-
Views
-
Cite
Cite
D Ciliberti, A Di Monaco, F Troisi, F Quadrini, L Sgarra, N Valenti, M Dadamo, F Fortunato, A Vitullo, M Milli, C Di Mario, M Grimaldi, ETHANOL ABLATION OF LEFT VENTRICULAR SUMMIT IN A PATIENT WITH REPAIRED CONGENITAL HEART DISEASE: WHEN THE GOING GETS THOUGH, European Heart Journal Supplements, Volume 27, Issue Supplement_5, May 2025, suaf076.017, https://doi.org/10.1093/eurheartjsupp/suaf076.017
Close - Share Icon Share
Abstract
A 22 years old young man with transposition of the great arteries, ventricular septal defect and pulmonary stenosis, repaired by previous Rastelli–type operation, showed up to our emergency department (ED) because of arrhythmic storm. Then, s–ICD had been implanted for secondary prevention, reaching clinical stability after two ablations and the addition of sotatol. In the ED, the patient was hemodynamically stable. Basal ECG was normal. Monomorphic VTs (289 ms CL, triggered by short couple extrasystole) had LBBB morphology, late transition, inferior axis, negative DI and QS morphology in the most negative lead aVL suggesting septal left ventricular summit, maybe between ventricular outflow tract (fig.1). A transthoracic echocardiogram showed normal bi–ventricular function and s–ICD interrogation appropriate interventions. Given the arrhythmogenesis, hydroquinidine was unsuccessfully added, so catheter ablation was pursued. Therefore, a CT heart scan was made and merged with electro–anatomical mapping (EAM). VT was induced localizing it near valved conduit in septal RVOT but only far field EGM were detected by a multi–spline catheter. Due to the intra–myocardial origin, we decided to perform coronary venous system (CVS) ethanol infusion. First of all the CVS angiography and EAM until the ostium of anterior inter ventricular vein (AIV) were carried out. Then, using a decapolar 4F micro–catheter we mapped septal branches of AIV identifying the best pace mapping and the earliest site of activation in the first branch (fig. 2), mirroring endocardial far field EGM. Angiography revealed collateral circulation between the first two branches. So an angioplasty balloon catheter was advanced over a wire in CS until the first branch; then, we moved forward a second balloon, distally over the ostium of second septal branch to avoid alcohol dissipation or infusion in non–targeting zones (fig. 3). At this point, after inflating baloons, ethanol infusion began with 1 ml every 40 seconds and overall 4 ml. Arrhythmia disappeared and no further VTs were inducible. During days after ablation, some non sustained VT were recorded so we continued sotalol therapy, referring the patient for stellectomy operation. Now he is asymptomatic and no further arrhythmias occurred. Left ventricular summit ablations are even more challenging in repaired congenital heart disease patients. Also in this case CVS ethanol infusion can be a feasible and effective approach.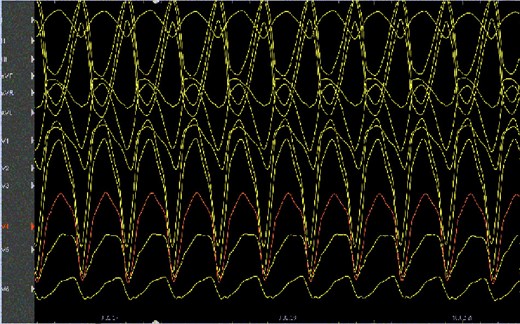
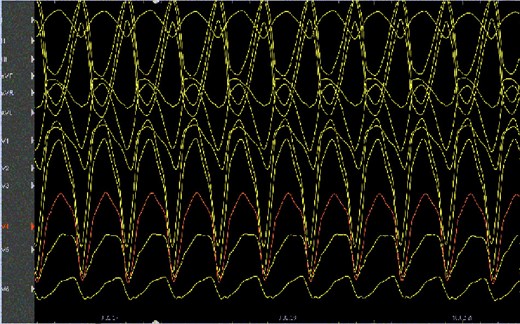
Figure 1
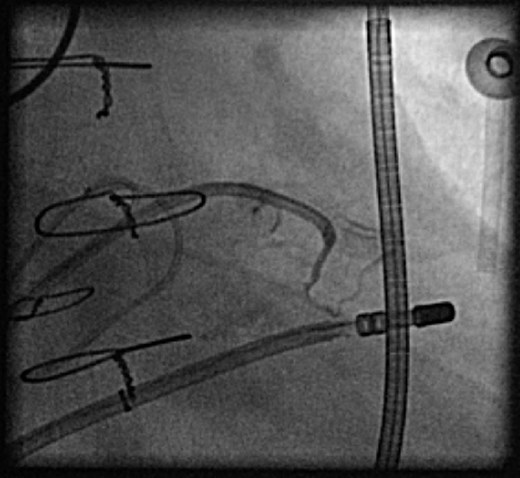
Figure 2
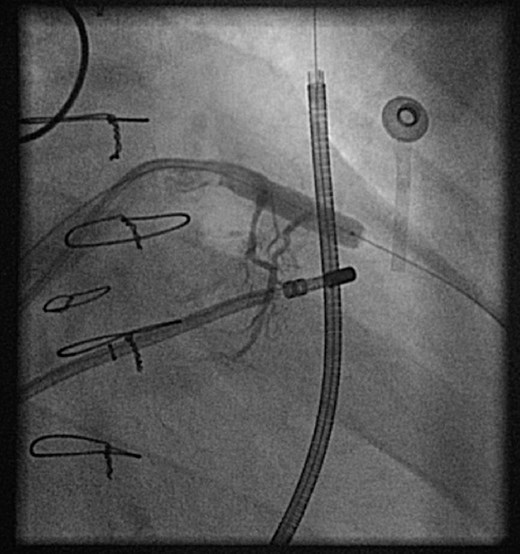
Figure 3
© The Author(s) 2025. Published by Oxford University Press on behalf of the European Society of Cardiology. All rights reserved. For commercial re-use, please contact [email protected] for reprints and translation rights for reprints. All other permissions can be obtained through our RightsLink service via the Permissions link on the article page on our site—for further information please contact [email protected].
This article is published and distributed under the terms of the Oxford University Press, Standard Journals Publication Model (https://dbpia.nl.go.kr/pages/standard-publication-reuse-rights)
You do not currently have access to this article.





