotics were often prescribed | Level 6 |
| Potkin et al., 201311 | To understand better prescriber, patient and caregiver perspectives about LAI antipsychotics (administered once every 2 or 4 weeks) therapy and how these perspectives affect their use | Population: 22 patients Women 13 Mean age 45.7 years Methods: Qualitative Ethnographic information of non-random sample of prescriber–patient conversations. Also, in-person observations in mental health centres including home visits Telephone in-depth interviews for additional information Measures: Perspectives about LAI antipsychotic therapy How perspectives affect LAI use | Involvement of patients in treatment decisions was greater when discussing LAI antipsychotics versus oral antipsychotic treatment. LAI antipsychotics -naïve patients expressed neutral rather than favorable or unfavorable responses. Patient resistance was often related to negative feelings about injections. Patient-described benefits of LAI antipsychotics versus orals included perceived rapid symptom improvement and greater overall efficacy. | Level 6 |
| Tan et al., 201135 | To determine the issues relating to insulin initiation for diabetes patients managed in primary care polyclinics | Population: 11 patients Women 5 Methods: Qualitative study, focus groups Purposive sample (doctors and nurses from different training backgrounds and years of experience; poorly controlled diabetes patients who refused insulin therapy despite being on maximum oral hypoglycaemic drugs and patients who were on insulin therapy). Measures: Barriers to insulin commencement | 1. Launching the topic and doctor-patient communication on insulin therapy were key issues in insulin initiation. 2. Patient barriers to insulin commencement included: refusal to acknowledge the need for insulin therapy, its perception as a social stigma, an inconvenient mode of treatment or punishment for failure and fear of needles, side effects and complications and the healthcare professionals’ attitude and experience with insulin therapy. | Level 6 |
| Jenkings et al., 201036 | To explore patients and health professionals’ experiences of initiating insulin as part of the treating to target in DM | Population: 45 patients and 21 health professionals Women 16 Mean age 64.7 years Methods: Qualitative through interviews Purposive sample Measures: Interviews which explored participants understandings and experiences of insulin initiation | Patients reported the key factors that fostered resistance to insulin initiation: 1. Engagement with disease progression. Patients felt that they personally failed with diabetes management. 2. Managing anxieties about insulin therapy. Patients were anxious about the prospect of injecting but frequently they surprised when they discover that they can use insulin pens. | Level 6 |
| Karter et al., 201016 | To investigate barriers to insulin initiation following a new prescription | Population: 169 patients Adherent patients mean age 58 years Women 47% Non-adherent patients mean age 61 years 35% women Methods: Mixed methods Telephone interviews and self-administered survey Patients receiving a new electronic prescription for insulin. Random sample from pharmacy records Measures: Barriers to insulin initiation among non-adherent and adherent patients newly prescribed insulin | Non-adherent patients: Reasons for failing to initiate insulin included: the patient planned to change health behaviours instead of starting insulin, injection phobia, negative impact on work, concerns about long-term medication use, inconvenience and not believing insulin was needed. Believed that people who require insulin ‘have not taken care of themselves in the past’ and that ‘taking insulin can cause. . .’ other consequences. They believed insulin causes harm. Expressed significantly more concern about their inability to adjust insulin dosage, the impact on social life and work, injection pain, and side effects. Reported problems learning about their medical condition because of difficulty understanding written information and claimed providers failed to adequately explain insulin’s risk and benefits. Fewer non-adherent patients reported receiving insulin self-management training from their doctor, nurse, health educator, or a class. | Level 4 |
| Peyrot et al., 201037 | To access factors associated with patient frequency of intentionally skipping insulin injections | Population: 502 patients Women 226 Mean age 55 years Methods: Quantitative study Internet survey with a questionnaire developed for the particular survey. Measures: Disease type, duration, complications and treatment Perceived burden of insulin injections The experience of injections Negative affect toward insulin injections Frequency of skipping insulin injections | Patients who are not managing their diabetes are significantly more likely to see insulin therapy as potentially beneficial. Most nurses and general practitioners delay insulin therapy until absolutely necessary, but specialists and opinion leaders are less likely to do so. Delay of insulin therapy is significantly less likely when physicians and nurses see their patients as more adherent to medication or appointment regimens, view insulin as more efficacious, and when they are less likely to delay oral diabetes medications. | Level 6 |
| Rubin et al., 200910 | To compare patients’ perceptions of injection-related problems with clinicians estimates of those problems | Population: 501 patients Women 225 Mean age 54.9 years Methods: Quantitative through interviews Internet survey of self-identified patients with diabetes Measures: 1. Perceived burden of insulin injections 2. Effect of injections on quality of life 3. Effect of injection problems on adherence to treatment 4. Patient-provider injection-related communication 5. Injection-related support from provider 6. Interest in and knowledge of products to ease injection burden | The majority of patients would like to reduce the number of injections they take each day. Almost half said that they would be more likely to take their insulin injections regularly if a product were available to ease the pain. Patients also reported: 1. Injections were a serious burden 2. They were dissatisfied with the way they took insulin 3. Injections had a substantial negative impact on quality of life 4. They skipped injections they should take or 5. Injection-related problems affected the number of injections they were willing to take. Half of the patients said they mentioned injection-related problems to their provider; a similar number reported that their providers had not given them a solution to problems with injection-related pain and bruising. | Level 6 |
| Khan et al., 200838 | To determine the prevalence and reasons for refusal to commence insulin in Bangladeshi patients with type 2 diabetes | Population: 212 patients Women 100 Mean age 55.3 years Methods: Qualitative study through focus groups Data were analysed by thematic content analysis using the constant comparative method. Measures: Reasons of insulin refusal | Patients refused insulin due to: 1. Disease severity: perceptions that requirement for insulin was an indicator of a more serious stage of their condition 2. Insulin leading to premature death: common suggestion that commencing insulin led to early death 3. Loss of control: fear of hypoglycaemia, weight gain, loss of independence and reliance on others to give insulin or look for signs of hypoglycaemia 4. Lack of perception of benefits: poor perception of the benefits of improved glycaemic control on quality of life and cardiovascular risk 5. Needle anxiety: concern over frequent injections. | Level 6 |
| Larkin et al., 200839 | To explore the attitudes that contribute to psychological insulin resistance (PIR) in insulin-naive patients with type 2 diabetes and to identify predictors of PIR | Population: 100 patients Women 39 Mean age 62 years Methods: Quantitative study Self-administrative questionnaires Measures: 1. Survey for people who do not take insulin: reasons why people are reluctant to start insulin, including risk of side effects or complications and changes in lifestyle 2. ITAS: assessment of patients’ perceptions of insulin treatment 3. HADS: depression screening questionnaire | The most commonly expressed negative attitudes were concern regarding hypoglycaemia, permanent need for insulin therapy, less flexibility, and feelings of failure. Less than 40% expressed fear of self-injection or thought that injections were painful. Poorer general health and higher depression scores also correlated with PIR. | Level 6 |
| Hayes et al., 200640 | To explore diabetes medication experiences of patients with type 2 diabetes | Population: 138 patients Women 94 61% were using insulin Methods: Qualitative study through focus groups Measures: How patients experience their diabetes drug treatment What they dislike about treatment What makes it inconvenient or inflexible, intolerable, or unacceptable What factors contribute to their treatment satisfaction and treatment preference | Patients expressed: 1. Inconvenience and inflexibility of the timing and frequency of administrations of many diabetes medication regimens. 2. Avoidance of injections and/or insulin therapy 3. The physical and emotional side effects of diabetes medications. Treatment preferences: Participants would weigh the convenience and flexibility, route of administration, side effects, and cost of the medications. | Level 6 |
| Morris et al., 200541 | To elucidate the range of subjective experiences of men and women with type 2 diabetes who have recently gone on to insulin | Population: Six patients Women 3 Methods: Qualitative study Semi-structured interviews which were audiotape-recorded and transcribed. Transcripts were analysed together with the researcher’s observational notes and documentary evidence (phenomenological analysis) Purposive sample Measures: Experiences of patients with DM | Patients experienced a range of initial reactions (from shock and anger, to relief) and perceptions of insulin, sometimes resulting in an altered self-image. Perceptions for insulin were shown to change over time, with some patients eventually accepting insulin and becoming empowered. | Level 6 |
| Mollema et al., 200142 | To define clinically relevant cut-off points for severe fear of self-injecting and self-treated phobia in insulin-treated patients with diabetes and to estimate the magnitude of these phobias in our research population | Population: 24 insulin-treated adult diabetes patients Women 17 Mean age 44.5 years Methods: Quantitative study Cross-sectional survey Purposive sample (high-scorers on FSI and/or FST) Measures: Relevance of fear of self-injecting (FSI) and self-testing (FST) (phobia) in insulin-treated patients with diabetes D-FISQ and BAT questionnaires | Severe FSI and FST, characterised by emotional distress and avoidance behaviour, seems to occur in a small group of insulin-treated patients with diabetes | Level 6 |
| Author/year . | Study purpose . | Methods . | Findings . | Level of evidence . |
|---|---|---|---|---|
| Campbell et al., 201728 | To understand better the impact that financial barriers have on patients with diabetes and the strategies that they use to cope with them | Population: 24 patients (10 men and 14 women) including 10 who used insulin Mean age men 59.1 years Mean age women 56.5 years Methods: Secondary analysis of 24 interviews of patients with diabetes and perceived financial barriers Semi-structured interviews were undertaken either face-to-face or by telephone Data analysis was performed using inductive thematic analysis. Measures: Qualitative data: Personal interviews exploring the following domains: Experience of living with diabetes Experience of having financial barriers erceived reasons for financial barriers Perceived consequences of financial barriers Mechanisms for overcoming financial barriers | The predominant aspects of care to which participants described financial barriers were medications, diabetes supplies and healthy food. Participants described that health professionals had the potential to either play an important supporting role; or alternatively, that they could also worsen the impacts of financial barriers. | Level 6 |
| Taylor et al., 201729 | To document in people with DM attitudes and beliefs that may result in psychological insulin resistance | Population: 117 patients Women 80 Mean age 66 years Methods: Quantitative through an interview administrated questionnaire Telephone interviews Measures: Attitudes and beliefs towards insulin (ITAS questionnaire) | Negative perceptions about insulin use 1. Meant a worsening of diabetes (68%) 2. Would worry family (63%) 3. Feared self-injection (58%) 4. Meant a failure in self-management (57%) 5. Injections were painful (54%) 6. Would be seen as being sicker (46%) 7. Increased hypoglycaemia risk (38%) 8. Required effort (34%) 9. Causes weight gain (27%) 10. Causes a deterioration in health (14%) 11. Would have to give up enjoyable activities (10%) Positive perceptions • Helps good glycaemic control (78%) • Would prevent complications (61%) • Improves health (58%) Patients using insulin had fewer negative perceptions than those not on insulin. | Level 6 |
| Taylor et al., 201630 | To explore self-reported knowledge and attitudes to insulin treatment among a group of adults with poorly controlled diabetes | Population: 29 patients Women 14 Methods: Quantitative study Cross-sectional study Measures: Insulin treatment Appraisal scale (ITAS) and barriers to insulin treatment Questionnaire (BITQ) scores related to knowledge and attitudes to insulin treatment, clinical and demographic measures | Perceived barriers are higher among older patients with fewer years of formal education. Low score in ‘knowledge’ items in the ITAS. | Level 6 |
| Victor Spain et al., 201614 | To explore the barriers that adult Americans experience when taking injectable medications for type 2 diabetes, from the time of filling the initial prescription through the decision to discontinue the medication | Population: 1190 patients Women 986 Methods: Quantitative using self-administrated questionnaire developed for the survey and DES Internet-based survey. Measures: Patients were asked: 1. If they filled the medication of interest when first prescribed, time until filling the prescription and if filled, how long until they started taking it 2. About their reactions to being prescribed an injectable 3. For those initiating the medication of interest, if they discontinued using it 4. For those discontinuing the medication of interest, the reasons for discontinuing use and the decision-making process for discontinuation 5. If still taking the medication of interest, what barriers (if any) to taking it they experienced | Among patients who delayed filling their prescription by more than one week, cost was a common reason for delay. The most commonly reported barrier to maintaining injectable medication was injection concerns (42%) such as aversion to needles, pain or needle size. Lack of perceived need was the most common reason for discontinuation for basal (47%) and prandial/premixed (44%) insulin. For liraglutide, the most common reason for discontinuation was experiencing an adverse event (33%), for exenatide once weekly, it was injection concerns such as aversion to needles, pain, or needle size (38%). | Level 6 |
| Papaspurou et al., 201531 | To investigate the health needs and self-management problems faced by patients with diabetes daily | Population: 15 patients Women 9 Methods: Qualitative study Sem-structured interviews (interpretative phenomenological approach) Measures: Health needs and self-management problems faced by patients with DM | Patients face fears and have unaddressed needs related to the diagnosis, treatment, expected impacts, prognosis and the daily management of the disease. Patients have several care needs; need of psychological support and education to recognize and prevent hypoglycaemia. Need of continuous education and communication with health professionals. | Level 6 |
| Patel et al., 201515 | To explore attitudes towards insulin acceptance an ethnically diverse population of people with type 2 diabetes | Population: 18 patients Women 9 Methods: Qualitative study Semi-structured interviews Purposive sampling Measures: Concerns, views and beliefs about the necessity of insulin | Decisions about accepting insulin involved balancing concerns against the perceived necessity of insulin (generally, inadequacy of oral medication). | Level 6 |
| Brod et al., 201432 | To identify patients’ beliefs as well as clinical realities about insulin that may be barriers to type 2 diabetes patients initiating insulin treatment | Population: 87 patients Women 37 Mean age: 52.9 years Methods: Purposive sample Mixed methods study 13 focus group in 5 different countries Measures: Qualitative data on attitudes through focus groups. Quantitative data were collected to understand better the factors influencing participants’ decisions about initiating insulin and patient-held beliefs regarding the process through the developed educational tool ‘questions about starting insulin: information on the myths, misconceptions and clinical realities about insulin’. | Patients’ reported the following key barriers to initiating insulin Treatment: 1.Insulin as a treatment of last resort 2. Insulin as evidence of personal failure to self-manage diabetes 3. Risk of long-term complications from insulin 4. Side effects of insulin 5. Treatment convenience 6. Needles and injections 7. Weight gain from insulin | Level 4 |
| Simon et al., 201433 | To identify experiences with and barriers to self-monitoring of blood glucose, insulin injection, and insulin titration among patients with type 2 diabetes | Population: 20 patients Group A: Patients who had never used computer-assisted insulin self-titration system Women 4 Mean age 53.9 years Group B: Patients who were enrolled in a 4-week pilot involving computer-assisted insulin self-titration system Women 4 Mean age 56.9 years Sampling method: In-depth, semi-structured interviews Face to face interviews for group A and telephone interviews for group B Design: Qualitative study Measures: Experiences with and barriers to insulin Self-management | Patients fear the lifelong commitment to insulin therapy and disease progression Barriers when implementing insulin therapy (e.g. perceived usefulness, physical impact, fear of injection) Difficulties increasing the insulin dose (fear of hypoglycaemia) Association of higher insulin doses with disease progression Ignorant of treatment targets Patients who never used a computer-assisted insulin self-titration system felt they had enough knowledge to know when their insulin should be adjusted, but still believed that the system advice would be useful to confirm their reasoning. | Level 6 |
| Iyer et al., 201334 | To investigate perceptions of and attitudes towards long-acting (once every 2 weeks) injectable antipsychotics among patients | Population: 34 patients Women 7 Methods: Qualitative study Focus groups Measures: Experiences with and attitudes toward LAI antipsychotic medication | 1. Awareness of and knowledge about LAI antipsychotics: Some patients had never heard about LAI antipsychotics, some others reported not having understood what was discussed with them regarding LAI antipsychotics and some patients had typically heard about. 2. Perceptions about LAI antipsychotics: Positive perceptions: Relapse prevention and reduced effort in ensuring adherence Negative perceptions: Financial costs and the inconvenience of appointments to receive injections a. Cost and convenience considerations b. Issues arising from the coercive context under which LAI antipsychotics were often prescribed | Level 6 |
| Potkin et al., 201311 | To understand better prescriber, patient and caregiver perspectives about LAI antipsychotics (administered once every 2 or 4 weeks) therapy and how these perspectives affect their use | Population: 22 patients Women 13 Mean age 45.7 years Methods: Qualitative Ethnographic information of non-random sample of prescriber–patient conversations. Also, in-person observations in mental health centres including home visits Telephone in-depth interviews for additional information Measures: Perspectives about LAI antipsychotic therapy How perspectives affect LAI use | Involvement of patients in treatment decisions was greater when discussing LAI antipsychotics versus oral antipsychotic treatment. LAI antipsychotics -naïve patients expressed neutral rather than favorable or unfavorable responses. Patient resistance was often related to negative feelings about injections. Patient-described benefits of LAI antipsychotics versus orals included perceived rapid symptom improvement and greater overall efficacy. | Level 6 |
| Tan et al., 201135 | To determine the issues relating to insulin initiation for diabetes patients managed in primary care polyclinics | Population: 11 patients Women 5 Methods: Qualitative study, focus groups Purposive sample (doctors and nurses from different training backgrounds and years of experience; poorly controlled diabetes patients who refused insulin therapy despite being on maximum oral hypoglycaemic drugs and patients who were on insulin therapy). Measures: Barriers to insulin commencement | 1. Launching the topic and doctor-patient communication on insulin therapy were key issues in insulin initiation. 2. Patient barriers to insulin commencement included: refusal to acknowledge the need for insulin therapy, its perception as a social stigma, an inconvenient mode of treatment or punishment for failure and fear of needles, side effects and complications and the healthcare professionals’ attitude and experience with insulin therapy. | Level 6 |
| Jenkings et al., 201036 | To explore patients and health professionals’ experiences of initiating insulin as part of the treating to target in DM | Population: 45 patients and 21 health professionals Women 16 Mean age 64.7 years Methods: Qualitative through interviews Purposive sample Measures: Interviews which explored participants understandings and experiences of insulin initiation | Patients reported the key factors that fostered resistance to insulin initiation: 1. Engagement with disease progression. Patients felt that they personally failed with diabetes management. 2. Managing anxieties about insulin therapy. Patients were anxious about the prospect of injecting but frequently they surprised when they discover that they can use insulin pens. | Level 6 |
| Karter et al., 201016 | To investigate barriers to insulin initiation following a new prescription | Population: 169 patients Adherent patients mean age 58 years Women 47% Non-adherent patients mean age 61 years 35% women Methods: Mixed methods Telephone interviews and self-administered survey Patients receiving a new electronic prescription for insulin. Random sample from pharmacy records Measures: Barriers to insulin initiation among non-adherent and adherent patients newly prescribed insulin | Non-adherent patients: Reasons for failing to initiate insulin included: the patient planned to change health behaviours instead of starting insulin, injection phobia, negative impact on work, concerns about long-term medication use, inconvenience and not believing insulin was needed. Believed that people who require insulin ‘have not taken care of themselves in the past’ and that ‘taking insulin can cause. . .’ other consequences. They believed insulin causes harm. Expressed significantly more concern about their inability to adjust insulin dosage, the impact on social life and work, injection pain, and side effects. Reported problems learning about their medical condition because of difficulty understanding written information and claimed providers failed to adequately explain insulin’s risk and benefits. Fewer non-adherent patients reported receiving insulin self-management training from their doctor, nurse, health educator, or a class. | Level 4 |
| Peyrot et al., 201037 | To access factors associated with patient frequency of intentionally skipping insulin injections | Population: 502 patients Women 226 Mean age 55 years Methods: Quantitative study Internet survey with a questionnaire developed for the particular survey. Measures: Disease type, duration, complications and treatment Perceived burden of insulin injections The experience of injections Negative affect toward insulin injections Frequency of skipping insulin injections | Patients who are not managing their diabetes are significantly more likely to see insulin therapy as potentially beneficial. Most nurses and general practitioners delay insulin therapy until absolutely necessary, but specialists and opinion leaders are less likely to do so. Delay of insulin therapy is significantly less likely when physicians and nurses see their patients as more adherent to medication or appointment regimens, view insulin as more efficacious, and when they are less likely to delay oral diabetes medications. | Level 6 |
| Rubin et al., 200910 | To compare patients’ perceptions of injection-related problems with clinicians estimates of those problems | Population: 501 patients Women 225 Mean age 54.9 years Methods: Quantitative through interviews Internet survey of self-identified patients with diabetes Measures: 1. Perceived burden of insulin injections 2. Effect of injections on quality of life 3. Effect of injection problems on adherence to treatment 4. Patient-provider injection-related communication 5. Injection-related support from provider 6. Interest in and knowledge of products to ease injection burden | The majority of patients would like to reduce the number of injections they take each day. Almost half said that they would be more likely to take their insulin injections regularly if a product were available to ease the pain. Patients also reported: 1. Injections were a serious burden 2. They were dissatisfied with the way they took insulin 3. Injections had a substantial negative impact on quality of life 4. They skipped injections they should take or 5. Injection-related problems affected the number of injections they were willing to take. Half of the patients said they mentioned injection-related problems to their provider; a similar number reported that their providers had not given them a solution to problems with injection-related pain and bruising. | Level 6 |
| Khan et al., 200838 | To determine the prevalence and reasons for refusal to commence insulin in Bangladeshi patients with type 2 diabetes | Population: 212 patients Women 100 Mean age 55.3 years Methods: Qualitative study through focus groups Data were analysed by thematic content analysis using the constant comparative method. Measures: Reasons of insulin refusal | Patients refused insulin due to: 1. Disease severity: perceptions that requirement for insulin was an indicator of a more serious stage of their condition 2. Insulin leading to premature death: common suggestion that commencing insulin led to early death 3. Loss of control: fear of hypoglycaemia, weight gain, loss of independence and reliance on others to give insulin or look for signs of hypoglycaemia 4. Lack of perception of benefits: poor perception of the benefits of improved glycaemic control on quality of life and cardiovascular risk 5. Needle anxiety: concern over frequent injections. | Level 6 |
| Larkin et al., 200839 | To explore the attitudes that contribute to psychological insulin resistance (PIR) in insulin-naive patients with type 2 diabetes and to identify predictors of PIR | Population: 100 patients Women 39 Mean age 62 years Methods: Quantitative study Self-administrative questionnaires Measures: 1. Survey for people who do not take insulin: reasons why people are reluctant to start insulin, including risk of side effects or complications and changes in lifestyle 2. ITAS: assessment of patients’ perceptions of insulin treatment 3. HADS: depression screening questionnaire | The most commonly expressed negative attitudes were concern regarding hypoglycaemia, permanent need for insulin therapy, less flexibility, and feelings of failure. Less than 40% expressed fear of self-injection or thought that injections were painful. Poorer general health and higher depression scores also correlated with PIR. | Level 6 |
| Hayes et al., 200640 | To explore diabetes medication experiences of patients with type 2 diabetes | Population: 138 patients Women 94 61% were using insulin Methods: Qualitative study through focus groups Measures: How patients experience their diabetes drug treatment What they dislike about treatment What makes it inconvenient or inflexible, intolerable, or unacceptable What factors contribute to their treatment satisfaction and treatment preference | Patients expressed: 1. Inconvenience and inflexibility of the timing and frequency of administrations of many diabetes medication regimens. 2. Avoidance of injections and/or insulin therapy 3. The physical and emotional side effects of diabetes medications. Treatment preferences: Participants would weigh the convenience and flexibility, route of administration, side effects, and cost of the medications. | Level 6 |
| Morris et al., 200541 | To elucidate the range of subjective experiences of men and women with type 2 diabetes who have recently gone on to insulin | Population: Six patients Women 3 Methods: Qualitative study Semi-structured interviews which were audiotape-recorded and transcribed. Transcripts were analysed together with the researcher’s observational notes and documentary evidence (phenomenological analysis) Purposive sample Measures: Experiences of patients with DM | Patients experienced a range of initial reactions (from shock and anger, to relief) and perceptions of insulin, sometimes resulting in an altered self-image. Perceptions for insulin were shown to change over time, with some patients eventually accepting insulin and becoming empowered. | Level 6 |
| Mollema et al., 200142 | To define clinically relevant cut-off points for severe fear of self-injecting and self-treated phobia in insulin-treated patients with diabetes and to estimate the magnitude of these phobias in our research population | Population: 24 insulin-treated adult diabetes patients Women 17 Mean age 44.5 years Methods: Quantitative study Cross-sectional survey Purposive sample (high-scorers on FSI and/or FST) Measures: Relevance of fear of self-injecting (FSI) and self-testing (FST) (phobia) in insulin-treated patients with diabetes D-FISQ and BAT questionnaires | Severe FSI and FST, characterised by emotional distress and avoidance behaviour, seems to occur in a small group of insulin-treated patients with diabetes | Level 6 |
LAI: long-acting injectable; ITAS: insulin treatment appraisal scale; BITQ: barriers to insulin treatment questionnaire; DES: diabetes empowerment scale; DM: diabetes mellitus; HADS: hospital anxiety and depression scale; D-FISQ: diabetes fear of injecting and self-testing questionnaire; BAT: behavioural avoidance test.
Results
The aim of this integrative review was to identify the facilitators, barriers and perceptions in delivering and managing injectable therapies from patients’ perspective, and 20 studies were identified. The majority of the studies were undertaken in the USA (6/20),11,12,14,16,29,30 four in the UK15,31,–33 two in Canada34,35 and two in The Netherlands.36,37 One study was conducted in each of the following countries: Australia,38 Greece,39 Barbados40 and Singapore.41 Two studies were multicentre and conducted in 1342 and five43 different countries.
Eleven of the studies followed qualitative methodology,12,15,29,31,,,–35,37,39,41 seven were quantitative11,14,30,36,38,40,42 and two studies were mixed methods.16,43 The sample of the studies ranged from eight to 1190 patients (Table 2).
| Authors . | Publication year . | Country . | Study design . | Aim . | Injectable medicine used . |
|---|---|---|---|---|---|
| Campbell et al. | 2017 | Canada | Qualitative study | To understand better the impact that financial barriers have on patients with diabetes and the strategies that they use to cope with them | Insulin injections |
| Taylor et al. | 2017 | Barbados | Quantitative study | To document in people with type 2 diabetes in Barbados attitudes and beliefs that may result in psychological insulin resistance | Insulin injections |
| Taylor et al. | 2016 | Australia | Quantitative study | To explore self-reported knowledge and attitudes to insulin treatment among a group of adults with poorly controlled diabetes in the Torres Strait islands | Insulin injections |
| Victor Spain et al. | 2016 | USA | Quantitative study | To explore the barriers that adult Americans experience when taking injectable medications for type 2 diabetes, from the time of filling the initial prescription to the decision to discontinue the medication | GLP-1 agonists injections |
| Papaspurou et al. | 2015 | Greece | Qualitative study | To investigate the health needs and self-management problems faced by patients with diabetes daily, especially those who use insulin | Insulin injections |
| Patel et al. | 2015 | UK | Qualitative study | To explore attitudes towards insulin acceptance in an ethnically diverse population of people with type 2 diabetes | Insulin injections |
| Brod et al. | 2014 | Multicentre Germany, Sweden, The Netherlands, UK and USA | Mixed methods | To identify patient beliefs as well as clinical realities about insulin that may be barriers to type 2 diabetes patients initiating insulin treatment | Insulin injections |
| Simon et al. | 2014 | The Netherlands | Qualitative study | To identify experiences with and barriers to self-monitoring of blood glucose, insulin injection, and insulin titration among patients with type 2 diabetes | Insulin injections |
| Iyer et al | 2013 | Canada | Qualitative study | To investigate perceptions of and attitudes toward long-acting injectable antipsychotics among patients in Canada. | Long-term Injectable antipsychotics |
| Potkin et al. | 2013 | USA | Qualitative study | To understand better prescriber, patient and caregiver perspectives about long-acting injectable antipsychotic therapy and how these perspectives affect their use | Long-term injectable antipsychotics |
| Tan et al. | 2011 | Singapore | Qualitative study | To determine the issues relating to insulin initiation for diabetes patients managed in primary care polyclinics in Singapore | Insulin injections |
| Jenkings et al. | 2010 | UK | Qualitative study | To explore patients and health professionals’ experiences of initiating insulin as part of the Treating to Target in Type 2 Diabetes (4-T) randomised controlled trial | Insulin injections |
| Karter et al. | 2010 | USA | Mixed method study | To investigate barriers to insulin initiation following a new prescription | Insulin injections |
| Peyrot et al. | 2010 | Multicentre Australia, France, Germany, India, Japan, The Netherlands, Poland, Scandinavia (divided equally among Sweden, Denmark and Norway), Spain, UK and USA | Quantitative study | To access factors associated with patient frequency of intentionally skipping insulin injections | Insulin injections |
| Rubin et al. | 2009 | USA | Quantitative study | To compare patients’ perceptions of injection-related problems with clinicians’ estimates of those problems | Insulin injections |
| Khan et al. | 2008 | UK | Qualitative study | To determine the prevalence and reasons for refusal to start insulin in Bangladeshi patients with type 2 diabetes | Insulin injections |
| Larkin et al. | 2008 | USA | Quantitative study | To explore the attitudes that contribute to psychological insulin resistance (PIR) in insulin-naive patients with type 2 diabetes and to identify predictors of PIR | Insulin injections |
| Hayes et al. | 2006 | USA | Qualitative study | To explore diabetes medication experiences of patients with type 2 diabetes | Insulin injections |
| Morris et al. | 2005 | UK | Qualitative study | To elucidate the range of subjective experiences of men and women with type 2 diabetes who have recently gone on to insulin | Insulin injections |
| Mollema et al. | 2001 | The Netherlands | Quantitative study | To define clinically relevant cut-off points for severe fear of self-injecting and self-testing phobia in insulin-treated patients with diabetes and to estimate the magnitude of these phobias in our research population | Insulin injections |
| Authors . | Publication year . | Country . | Study design . | Aim . | Injectable medicine used . |
|---|---|---|---|---|---|
| Campbell et al. | 2017 | Canada | Qualitative study | To understand better the impact that financial barriers have on patients with diabetes and the strategies that they use to cope with them | Insulin injections |
| Taylor et al. | 2017 | Barbados | Quantitative study | To document in people with type 2 diabetes in Barbados attitudes and beliefs that may result in psychological insulin resistance | Insulin injections |
| Taylor et al. | 2016 | Australia | Quantitative study | To explore self-reported knowledge and attitudes to insulin treatment among a group of adults with poorly controlled diabetes in the Torres Strait islands | Insulin injections |
| Victor Spain et al. | 2016 | USA | Quantitative study | To explore the barriers that adult Americans experience when taking injectable medications for type 2 diabetes, from the time of filling the initial prescription to the decision to discontinue the medication | GLP-1 agonists injections |
| Papaspurou et al. | 2015 | Greece | Qualitative study | To investigate the health needs and self-management problems faced by patients with diabetes daily, especially those who use insulin | Insulin injections |
| Patel et al. | 2015 | UK | Qualitative study | To explore attitudes towards insulin acceptance in an ethnically diverse population of people with type 2 diabetes | Insulin injections |
| Brod et al. | 2014 | Multicentre Germany, Sweden, The Netherlands, UK and USA | Mixed methods | To identify patient beliefs as well as clinical realities about insulin that may be barriers to type 2 diabetes patients initiating insulin treatment | Insulin injections |
| Simon et al. | 2014 | The Netherlands | Qualitative study | To identify experiences with and barriers to self-monitoring of blood glucose, insulin injection, and insulin titration among patients with type 2 diabetes | Insulin injections |
| Iyer et al | 2013 | Canada | Qualitative study | To investigate perceptions of and attitudes toward long-acting injectable antipsychotics among patients in Canada. | Long-term Injectable antipsychotics |
| Potkin et al. | 2013 | USA | Qualitative study | To understand better prescriber, patient and caregiver perspectives about long-acting injectable antipsychotic therapy and how these perspectives affect their use | Long-term injectable antipsychotics |
| Tan et al. | 2011 | Singapore | Qualitative study | To determine the issues relating to insulin initiation for diabetes patients managed in primary care polyclinics in Singapore | Insulin injections |
| Jenkings et al. | 2010 | UK | Qualitative study | To explore patients and health professionals’ experiences of initiating insulin as part of the Treating to Target in Type 2 Diabetes (4-T) randomised controlled trial | Insulin injections |
| Karter et al. | 2010 | USA | Mixed method study | To investigate barriers to insulin initiation following a new prescription | Insulin injections |
| Peyrot et al. | 2010 | Multicentre Australia, France, Germany, India, Japan, The Netherlands, Poland, Scandinavia (divided equally among Sweden, Denmark and Norway), Spain, UK and USA | Quantitative study | To access factors associated with patient frequency of intentionally skipping insulin injections | Insulin injections |
| Rubin et al. | 2009 | USA | Quantitative study | To compare patients’ perceptions of injection-related problems with clinicians’ estimates of those problems | Insulin injections |
| Khan et al. | 2008 | UK | Qualitative study | To determine the prevalence and reasons for refusal to start insulin in Bangladeshi patients with type 2 diabetes | Insulin injections |
| Larkin et al. | 2008 | USA | Quantitative study | To explore the attitudes that contribute to psychological insulin resistance (PIR) in insulin-naive patients with type 2 diabetes and to identify predictors of PIR | Insulin injections |
| Hayes et al. | 2006 | USA | Qualitative study | To explore diabetes medication experiences of patients with type 2 diabetes | Insulin injections |
| Morris et al. | 2005 | UK | Qualitative study | To elucidate the range of subjective experiences of men and women with type 2 diabetes who have recently gone on to insulin | Insulin injections |
| Mollema et al. | 2001 | The Netherlands | Quantitative study | To define clinically relevant cut-off points for severe fear of self-injecting and self-testing phobia in insulin-treated patients with diabetes and to estimate the magnitude of these phobias in our research population | Insulin injections |
| Authors . | Publication year . | Country . | Study design . | Aim . | Injectable medicine used . |
|---|---|---|---|---|---|
| Campbell et al. | 2017 | Canada | Qualitative study | To understand better the impact that financial barriers have on patients with diabetes and the strategies that they use to cope with them | Insulin injections |
| Taylor et al. | 2017 | Barbados | Quantitative study | To document in people with type 2 diabetes in Barbados attitudes and beliefs that may result in psychological insulin resistance | Insulin injections |
| Taylor et al. | 2016 | Australia | Quantitative study | To explore self-reported knowledge and attitudes to insulin treatment among a group of adults with poorly controlled diabetes in the Torres Strait islands | Insulin injections |
| Victor Spain et al. | 2016 | USA | Quantitative study | To explore the barriers that adult Americans experience when taking injectable medications for type 2 diabetes, from the time of filling the initial prescription to the decision to discontinue the medication | GLP-1 agonists injections |
| Papaspurou et al. | 2015 | Greece | Qualitative study | To investigate the health needs and self-management problems faced by patients with diabetes daily, especially those who use insulin | Insulin injections |
| Patel et al. | 2015 | UK | Qualitative study | To explore attitudes towards insulin acceptance in an ethnically diverse population of people with type 2 diabetes | Insulin injections |
| Brod et al. | 2014 | Multicentre Germany, Sweden, The Netherlands, UK and USA | Mixed methods | To identify patient beliefs as well as clinical realities about insulin that may be barriers to type 2 diabetes patients initiating insulin treatment | Insulin injections |
| Simon et al. | 2014 | The Netherlands | Qualitative study | To identify experiences with and barriers to self-monitoring of blood glucose, insulin injection, and insulin titration among patients with type 2 diabetes | Insulin injections |
| Iyer et al | 2013 | Canada | Qualitative study | To investigate perceptions of and attitudes toward long-acting injectable antipsychotics among patients in Canada. | Long-term Injectable antipsychotics |
| Potkin et al. | 2013 | USA | Qualitative study | To understand better prescriber, patient and caregiver perspectives about long-acting injectable antipsychotic therapy and how these perspectives affect their use | Long-term injectable antipsychotics |
| Tan et al. | 2011 | Singapore | Qualitative study | To determine the issues relating to insulin initiation for diabetes patients managed in primary care polyclinics in Singapore | Insulin injections |
| Jenkings et al. | 2010 | UK | Qualitative study | To explore patients and health professionals’ experiences of initiating insulin as part of the Treating to Target in Type 2 Diabetes (4-T) randomised controlled trial | Insulin injections |
| Karter et al. | 2010 | USA | Mixed method study | To investigate barriers to insulin initiation following a new prescription | Insulin injections |
| Peyrot et al. | 2010 | Multicentre Australia, France, Germany, India, Japan, The Netherlands, Poland, Scandinavia (divided equally among Sweden, Denmark and Norway), Spain, UK and USA | Quantitative study | To access factors associated with patient frequency of intentionally skipping insulin injections | Insulin injections |
| Rubin et al. | 2009 | USA | Quantitative study | To compare patients’ perceptions of injection-related problems with clinicians’ estimates of those problems | Insulin injections |
| Khan et al. | 2008 | UK | Qualitative study | To determine the prevalence and reasons for refusal to start insulin in Bangladeshi patients with type 2 diabetes | Insulin injections |
| Larkin et al. | 2008 | USA | Quantitative study | To explore the attitudes that contribute to psychological insulin resistance (PIR) in insulin-naive patients with type 2 diabetes and to identify predictors of PIR | Insulin injections |
| Hayes et al. | 2006 | USA | Qualitative study | To explore diabetes medication experiences of patients with type 2 diabetes | Insulin injections |
| Morris et al. | 2005 | UK | Qualitative study | To elucidate the range of subjective experiences of men and women with type 2 diabetes who have recently gone on to insulin | Insulin injections |
| Mollema et al. | 2001 | The Netherlands | Quantitative study | To define clinically relevant cut-off points for severe fear of self-injecting and self-testing phobia in insulin-treated patients with diabetes and to estimate the magnitude of these phobias in our research population | Insulin injections |
| Authors . | Publication year . | Country . | Study design . | Aim . | Injectable medicine used . |
|---|---|---|---|---|---|
| Campbell et al. | 2017 | Canada | Qualitative study | To understand better the impact that financial barriers have on patients with diabetes and the strategies that they use to cope with them | Insulin injections |
| Taylor et al. | 2017 | Barbados | Quantitative study | To document in people with type 2 diabetes in Barbados attitudes and beliefs that may result in psychological insulin resistance | Insulin injections |
| Taylor et al. | 2016 | Australia | Quantitative study | To explore self-reported knowledge and attitudes to insulin treatment among a group of adults with poorly controlled diabetes in the Torres Strait islands | Insulin injections |
| Victor Spain et al. | 2016 | USA | Quantitative study | To explore the barriers that adult Americans experience when taking injectable medications for type 2 diabetes, from the time of filling the initial prescription to the decision to discontinue the medication | GLP-1 agonists injections |
| Papaspurou et al. | 2015 | Greece | Qualitative study | To investigate the health needs and self-management problems faced by patients with diabetes daily, especially those who use insulin | Insulin injections |
| Patel et al. | 2015 | UK | Qualitative study | To explore attitudes towards insulin acceptance in an ethnically diverse population of people with type 2 diabetes | Insulin injections |
| Brod et al. | 2014 | Multicentre Germany, Sweden, The Netherlands, UK and USA | Mixed methods | To identify patient beliefs as well as clinical realities about insulin that may be barriers to type 2 diabetes patients initiating insulin treatment | Insulin injections |
| Simon et al. | 2014 | The Netherlands | Qualitative study | To identify experiences with and barriers to self-monitoring of blood glucose, insulin injection, and insulin titration among patients with type 2 diabetes | Insulin injections |
| Iyer et al | 2013 | Canada | Qualitative study | To investigate perceptions of and attitudes toward long-acting injectable antipsychotics among patients in Canada. | Long-term Injectable antipsychotics |
| Potkin et al. | 2013 | USA | Qualitative study | To understand better prescriber, patient and caregiver perspectives about long-acting injectable antipsychotic therapy and how these perspectives affect their use | Long-term injectable antipsychotics |
| Tan et al. | 2011 | Singapore | Qualitative study | To determine the issues relating to insulin initiation for diabetes patients managed in primary care polyclinics in Singapore | Insulin injections |
| Jenkings et al. | 2010 | UK | Qualitative study | To explore patients and health professionals’ experiences of initiating insulin as part of the Treating to Target in Type 2 Diabetes (4-T) randomised controlled trial | Insulin injections |
| Karter et al. | 2010 | USA | Mixed method study | To investigate barriers to insulin initiation following a new prescription | Insulin injections |
| Peyrot et al. | 2010 | Multicentre Australia, France, Germany, India, Japan, The Netherlands, Poland, Scandinavia (divided equally among Sweden, Denmark and Norway), Spain, UK and USA | Quantitative study | To access factors associated with patient frequency of intentionally skipping insulin injections | Insulin injections |
| Rubin et al. | 2009 | USA | Quantitative study | To compare patients’ perceptions of injection-related problems with clinicians’ estimates of those problems | Insulin injections |
| Khan et al. | 2008 | UK | Qualitative study | To determine the prevalence and reasons for refusal to start insulin in Bangladeshi patients with type 2 diabetes | Insulin injections |
| Larkin et al. | 2008 | USA | Quantitative study | To explore the attitudes that contribute to psychological insulin resistance (PIR) in insulin-naive patients with type 2 diabetes and to identify predictors of PIR | Insulin injections |
| Hayes et al. | 2006 | USA | Qualitative study | To explore diabetes medication experiences of patients with type 2 diabetes | Insulin injections |
| Morris et al. | 2005 | UK | Qualitative study | To elucidate the range of subjective experiences of men and women with type 2 diabetes who have recently gone on to insulin | Insulin injections |
| Mollema et al. | 2001 | The Netherlands | Quantitative study | To define clinically relevant cut-off points for severe fear of self-injecting and self-testing phobia in insulin-treated patients with diabetes and to estimate the magnitude of these phobias in our research population | Insulin injections |
Facilitators to injectable therapy
The facilitators to injectable therapy, both initiation and adherence, of patients who were eligible to take injectables or were already taking injectable therapy, were studied in eight of the 20 studies included in the current review (Table 3).14,29,33,35,37,38,40,43 Injectable therapies were described in terms of the initiation of treatment as well as adherence and persistence once started.
| Article . | Health improvement . | Quick and long acting . | Convenient on management . | Taking control of their disease . | Less anxious, easier to take . | More effective . | Prevents complications . |
|---|---|---|---|---|---|---|---|
| Campbell et al., 2017 | |||||||
| Taylor et al., 2017 | X | X | X | ||||
| Taylor et al., 2016 | X | X | X | ||||
| Victor Spain et al., 2016 | X | X | X | ||||
| Papaspurou et al., 2015 | |||||||
| Patel et al., 2015 | |||||||
| Brod et al., 2014 | X | X | X | X | |||
| Simon et al., 2014 | X | ||||||
| Iyer et al., 2013 | X | X | X | X | |||
| Potkin et al., 2013 | |||||||
| Tan et al., 2011 | |||||||
| Jenkings et al., 2010 | |||||||
| Karter et al., 2010 | |||||||
| Peyrot et al., 2010 | |||||||
| Rubin et al., 2009 | |||||||
| Khan et al., 2008 | |||||||
| Larkin et al., 2008 | |||||||
| Hayes et al., 2006 | X | X | X | ||||
| Morris et al., 2005 | X | X | X | X | |||
| Mollema et al., 2001 |
| Article . | Health improvement . | Quick and long acting . | Convenient on management . | Taking control of their disease . | Less anxious, easier to take . | More effective . | Prevents complications . |
|---|---|---|---|---|---|---|---|
| Campbell et al., 2017 | |||||||
| Taylor et al., 2017 | X | X | X | ||||
| Taylor et al., 2016 | X | X | X | ||||
| Victor Spain et al., 2016 | X | X | X | ||||
| Papaspurou et al., 2015 | |||||||
| Patel et al., 2015 | |||||||
| Brod et al., 2014 | X | X | X | X | |||
| Simon et al., 2014 | X | ||||||
| Iyer et al., 2013 | X | X | X | X | |||
| Potkin et al., 2013 | |||||||
| Tan et al., 2011 | |||||||
| Jenkings et al., 2010 | |||||||
| Karter et al., 2010 | |||||||
| Peyrot et al., 2010 | |||||||
| Rubin et al., 2009 | |||||||
| Khan et al., 2008 | |||||||
| Larkin et al., 2008 | |||||||
| Hayes et al., 2006 | X | X | X | ||||
| Morris et al., 2005 | X | X | X | X | |||
| Mollema et al., 2001 |
| Article . | Health improvement . | Quick and long acting . | Convenient on management . | Taking control of their disease . | Less anxious, easier to take . | More effective . | Prevents complications . |
|---|---|---|---|---|---|---|---|
| Campbell et al., 2017 | |||||||
| Taylor et al., 2017 | X | X | X | ||||
| Taylor et al., 2016 | X | X | X | ||||
| Victor Spain et al., 2016 | X | X | X | ||||
| Papaspurou et al., 2015 | |||||||
| Patel et al., 2015 | |||||||
| Brod et al., 2014 | X | X | X | X | |||
| Simon et al., 2014 | X | ||||||
| Iyer et al., 2013 | X | X | X | X | |||
| Potkin et al., 2013 | |||||||
| Tan et al., 2011 | |||||||
| Jenkings et al., 2010 | |||||||
| Karter et al., 2010 | |||||||
| Peyrot et al., 2010 | |||||||
| Rubin et al., 2009 | |||||||
| Khan et al., 2008 | |||||||
| Larkin et al., 2008 | |||||||
| Hayes et al., 2006 | X | X | X | ||||
| Morris et al., 2005 | X | X | X | X | |||
| Mollema et al., 2001 |
| Article . | Health improvement . | Quick and long acting . | Convenient on management . | Taking control of their disease . | Less anxious, easier to take . | More effective . | Prevents complications . |
|---|---|---|---|---|---|---|---|
| Campbell et al., 2017 | |||||||
| Taylor et al., 2017 | X | X | X | ||||
| Taylor et al., 2016 | X | X | X | ||||
| Victor Spain et al., 2016 | X | X | X | ||||
| Papaspurou et al., 2015 | |||||||
| Patel et al., 2015 | |||||||
| Brod et al., 2014 | X | X | X | X | |||
| Simon et al., 2014 | X | ||||||
| Iyer et al., 2013 | X | X | X | X | |||
| Potkin et al., 2013 | |||||||
| Tan et al., 2011 | |||||||
| Jenkings et al., 2010 | |||||||
| Karter et al., 2010 | |||||||
| Peyrot et al., 2010 | |||||||
| Rubin et al., 2009 | |||||||
| Khan et al., 2008 | |||||||
| Larkin et al., 2008 | |||||||
| Hayes et al., 2006 | X | X | X | ||||
| Morris et al., 2005 | X | X | X | X | |||
| Mollema et al., 2001 |
Facilitators to initiation of injectables
Facilitators to the initiation of injectable therapy included health improvement, prevention of disease complications and taking control of their disease. Six out of eight studies highlighted the importance of treatment efficacy on physical and emotional aspects and the wellbeing of the patients using injectable therapies.14,33,37,38,40,43 Long-term disease complications and concerns about their disease worsening were also mentioned by the participants in two out of eight studies as an important facilitator to initiate injectable therapy.38,40 Finally, three studies stated that patients felt that they have much more control of their disease management through the use of injectable therapy.14,33,35
Facilitators to adherence and persistence of injectables
Facilitators to the adherence of injectable therapy included quick use, the effectiveness of the medication and convenience in management. Four of the studies stated that educated patients were more adherent to medication as they felt medication was convenient.29,33,35,43 Empowerment and confidence gained through self-management training by a diabetes health professional specialist appeared to be the most important facilitator to adherence. Moreover, in two out of eight studies patients already using injectable therapy highlighted that they felt less anxious and relieved after starting using injectables, mostly as they were able to see their effectiveness and improvement on disease control.35,43
Barriers to injectable therapy
All of the studies included in the review investigated the barriers to injectable therapy; both on initiation and ongoing adherence of eligible patients who were already prescribed or taking the injectables (Table 4).
| Article . | Injection phobia . | Complications/side effects . | Loss of independence . | Cost . | Social stigma . | Impact on skin (bruises, swellings) . | Impact on daily living . | Poor perception of benefits . | Inconvenience of management . | Depended on doctor . | Education problems . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Taylor et al., 2017 | X | X | X | X | X | ||||||
| Campbell et al., 2017 | X | ||||||||||
| Taylor et al., 2016 | X | X | X | X | X | ||||||
| Victor Spain et al., 2016 | X | X | X | ||||||||
| Papaspurou et al., 2015 | X | ||||||||||
| Patel et al., 2015 | X | X | |||||||||
| Brod et al., 2014 | X | X | X | X | X | ||||||
| Simon et al., 2014 | X | X | X | X | X | ||||||
| Iyer et al., 2013 | X | X | X | X | X | X | |||||
| Potkin et al., 2013 | X | X | X | X | |||||||
| Tan et al., 2011 | X | X | X | X | X | X | X | ||||
| Jenkings et al., 2010 | X | ||||||||||
| Karter et al., 2010 | X | X | X | X | X | X | |||||
| Peyrot et al., 2010 | X | X | X | ||||||||
| Rubin et al., 2009 | X | X | X | X | X | ||||||
| Khan et al., 2008 | X | X | X | X | X | X | |||||
| Larkin et al., 2008 | X | X | |||||||||
| Hayes et al., 2006 | X | X | X | X | X | ||||||
| Morris et al., 2005 | X | X | X | ||||||||
| Mollema et al., 2001 | X | X |
| Article . | Injection phobia . | Complications/side effects . | Loss of independence . | Cost . | Social stigma . | Impact on skin (bruises, swellings) . | Impact on daily living . | Poor perception of benefits . | Inconvenience of management . | Depended on doctor . | Education problems . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Taylor et al., 2017 | X | X | X | X | X | ||||||
| Campbell et al., 2017 | X | ||||||||||
| Taylor et al., 2016 | X | X | X | X | X | ||||||
| Victor Spain et al., 2016 | X | X | X | ||||||||
| Papaspurou et al., 2015 | X | ||||||||||
| Patel et al., 2015 | X | X | |||||||||
| Brod et al., 2014 | X | X | X | X | X | ||||||
| Simon et al., 2014 | X | X | X | X | X | ||||||
| Iyer et al., 2013 | X | X | X | X | X | X | |||||
| Potkin et al., 2013 | X | X | X | X | |||||||
| Tan et al., 2011 | X | X | X | X | X | X | X | ||||
| Jenkings et al., 2010 | X | ||||||||||
| Karter et al., 2010 | X | X | X | X | X | X | |||||
| Peyrot et al., 2010 | X | X | X | ||||||||
| Rubin et al., 2009 | X | X | X | X | X | ||||||
| Khan et al., 2008 | X | X | X | X | X | X | |||||
| Larkin et al., 2008 | X | X | |||||||||
| Hayes et al., 2006 | X | X | X | X | X | ||||||
| Morris et al., 2005 | X | X | X | ||||||||
| Mollema et al., 2001 | X | X |
| Article . | Injection phobia . | Complications/side effects . | Loss of independence . | Cost . | Social stigma . | Impact on skin (bruises, swellings) . | Impact on daily living . | Poor perception of benefits . | Inconvenience of management . | Depended on doctor . | Education problems . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Taylor et al., 2017 | X | X | X | X | X | ||||||
| Campbell et al., 2017 | X | ||||||||||
| Taylor et al., 2016 | X | X | X | X | X | ||||||
| Victor Spain et al., 2016 | X | X | X | ||||||||
| Papaspurou et al., 2015 | X | ||||||||||
| Patel et al., 2015 | X | X | |||||||||
| Brod et al., 2014 | X | X | X | X | X | ||||||
| Simon et al., 2014 | X | X | X | X | X | ||||||
| Iyer et al., 2013 | X | X | X | X | X | X | |||||
| Potkin et al., 2013 | X | X | X | X | |||||||
| Tan et al., 2011 | X | X | X | X | X | X | X | ||||
| Jenkings et al., 2010 | X | ||||||||||
| Karter et al., 2010 | X | X | X | X | X | X | |||||
| Peyrot et al., 2010 | X | X | X | ||||||||
| Rubin et al., 2009 | X | X | X | X | X | ||||||
| Khan et al., 2008 | X | X | X | X | X | X | |||||
| Larkin et al., 2008 | X | X | |||||||||
| Hayes et al., 2006 | X | X | X | X | X | ||||||
| Morris et al., 2005 | X | X | X | ||||||||
| Mollema et al., 2001 | X | X |
| Article . | Injection phobia . | Complications/side effects . | Loss of independence . | Cost . | Social stigma . | Impact on skin (bruises, swellings) . | Impact on daily living . | Poor perception of benefits . | Inconvenience of management . | Depended on doctor . | Education problems . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Taylor et al., 2017 | X | X | X | X | X | ||||||
| Campbell et al., 2017 | X | ||||||||||
| Taylor et al., 2016 | X | X | X | X | X | ||||||
| Victor Spain et al., 2016 | X | X | X | ||||||||
| Papaspurou et al., 2015 | X | ||||||||||
| Patel et al., 2015 | X | X | |||||||||
| Brod et al., 2014 | X | X | X | X | X | ||||||
| Simon et al., 2014 | X | X | X | X | X | ||||||
| Iyer et al., 2013 | X | X | X | X | X | X | |||||
| Potkin et al., 2013 | X | X | X | X | |||||||
| Tan et al., 2011 | X | X | X | X | X | X | X | ||||
| Jenkings et al., 2010 | X | ||||||||||
| Karter et al., 2010 | X | X | X | X | X | X | |||||
| Peyrot et al., 2010 | X | X | X | ||||||||
| Rubin et al., 2009 | X | X | X | X | X | ||||||
| Khan et al., 2008 | X | X | X | X | X | X | |||||
| Larkin et al., 2008 | X | X | |||||||||
| Hayes et al., 2006 | X | X | X | X | X | ||||||
| Morris et al., 2005 | X | X | X | ||||||||
| Mollema et al., 2001 | X | X |
Barriers to initiation of injectables
Almost all of the studies (17/20) found that fear of needles and apprehension about injecting were two of the most important barriers among the patients.11,12,14,16,29,,,–33,35,,–38,40,,–43 Although the two terms are overlapping barriers, it was decided to keep both because the term ‘apprehension’ tended to be more general and means more than the needle phobia. In addition, nine of the studies included in the review concluded that there was a commonly held perception that injectable insulin will cause harm, including blindness, renal failure, heart attack and early death.14,–16,32,33,38,40,41,43 Seven of the 20 studies identified that poor perception of the benefits of injectable therapies on their quality of life led patients to be more reluctant to start the use of injectables.12,14,16,32,33,35,41 This highlights the importance of education prior to the start of therapies.
Barriers to adherence and persistence of injectables
Barriers were also evident in those who had started therapies and threatened the ongoing adherence to medication. The most important factor, mentioned in nine out of 20 studies, was the inconvenience of self-management of the injectables.11,16,29,35,37,38,40,41,43 Self-management included self-injection, dose titration, knowledge and management of side effects. In addition, social stigma and impact on daily living were frequently mentioned as important barriers to adherence. In particular, in eight out of 20 studies patients talked about embarrassment and general difficulty administering their injectable in public,11,15,29,32,37,38,41,–43 while in seven of the studies included the ‘planning of their days around injections’ was one of the strongest statements from the participants.11,16,35,37,40,42,43 Financial barriers were mentioned in three of the studies.12,34,35 Participants stated that the cost of the medication and the supplies needed for self-monitoring had a direct impact on the control of the disease. Bodily injury associated with injections (bruising, destruction of body tissue) appeared to be another barrier to injectable adherence in four out of 20 studies.11,29,37,41 Finally, non-adherent patients confirmed a lack of education about the importance of injectable therapy, the attendant benefits and risks, the self-management requirements and the failure of health professionals to explain adequately all these at the time of diagnosis (six out of 20 studies).12,16,35,36,39,41
Perceptions for injectable therapies
Less than half of the included studies investigated patients’ perceptions about injectable therapies (eight/20) (Table 5).11,15,30,32,33,37,38,43
| Article . | Treatment of last resort (‘the end of the road’) . | Personal failure to self-manage . | Family and friends are more concerned . | Life becomes less flexible . | Punishment/ restriction . | Losing ‘normality’ . | Regaining health . |
|---|---|---|---|---|---|---|---|
| Campbell et al., 2017 | |||||||
| Taylor et al., 2017 | |||||||
| Taylor et al., 2016 | X | X | X | X | |||
| Victor Spain et al., 2016 | |||||||
| Papaspurou et al., 2015 | |||||||
| Patel et al., 2015 | X | ||||||
| Brod et al., 2014 | X | X | X | X | |||
| Simon et al., 2014 | X | ||||||
| Iyer et al., 2013 | |||||||
| Potkin et al., 2013 | |||||||
| Tan et al., 2011 | |||||||
| Jenkings et al., 2010 | |||||||
| Karter et al., 2010 | |||||||
| Peyrot et al., 2010 | |||||||
| Rubin et al., 2009 | X | X | |||||
| Khan et al., 2008 | X | ||||||
| Larkin et al., 2008 | X | X | X | X | |||
| Hayes et al., 2006 | |||||||
| Morris et al., 2005 | X | X | X | X | X | ||
| Mollema et al., 2001 |
| Article . | Treatment of last resort (‘the end of the road’) . | Personal failure to self-manage . | Family and friends are more concerned . | Life becomes less flexible . | Punishment/ restriction . | Losing ‘normality’ . | Regaining health . |
|---|---|---|---|---|---|---|---|
| Campbell et al., 2017 | |||||||
| Taylor et al., 2017 | |||||||
| Taylor et al., 2016 | X | X | X | X | |||
| Victor Spain et al., 2016 | |||||||
| Papaspurou et al., 2015 | |||||||
| Patel et al., 2015 | X | ||||||
| Brod et al., 2014 | X | X | X | X | |||
| Simon et al., 2014 | X | ||||||
| Iyer et al., 2013 | |||||||
| Potkin et al., 2013 | |||||||
| Tan et al., 2011 | |||||||
| Jenkings et al., 2010 | |||||||
| Karter et al., 2010 | |||||||
| Peyrot et al., 2010 | |||||||
| Rubin et al., 2009 | X | X | |||||
| Khan et al., 2008 | X | ||||||
| Larkin et al., 2008 | X | X | X | X | |||
| Hayes et al., 2006 | |||||||
| Morris et al., 2005 | X | X | X | X | X | ||
| Mollema et al., 2001 |
| Article . | Treatment of last resort (‘the end of the road’) . | Personal failure to self-manage . | Family and friends are more concerned . | Life becomes less flexible . | Punishment/ restriction . | Losing ‘normality’ . | Regaining health . |
|---|---|---|---|---|---|---|---|
| Campbell et al., 2017 | |||||||
| Taylor et al., 2017 | |||||||
| Taylor et al., 2016 | X | X | X | X | |||
| Victor Spain et al., 2016 | |||||||
| Papaspurou et al., 2015 | |||||||
| Patel et al., 2015 | X | ||||||
| Brod et al., 2014 | X | X | X | X | |||
| Simon et al., 2014 | X | ||||||
| Iyer et al., 2013 | |||||||
| Potkin et al., 2013 | |||||||
| Tan et al., 2011 | |||||||
| Jenkings et al., 2010 | |||||||
| Karter et al., 2010 | |||||||
| Peyrot et al., 2010 | |||||||
| Rubin et al., 2009 | X | X | |||||
| Khan et al., 2008 | X | ||||||
| Larkin et al., 2008 | X | X | X | X | |||
| Hayes et al., 2006 | |||||||
| Morris et al., 2005 | X | X | X | X | X | ||
| Mollema et al., 2001 |
| Article . | Treatment of last resort (‘the end of the road’) . | Personal failure to self-manage . | Family and friends are more concerned . | Life becomes less flexible . | Punishment/ restriction . | Losing ‘normality’ . | Regaining health . |
|---|---|---|---|---|---|---|---|
| Campbell et al., 2017 | |||||||
| Taylor et al., 2017 | |||||||
| Taylor et al., 2016 | X | X | X | X | |||
| Victor Spain et al., 2016 | |||||||
| Papaspurou et al., 2015 | |||||||
| Patel et al., 2015 | X | ||||||
| Brod et al., 2014 | X | X | X | X | |||
| Simon et al., 2014 | X | ||||||
| Iyer et al., 2013 | |||||||
| Potkin et al., 2013 | |||||||
| Tan et al., 2011 | |||||||
| Jenkings et al., 2010 | |||||||
| Karter et al., 2010 | |||||||
| Peyrot et al., 2010 | |||||||
| Rubin et al., 2009 | X | X | |||||
| Khan et al., 2008 | X | ||||||
| Larkin et al., 2008 | X | X | X | X | |||
| Hayes et al., 2006 | |||||||
| Morris et al., 2005 | X | X | X | X | X | ||
| Mollema et al., 2001 |
Perceptions on initiation of injectables
Almost all (six out of eight of the 20 studies) studies investigating perceptions referred to the perception of injectable therapies as a last resort (‘the end of the road’)15,30,32,37,38,43 and in five studies, the perception that life becomes less flexible.11,30,33,38,43 Other negative perceptions indicated were also ‘family and friends are more concerned’,30,38 injectable therapies were seen as ‘punishment/restriction’33 and ‘losing normality’.11,33 A positive perception for injectable therapies as a means of regaining health was indicated in only two studies.33,43
Perceptions to adherence and persistence of injectables
Only one perception related to adherence and persistence of injectables is referred to in the included studies; a personal failure of self-management and is reported in four of the studies.30,33,38,43
Discussion
Chronic diseases are a current and challenging issue in public health with tremendous personal and socioeconomic burden. Initiation of appropriate treatment, medication adherence and persistence are core components of chronic disease management to ensure optimal therapy, especially in CVD. It requires patients to be knowledgeable about the trajectory of their disease in order to be able to identify abnormal symptoms and intervene accordingly.44 Adequate disease management may preserve or better improve the quality of life of patients. A more detailed understanding of the patients’ condition will help health professionals to identify patients’ needs and disease complications before complex and acute events happen.45,–47
This integrative review identified 20 studies reporting facilitators and barriers for injectable therapies of persons with chronic diseases. More specifically, facilitators, barriers and perceptions of initiating and adhering to injectable therapies were found. In only two of the 20 studies were patients on LAI antipsychotics,12,35 while the participants of the rest of the studies were on insulin therapy.
The most common barriers found for the initiation of injectable therapies were the fear of needles, the perception that injectable insulin causes harm and the poor perception of the benefits of injectable therapies. A recent systematic review focusing on the barriers of insulin initiation also highlight needle phobia, and concern for side effects of insulin as the most common patient-related barriers.48 Parellada and Bioque (2015), in their review on LAI antipsychotics, also concluded that the main patient barriers to the initiation of injectable antipsychotics were the lack of adequate information on the benefits, the pragmatic difficulties in LAIs uptake and the negative perceptions on the medication.18 All these suggest that the barriers to the initiation of injectable therapies can be addressed by redoubling efforts on patients’ education18 and more effective communication between health professionals and patients.49 The articles included in this review referred to patients using either insulin or LAI antipsychotics. Reference to ‘harm’ and ‘poor benefits’ can be considered to mention those particular medications and not generally to injectable medicines that can be used in other conditions such as hypercholesterolemia and heart failure.
Patients’ attitudes towards injectable therapies are found to be influenced by their interactions with health professionals and the communication process between them.39,41,50 Communication is more than just the transfer of information or skills from one person to another; interpersonal aspects of communication in DM care, such as involvement in decision-making and goal setting, can impact on how the person with DM relates to and engages in their care.50 Injection phobia, fear of complications and side effects and poor perception of benefits, can easily be resolved through communication. It is stated that effective communication between health professionals and patients is very important for the patient’s treatment acceptance and adherence as well.49 Funnel et al. (2004) reported that diabetes nurse educators can help to decrease psychological insulin resistance and make a significant contribution to the education of patients with DM.51 Papaspurou et al. (2015) reported that most of the patients on injectable insulin expressed the need for communication, psychological support and self-management education from a diabetes nurse educator.39 Moreover, there is also growing evidence for CVD-specific injectable medicines. Kosmas et al. (2018) in their review showed overall better patient adherence to PCSK9 inhibitors in real-life settings. However, they suggested that in-depth patient education, close supervision and regular follow-up are important in order to optimise adherence and compliance with therapy.21
Inconvenience of management and education problems were also two of the most important barriers affecting the initiation and adherence to injectable therapies. Α recent review referred to a 4-hour educational module developed and tested to empower patients with type 2 diabetes being treated with injectable therapies for self-management. The module was found to allow health professionals to provide appropriate self-management education and support while increasing patients’ confidence and empowerment to self-manage.52 The results give health professionals evidence on what might work in enhancing effective communication and education for self-management as inconvenience of self-management, lack of education and the fear of body injury were found to be the most important barriers to non-adherence to injectable therapy.
Educational information may enhance communication between health professionals and patients and provide solutions to the barriers arising, thereby also encouraging continuity of care and adherence to injectable therapy. The possible development of an educational tool based on what is important to patients and health professionals in discussing the initiation of injectable therapy treatment, presented in plain terminology, using the language patients use and replying to most possible concerns, fears and misconceptions of patients might therefore have merit.43 Understanding of the factors influencing patients’ self-management decisions, and presentation of the beneficial effects of injectable therapy will help guide the development of appropriate and targeted educational information. Such a tool will help to educate patients who may need injectable therapy and will also support the patients in making the decision to initiate the therapy as early as possible to make it the most beneficial therapy for them, and at the same time to serve as a communication tool between health professionals and patients.
Other barriers found were the fear of social stigma, embarrassment and cost of medication. In diabetes social stigma is found to be positively and independently associated with negative insulin appraisals among adults with insulin-treated type 2 diabetes,53 and is the strongest contributor to diabetes-specific distress and self-efficacy.53,54 Myths and misconceptions about initiating insulin treatment are a challenge for health professionals and may make it difficult to change patient opinions. People with preconceived notions and fears about injectable therapy can be persistent in their decision to delay or not start treatment. These patients require special attention and further communication with health professionals, who need to recognise these barriers to treatment and proactively identify and address proper injectable initiation and optimisation to reduce future disease burden, instead of delaying initiation of the injectable therapy. It appears that for some patients, their internal fears and beliefs are stronger than their health professionals’ advice.43 Health professionals must be especially proactive in communicating and discussing the concerns raised by these patients, to overcome information gaps. They need to explain right from the beginning all possible therapies and their advantages, including injectable therapies, and help patients to understand that the use of different therapy does not mean ‘personal failure to self-manage’30,33,38,43 or worsening disease, but it may be the optimal therapy for them at a particular stage with better possible outcomes.
So, it is not surprising that the facilitators found to support adherence to injectable therapy include quick use, ease of use, effectiveness of the medication and self- management convenience.14,29,33,35,37,38,40,43 With adequate communication and education, information gaps and misconceptions may be overcome. Self-efficacy refers to the belief in one’s capability to predict and accomplish certain behaviours.55 Patients’ empowerment and increase of their self-efficacy can encourage mutual trust and open communication between patients and healthcare providers.50
Improved communication will further improve the therapeutic plan, and the development of a patient-centred relationship.56 Patients and health professionals may sometimes have divergent views in some areas; for example, glycaemic targets or consequences/complications of the disease, highlighting the need to agree blood glucose goals and therapy in a collaborative way.57,58 However, shared decision-making goes beyond maintaining active patient consent to decisions, it involves the shared shaping of disease management in order to advance the life and quality of life of the person.59 Future studies may bring to light ways and approaches of communication and information, enhancing a patient-centred relationship and decision-making. Possible focus groups and other qualitative analysis may provide more information on how to build such health professional–patient relationships promoting trust and at the same time confidence for self-management when injectable therapies are needed.
Strengths and limitations
The review’s strength is reflected by the systematic identification of papers using both broad and specific search strategies and multiple databases. The integrative approach allowed the inclusion of diverse methodologies and has the potential to play a great role in evidence-based practice for nursing. Its rigor is enhanced by the assessment of all papers added based on the critical appraisal by two members of the research team. A possible limitation of the study is the potential bias introduced by excluding non-English studies. Moreover, the data extracted from primary articles was from diverse methodologies generally with varied data. The complexity inherent in combining diverse methodologies could contribute to inaccuracy and bias. Also, the general reference in chronic diseases may create confusion to readers; nevertheless, health professionals realise the human perspectives might be in common among patient populations with chronic diseases. So, researchers aiming not to miss a possible facilitator, or barriers or perceptions that may occur when injectable therapies are needed, decided to include all relevant studies.
Conclusion
Injectable therapies are still creating dilemmas for patients as the change of the treatment is considered a failure of disease self-management or as a treatment of last resort no matter the benefits in preventing complications such as CVD. Fear of injections, inconvenience of management and educational problems were found to be the most important barriers to the use of injectable therapies. Thereby, it seems important for health professionals and researchers to find ways to improve communication with patients in order to overcome existing obstacles and barriers. There is currently a lot of evidence on how to create effective communication and shared decision-making relationships, with technology available to help health professionals to provide the best possible care to patients who need injectable therapy and support for self-management. The current review highlights that there were no studies focusing on barriers, facilitators or perceptions of patients using CVD-specific injectable therapies. Future research can focus on exploring all these in patients with CVD who are using injectable therapies. Moreover, this might help guide the response to fears of the patients and barriers to injectable therapies using patients’ language and by the development of a possible tool for making educational information easier.
The management of risk factors such as glucose and dyslipidaemia may lead to improved microand macro-vascular complications in individuals with Type 2 DM.
Yet, therapeutic inertia is common in the management of these risk factors in clinical practice, either due to patients’ refusal or HPs avoidance and delay, leading to increased incidence of CVD.
Increasing the knowledge of patients’ perceptions, facilitators, and barriers on the use of injectable therapies can guide healthcare providers and researchers to implement the appropriate interventions to support patients and their families in order to improve their health and quality of life.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This phase of the project is part of a larger funded study on injectable therapies in patients with cardiovascular disease.




Comments