-
PDF
- Split View
-
Views
-
Cite
Cite
Harriette G C Van Spall, Roxana Mehran, James L Januzzi, Dear colleagues: enough with the men-only author panels, European Heart Journal Supplements, Volume 24, Issue Supplement_L, December 2022, Pages L53–L56, https://doi.org/10.1093/eurheartjsupp/suac118
Close - Share Icon Share
Introduction
Despite the gender balance among medical student graduates and those with advanced research degrees, women are under-represented as cardiovascular clinicians and research leaders relative to men. While the gender gap in cardiovascular research authorship appears to have narrowed in recent years, the dominance of men persists. In this viewpoint, we outline the benefits of diverse authorship, culprit factors in the gender imbalance among authors of cardiovascular research publications, and processes that leave women out of collaborations. We offer quick win and long-term recommendations for researchers, academic institutions, professional societies, sponsors, and journals to increase women in cardiovascular research collaborations and to harness the strengths that diverse teams bring to research.
Women are often excluded from research networks
Women represent a minority of authors in cardiovascular research publications, sometimes to the point of exclusion, due to pervasive gender inequities in the academia. The problem is only partly related to the under-representation of women as cardiovascular specialists; in fact, the pool of women cardiovascular researchers is much larger than cardiovascular specialists. For example, among National Institutes of Health (NIH)-funded R01 operating grant recipients for cardiovascular research in the USA, the largest pool were non-MD PhDs.1 Only 6.0% of R01 recipients for cardiovascular research were cardiologists and 0.8% were women cardiologists.2 There is gender parity among those who graduate with advanced research degrees, but men receive greater amounts of funding, get more citations, receive cardiovascular scientific awards more often, are invited to join research networks more frequently, and are given research leadership opportunities and journal senior editorial positions more commonly than women.1–18 Of a total of 1534 NIH grants award recipients, 20.0% were women; and among 406 co-recipients identified, 19.1% were women.1 Research submitted under a woman’s name is likely to receive a more critical review than the same research under a man’s name.9,16 Three quarters of industry payments are made to men, who get paid more for similar research activities as women.17 Thus, ‘gender-unequal’ processes hold women back as cardiovascular researchers.4 The informal institutional networks that invest in men via mentorship, research funding, salary support, and academic promotion also make them favourable candidates for collaborations; these grow citations and H-indices, and generate downstream research leadership positions. The process is self-fulfilling, creating an exclusive network, where individuals mentored into research leadership roles—typically men—are rewarded with incremental and exclusive opportunities for more leadership and collaborations.3
The notable attrition of women physicians at each stage of specialty training and at each academic rank is similar to that faced by non-physician researchers, and results from an interplay of factors that make academic medicine inhospitable to women. This attrition is evident at the institutional level, where biases, policies, and opportunities favour men over women, and destructive behaviours such as bullying, mobbing, and harassment more commonly target women than men.19 In environments that lack respect and equal opportunity, the skills, academic growth, and mentorship potential of women cardiovascular researchers are lost as women leave the academic environment, and achieving the goal of inclusion becomes all the more challenging.
The lower investment in women as research leaders, exclusion of women from research networks, and attrition of women from academia translate to a gender gap in research authorship. Data on men-only authorship panels are lacking. In an analysis of 414 heart failure (HF) trials published in high impact journals between 2000 and 2020, 19.6% of trial publications had exclusively men authors, and 25.9% had only one female author among a median (interquartile range) of 8 (5–12) authors per publication. In cardiovascular research, as a whole, women authors represent 35.3% of first and 22.9% of last authors, but these proportions are lower in high impact factor cardiovascular journals.5,10 The gender disparity in authorship varies with type of research articles, with a lower proportion of female first or last authors invited editorials and reviews than primary research articles.9 Within primary cardiovascular research, the gender disparities in authorship are greatest in clinical trials.8 The processes and policies that culminate in men-only research and authorship teams is reflected also in research steering committees; indeed, in a systematic review of HF randomized controlled trials published over the last 20 years, nearly half of all trial steering committees included no women.15
Importance of diverse research authorship panels
Research allyship, mentorship, and sponsorship occur along gender lines, and diverse research leaders build more diverse research teams. For example, cardiovascular publications with women senior authors have a greater proportion of women first and total authors, and trials led by women have a larger percentage of women steering committee members.3,5,14,15 Mentors guide individuals to develop skills in research and networking, while sponsors actively include individuals in their networks. Both are important to address the gender imbalance among authors in academic publishing. Diversity in research leadership and collaborations may encourage critical and disruptive thinking rather than ‘group think’; answer research questions relevant to diverse populations; and use culturally sensitive processes both within research teams and in interactions with patients.3,4,11,12 For example, in adjusted analyses, trials led by women investigators enrol a greater proportion of participants who are female, Black, Indigenous, and people of colour,11,12 generating more balanced subgroups for meaningful subgroup analysis. Since a majority of research continues to be led by men and include largely men collaborators, however, it is difficult to break the cycle of homogeneity among researchers without major change.3,5,8,9,11
Proposed solutions
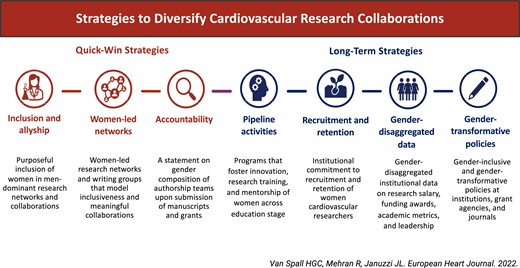
Strategies to address men-only research teams and to foster the growth of women as cardiovascular research leaders and collaborators could aim for quick wins and long-term success (Graphical Abstract). In the short term, there must be emphasis on purposeful, intentional, and meaningful inclusion of women researchers in research networks. This can only be achieved through active allyship of men colleagues and the immediate expansion of established research networks to foster diversity. Members of men-only research or authorship teams should raise inclusiveness as a priority and propose names of women who could provide meaningful input to the work. Women-led research networks and writing groups such as the Canadian Women’s Heart Health Alliance and those supported by the American College of Cardiology can also increase the academic output of women researchers, although, as gender disparities narrow, the goal should be for all networks to be diverse. Journals and grant agencies must reqest a diversity and inclusion statement from authors.
To address the underlying factors that culminate in men-only research and authorship teams, efforts should be made to recognize and mitigate unconscious or implicit bias; certificate programmes in Implicit Bias training should be offered to leaders and reviewers of awards, leadership funding opportunities in research institutes and granting agencies. Pipeline activities, research training programmes, research mentorship, and gender-equal research salary support could facilitate the career growth and retention of women cardiovascular researchers. There must be transparent reporting of gender-disaggregated metrics on recruitment, advancement, salary support, and retention at research institutes. Professional directories at the society, catalyst organization, or academic institution level could be used to identify qualified women researchers who wish to be included in research steering committees or collaborations. Lastly, analogous to the rules that exist in some regions to require women representatives on industry Board of Directors (with lack of parity subject to penalty), homogenous authorship teams should be identified and held accountable by academic journals and granting agencies: without such rigorous ‘carrot and stick’ policies, why would any change be made in the short term (Graphical Abstract)?
Conclusion
For far too long, the dominance of men has been normalized in academic medicine and cardiovascular research, with processes for recruitment, advancement, mentorship, and sponsorship favouring men. Men-only research teams, steering committees, and authorship groups persist, but there is a clear and pressing need to harness the potential of the current generation of motivated women academics. The cardiovascular research enterprise must be transformed to provide equal opportunity to women who have the skillset to lead and collaborate on research. Benefits from such evolution will include a broader range of ideas, voices, and interests, and propagation of research diversity not only among professionals but also among research participants. Active allyship from men, women-led research networks, and accountability from funding bodies and journals could narrow the gender gap in cardiovascular research authorship and end men-only authorship panels. Long-term gains will be made through the achievement of meaningful change in how academics are trained, evaluated, supported, and ultimately promoted. It is critical that such changes are made, and done so urgently.
Main messages
Women are under-represented as authors of cardiovascular research publications, in large part due to inequities within academic medicine and the research enterprise.
Diversity among researchers fuels further diversity, both among research authorship teams and research participants.
Deliberate action for quick wins and long-term gains must be taken by men and women investigators, academic institutions, professional societies, industry sponsors, funding agencies, and scientific journals to overcome gender inequalities in cardiovascular research.
Funding
This paper was published as part of a supplement sponsored by Novartis Pharma AG. The content was developed independent of the sponsor and the authors did not receive an honorarium.
Data availability
No new data were generated or analysed in support of this research.
References
Author notes
Men-only author papers (#Mapers) are still common in #CV science, widening the gender gap in academic advancement. We make a call for the purposeful inclusion of diverse authors and inclusive policies in cardiovascular research. @hvanspall @JJHeart_doc @Drroxmehran
Conflict of interest: J.L.J. is a Trustee of the American College of Cardiology, a Board member of Imbria Pharmaceuticals, has received grant support from Abbott Diagnostics, Applied Therapeutics, Innolife, Novartis Pharmaceuticals and Roche Diagnostics, consulting income from Abbott, Janssen, Novartis, Prevencio, and Roche Diagnostics, and participates in clinical endpoint committees/data safety monitoring boards for Abbott, AbbVie, Amgen, Bayer, CVRx, Janssen, MyoKardia, Takeda and Vifor. R.M. has received support from Abbott Laboratories, Abiomed, Applied Therapeutics, AstraZeneca, Bayer, Beth Israel Deaconess, Briston-Myers Squibb, CERC, Chiesi, Concept Medical, CSL Behring, DSI, and is co-founder of Women As One. H.G.C.V. receives research support from Canadian Institutes of Health Research and Heart and Stroke Foundation of Canada, and has initiated a Clinical Trials Diversity fellowship program to increase diversity among researchers.



