-
PDF
- Split View
-
Views
-
Cite
Cite
Daniele Guarino, Massimiliano Palazzini, Francesco Saia, Fabio Dardi, Nevio Taglieri, Alessandro De Lorenzis, Alberto Ballerini, Mariangela Rotunno, Ilenia Magnani, Federico Donato, Riccardo Bertozzi, Cinzia Marrozzini, Alessandra Manes, Nazzareno Galiè, 45 Experience of 5 years of balloon pulmonary angioplasty in a single centre: safety and short-term results, European Heart Journal Supplements, Volume 23, Issue Supplement_G, December 2021, suab133.010, https://doi.org/10.1093/eurheartj/suab133.010
Close - Share Icon Share
Abstract
Balloon pulmonary angioplasty (BPA) has recently been developed as a treatment strategy for chronic thromboembolic pulmonary hypertension (CTEPH) but efficacy and technical safety have to be established. We examine the effects of BPA on patients with inoperable disease or residual pulmonary hypertension (PH) after pulmonary endarterectomy (PEA).
From 2015 to 2020 we enrolled symptomatic inoperable CTEPH patients and patients with residual PH after PEA. At baseline and 3 months after last BPA session patients underwent clinical evaluation, 6-min walking distance (6MWD), and right heart catheterization. Friedman test with Bonferroni post-hoc pairwise analysis was used. Fifty patients [male 42%, median age 68 (51–74) years, 42 inoperable, and 8 with residual PH after PEA] were treated for a total of 156 sessions (median 2 sessions/patient); during each session we treated 2.3 (2.2–2.7) vessels. Results are shown in the Table. Forty-nine patients were treated with medical therapy before BPA (19 with combination therapy). Five pulmonary artery dissection and two haemoptysis with clinical impairment were documented during the procedures; 37 patients had lung injury (radiographic opacity with/without haemoptysis and/or hypoxaemia), none had renal dysfunction, 7 patients had access site complications. Seven patients died during follow-up (none within 30 days from the procedure) because of sepsis (1), heart failure (1), cancer (2), arrhythmic storm (2), and sudden death in patients with severe coronary atherosclerosis (1).
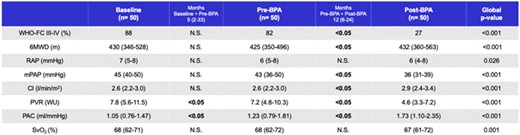
6MWD, six minute walking distance
CI, cardiac index; mPAP, mean pulmonary arterial pressure; PAC, pulmonary arterial compliance; PVR, pulmonary vascular resistance; RAP, right atrial pressure; SvO2, mixed venous oxygen saturation; WHO-FC, World Health Organization functional class.
- atherosclerosis
- catheterization of right heart
- coronary arteriosclerosis
- sepsis
- sudden death
- hemodynamics
- thromboembolic pulmonary hypertension
- pulmonary artery
- hypoxemia
- balloon dilatation
- lung
- heart failure
- pulmonary hypertension
- cancer
- right atrial pressure
- kidney failure
- hemoptysis
- angioplasty
- combined modality therapy
- tissue dissection
- follow-up
- safety
- world health organization
- pulmonary artery line
- mixed venous oxygen saturation measurement
- cardiac index
- pulmonary artery pressure
- lung injuries
- pulmonary vascular resistance
- walking distance
- pulmonary artery endarterectomy
- 6-minute walk test
- medical management
- treatment effectiveness
- site of access
- friedman test
- cardiac electrical storm



