-
PDF
- Split View
-
Views
-
Cite
Cite
Francesco Versaci, Sebastiano Sciarretta, Massimiliano Scappaticci, Riccardo Di Pietro, Simone Calcagno, Armando Del Prete, Carlo Gaspardone, Giuseppe Biondi Zoccai, Renal arteries denervation: from the treatment of resistant hypertension to the treatment of atrial fibrillation, European Heart Journal Supplements, Volume 23, Issue Supplement_E, October 2021, Pages E177–E183, https://doi.org/10.1093/eurheartj/suab117
Close - Share Icon Share
Abstract
Renal denervation (RDN) is a therapeutic strategy for patients with uncontrolled arterial hypertension characterized by considerable fluctuations during its progression. After initial strong enthusiasm, the procedure came to an abrupt halt following the publication of the Symplicity HTN-3 study results. The results of recently published studies highlight the reduction in blood pressure values after RDN and justify the inclusion in the Guidelines of new recommendations for the use of RDN in clinical practice, in selected patients. Additionally, RDN findings are summarized in view of other potential indications such as atrial fibrillation. Six prospective, randomized studies are presented that evaluated RDN as an adjunct therapy to pulmonary vein isolation for the treatment of atrial fibrillation. In five studies, patients had uncontrolled hypertension despite therapy with three antihypertensive drugs. The analysis of these studies showed that RDN reduced the recurrence of atrial fibrillation (AF) by 57% compared to patients with pulmonary vein isolation (PVI) only. Modulation of the autonomic nervous system by RDN has been shown not only to reduce blood pressure but also to have an antiarrhythmic effect in symptomatic AF patients when the strategy is combined with PVI, thus opening up new therapeutic scenarios.
Introduction
RDN is a therapeutic option for the treatment of resistant arterial hypertension and for uncontrolled hypertension. 1 Initial randomized studies such as Symplicity HTN-1 and the Symplicity HTN-2 had shown promising results of renal denervation in reducing blood pressure levels; 2,3 however, in 2014 the Symplicity HTN-3 study, a randomized study comparing RDNs to the placebo group, had shown insignificant differences between the groups of patients studied. 4,5 The reasons for these results were many, among them the sample of patients numerically insufficient from a statistical point of view, the inadequate selection of patients, the inexperience of the operators, and the use of first-generation devices. More recent randomized trials were carried out with second-generation devices: the DENERHTN trial, the Spyral HTN-OFF MED trial, the Spyral HTN-ON MED trial and the RARDIANCE-HTN SOLO trial showing how renal denervation resulted in a significant reduction in arterial blood pressure in the outpatient setting. 6–13
This review will highlight the results of the latest RDN studies for the treatment of arterial hypertension. The effects of RDN on other potential applications such as in the treatment of atrial fibrillation will also be summarized.
Kidney denervation in the treatment of arterial hypertension
Randomized studies vs. placebo
In the SPYRAL HTN-OFF MED trial, 7 recently published in the Lancet, 331 patients with uncontrolled arterial hypertension (Table 1), not on drug treatment, were randomized 1:1 to RDN or placebo treatment. The RDN procedure was performed using second-generation devices: Spyral™ catheter with four electrodes. In order to reduce procedural variability, in each centre, the intervention was carried out by the same operator. The energy required for denervation was released by placing the electrodes in the main artery or in the branches with a diameter greater than 3 mm. In the RDN group, the average number of ablation points was 46.9 (18.3 in the main artery and 28.6 in the secondary branches). In randomized patients, blood and urine samples were taken at baseline and after three months, to assess the absence of metabolites of antihypertensive drugs. At baseline, no antihypertensive drug was found in 91% of patients in the RDN group and in 87% of the placebo group. At three months, excluding patients who had to resort to drug treatment due to increased blood pressure, 91 and 95% of patients, respectively, had no drug treatment. After three months, there was a reduction in 24-h systolic blood pressure of 4.7 mmHg in the RDN group and of 0.6 mmHg in the placebo group (P < 0.0005), while ambulatory blood pressure values obtained in the two groups were 9.2 vs. 2.5 mmHg, respectively (P < 0.0001). Interestingly, the reduction in systolic and diastolic pressure was persistent throughout the day. Furthermore, no major events related to the RDN were recorded, confirming the safety of the procedure carried out with the second-generation devices.
The results of the main studies that evaluated the effects of renal denervation (RDN) for the treatment of systemic arterial hypertension
| Study . | Type of study . | Year . | Type of device . | Baseline blood pressure for inclusion . | Antihypertensive therapy . | No. of patients/controls . | Traeatment sham/therapy . | Follow-up . | Reduction of BP in the group RDN/sham PAS/PAD (mmHg) Ambulatory ABPM RDN Sham/RDN Sham . | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SPYRAL-HTN OFF MED | RCT | 2020 | Multiple unipolar electrode radiofrequency energy | Ambulatory BP 150–179 mmHg e PAD ≥ 90mmHg e 24-h PAD 140–169 mmHg | Off | 166/165 | Yes/yes | 3 months | −9.2/−5.1 | −2.5/−1.0 | −4.7/−3.7 | −0.6/−0.8 |
| RADIANCE-HTN SOLO | RCT | 2019 | Ultrasuond catheter | 24-h PAD 135–169 mmHg e 24-h PAD 85–104 mmHg | On | 74/72 | Yes/no | 6 months | −18.2/−10.1 | −15.9/−9.5 | −16.5/−9.7 | −14.9/−9.4 |
| REDUCE HTN: REINFORCE | RCT | 2020 | bipolar catheter radiofrequency energy | Ambulatory BP 150–180 mmHg e 24-h PAS 140–170 mmHg | Off | 34/17 | Yes/yes | 2 months | −5.2/−2.5 | −5.2/−2.5 | −5.3/−2.6 | −8.5/−4.6 |
| Mahfoud et al. | Non-randomized, open-label | 2020 | RDN Alcohol infusion | Ambulatory BP ≥ 150, PAD ≥ 85 mmHg e 24-h PAS ≥ 135 mm Hg | On | 45/– | No/no | 6 months | −18/−10 | ND | −11/−7 | ND |
| Global Symplicity Registry | Register | 2019 | Catheter with single unipolar electrode radiofrequency energy | Ambulatory BP ≥ 150 mm Hg e 24 h PAS ≥ 135 mm Hg | On | 1742/– | No/no | 3 months | −16.5/NA | ND | −8.0/NA | ND |
| Study . | Type of study . | Year . | Type of device . | Baseline blood pressure for inclusion . | Antihypertensive therapy . | No. of patients/controls . | Traeatment sham/therapy . | Follow-up . | Reduction of BP in the group RDN/sham PAS/PAD (mmHg) Ambulatory ABPM RDN Sham/RDN Sham . | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SPYRAL-HTN OFF MED | RCT | 2020 | Multiple unipolar electrode radiofrequency energy | Ambulatory BP 150–179 mmHg e PAD ≥ 90mmHg e 24-h PAD 140–169 mmHg | Off | 166/165 | Yes/yes | 3 months | −9.2/−5.1 | −2.5/−1.0 | −4.7/−3.7 | −0.6/−0.8 |
| RADIANCE-HTN SOLO | RCT | 2019 | Ultrasuond catheter | 24-h PAD 135–169 mmHg e 24-h PAD 85–104 mmHg | On | 74/72 | Yes/no | 6 months | −18.2/−10.1 | −15.9/−9.5 | −16.5/−9.7 | −14.9/−9.4 |
| REDUCE HTN: REINFORCE | RCT | 2020 | bipolar catheter radiofrequency energy | Ambulatory BP 150–180 mmHg e 24-h PAS 140–170 mmHg | Off | 34/17 | Yes/yes | 2 months | −5.2/−2.5 | −5.2/−2.5 | −5.3/−2.6 | −8.5/−4.6 |
| Mahfoud et al. | Non-randomized, open-label | 2020 | RDN Alcohol infusion | Ambulatory BP ≥ 150, PAD ≥ 85 mmHg e 24-h PAS ≥ 135 mm Hg | On | 45/– | No/no | 6 months | −18/−10 | ND | −11/−7 | ND |
| Global Symplicity Registry | Register | 2019 | Catheter with single unipolar electrode radiofrequency energy | Ambulatory BP ≥ 150 mm Hg e 24 h PAS ≥ 135 mm Hg | On | 1742/– | No/no | 3 months | −16.5/NA | ND | −8.0/NA | ND |
BP: blood pressure; SBP: systolic blood pressure; DBP: diastolic blood pressure; NA: not applicable; NP: not performed; RCT: Randomized controlled trial; ABPM: blood pressure monitoring for 24 h.
The results of the main studies that evaluated the effects of renal denervation (RDN) for the treatment of systemic arterial hypertension
| Study . | Type of study . | Year . | Type of device . | Baseline blood pressure for inclusion . | Antihypertensive therapy . | No. of patients/controls . | Traeatment sham/therapy . | Follow-up . | Reduction of BP in the group RDN/sham PAS/PAD (mmHg) Ambulatory ABPM RDN Sham/RDN Sham . | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SPYRAL-HTN OFF MED | RCT | 2020 | Multiple unipolar electrode radiofrequency energy | Ambulatory BP 150–179 mmHg e PAD ≥ 90mmHg e 24-h PAD 140–169 mmHg | Off | 166/165 | Yes/yes | 3 months | −9.2/−5.1 | −2.5/−1.0 | −4.7/−3.7 | −0.6/−0.8 |
| RADIANCE-HTN SOLO | RCT | 2019 | Ultrasuond catheter | 24-h PAD 135–169 mmHg e 24-h PAD 85–104 mmHg | On | 74/72 | Yes/no | 6 months | −18.2/−10.1 | −15.9/−9.5 | −16.5/−9.7 | −14.9/−9.4 |
| REDUCE HTN: REINFORCE | RCT | 2020 | bipolar catheter radiofrequency energy | Ambulatory BP 150–180 mmHg e 24-h PAS 140–170 mmHg | Off | 34/17 | Yes/yes | 2 months | −5.2/−2.5 | −5.2/−2.5 | −5.3/−2.6 | −8.5/−4.6 |
| Mahfoud et al. | Non-randomized, open-label | 2020 | RDN Alcohol infusion | Ambulatory BP ≥ 150, PAD ≥ 85 mmHg e 24-h PAS ≥ 135 mm Hg | On | 45/– | No/no | 6 months | −18/−10 | ND | −11/−7 | ND |
| Global Symplicity Registry | Register | 2019 | Catheter with single unipolar electrode radiofrequency energy | Ambulatory BP ≥ 150 mm Hg e 24 h PAS ≥ 135 mm Hg | On | 1742/– | No/no | 3 months | −16.5/NA | ND | −8.0/NA | ND |
| Study . | Type of study . | Year . | Type of device . | Baseline blood pressure for inclusion . | Antihypertensive therapy . | No. of patients/controls . | Traeatment sham/therapy . | Follow-up . | Reduction of BP in the group RDN/sham PAS/PAD (mmHg) Ambulatory ABPM RDN Sham/RDN Sham . | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SPYRAL-HTN OFF MED | RCT | 2020 | Multiple unipolar electrode radiofrequency energy | Ambulatory BP 150–179 mmHg e PAD ≥ 90mmHg e 24-h PAD 140–169 mmHg | Off | 166/165 | Yes/yes | 3 months | −9.2/−5.1 | −2.5/−1.0 | −4.7/−3.7 | −0.6/−0.8 |
| RADIANCE-HTN SOLO | RCT | 2019 | Ultrasuond catheter | 24-h PAD 135–169 mmHg e 24-h PAD 85–104 mmHg | On | 74/72 | Yes/no | 6 months | −18.2/−10.1 | −15.9/−9.5 | −16.5/−9.7 | −14.9/−9.4 |
| REDUCE HTN: REINFORCE | RCT | 2020 | bipolar catheter radiofrequency energy | Ambulatory BP 150–180 mmHg e 24-h PAS 140–170 mmHg | Off | 34/17 | Yes/yes | 2 months | −5.2/−2.5 | −5.2/−2.5 | −5.3/−2.6 | −8.5/−4.6 |
| Mahfoud et al. | Non-randomized, open-label | 2020 | RDN Alcohol infusion | Ambulatory BP ≥ 150, PAD ≥ 85 mmHg e 24-h PAS ≥ 135 mm Hg | On | 45/– | No/no | 6 months | −18/−10 | ND | −11/−7 | ND |
| Global Symplicity Registry | Register | 2019 | Catheter with single unipolar electrode radiofrequency energy | Ambulatory BP ≥ 150 mm Hg e 24 h PAS ≥ 135 mm Hg | On | 1742/– | No/no | 3 months | −16.5/NA | ND | −8.0/NA | ND |
BP: blood pressure; SBP: systolic blood pressure; DBP: diastolic blood pressure; NA: not applicable; NP: not performed; RCT: Randomized controlled trial; ABPM: blood pressure monitoring for 24 h.
The RADIANCE-SOLO9 trial was a multi-centre randomized placebo-controlled trial, in which patients with systolic-diastolic hypertension were recruited after 4 weeks of stopping at least two antihypertensive drugs. Patients were randomized to RDN by ultrasound device or placebo. After 2 months, a significantly greater reduction in ambulatory systolic blood pressure values was recorded in the RDN group compared to the placebo group (−8.5 vs. −2.2 mmHg). Between the 2nd and 5th months of treatment (RDN vs. placebo), based on blood pressure (BP) values (if greater than 135/85 mmHg), a standardized antihypertensive treatment was started, consisting of the addition of amlodipine (5 mg/day), a standard dose of angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker and hydrochlorothiazide (12.5 mg/dL). This regimen could be adapted, when necessary, by increasing hydrochlorothiazide to 25 mg/day and amlodipine to 10 mg per day. At 6 months, 65.2% of patients in the RDN group were treated with hypertensive drugs vs. 84.5% in the placebo group (P = 0.008). The mean number of antihypertensive drugs was significantly lower in the RDN group than in the placebo group (0.9 vs. 1.3; P = 0.01). Despite the lower use of drugs, the RDN group was characterized by a greater reduction in BP compared to the placebo group (−18.1 vs. −15.6 mmHg); the difference in BP adjusted for the number of drugs was −4.3 mmHg, (P = 0.024). No adverse events were reported in the Follow-up of the two treated groups. Another very interesting study is the REDUCE HTN: REIFORCE (Renal Denervation Using the Vessix Renal Denervation System for the Treatment of Hypertension): 10 a randomized, placebo-controlled multicenter trial performed using the Vessix™ radiofrequency bipolar, multi-electrode device. Patients with systolic BP between 180 and 150 mmHg and mean BP at Holter recording of 135–170 mmHg after drug withdrawal were randomized. The goal of the study was the reduction of systolic BP values during the 24 h up to 8 weeks. At 8 weeks, the mean reduction in systolic BP was −5.3 mmHg for the RDN group and −8.5 mmHg for the placebo group (P = ns). Enrollment was interrupted before reaching the predetermined sample number, but the observation continued and antihypertensive drug therapy was added as planned in the study. Particularly surprising were the results at 6 months which showed a greater reduction in BP values in the RDN group: the differences between the two groups were −7.2 mmHg for the 24-h systolic BP and −11.4 mmHg for the BP measured in the clinic. More patients in the RDN group achieved values below 140 mmHg (52 vs. 12% in the placebo group with P = 0.0061), despite the same number of patients (∼50%) in each group taking antihypertensive medical therapy. In addition, the antihypertensive effect of RDN was maintained between the 6th and 12th months, underlining the persistence of the effectiveness of RDN over time. The authors identified two potential reasons for the delayed response of RDN. The first is that the RDN does not immediately interrupt the efferent sympathetic activity but determines an ablation of the signals of the efferent sympathetic fibres towards the kidney. Consequently, the impact of the kidneys on sympathetic afferent fibres to modify central regulation is delayed. The second is that antihypertensive drugs are more effective in reducing BP in patients treated with RDN. In fact, the efficacy of drugs such as vasodilators and diuretics can be limited by an increase in sympathetic activity, therefore the sympathetic-inhibitory effects produced by RDN can increase the BP-lowering effects of drug therapy.
Non-randomized studies and registers
In recent months, the results of studies have been published that have evaluated the efficacy and safety of new devices for RDN. In particular, the Peregrine device was used which allows the infusion of a neuro-lytic agent such as alcohol into the peri-arterial space. 14 Forty-five patients with hypertension not controlled by at least three drugs were treated. In the 6-month follow-up, a reduction in systolic BP of 11 mmHg and diastolic BP of 7 mmHg was achieved (P < 0.001). Ambulatory systolic BP was reduced by 18 mmHg and diastolic by 10 mmHg (P < 0.001). Two pseudo-aneurysms were recorded at the femoral access site but no major adverse events. The results of the ongoing TARGET BP OFF MED and TARGET BP randomized controlled trials will offer further data regarding the safety and efficacy of these devices.
Global SYMPLICITY Register
The Global SYMPLICITY Registry is a study conducted in 196 countries around the world in hypertensive patients treated with RDN. 15 2237 patients were enrolled and treated with Symplicity Flex™ catheter. The results showed a persistent reduction in BP in the three-year follow-up, represented by a reduction in ambulatory pressure after RDN (−16.5 ± 28.6 mmHg, P < 0.001) and in 24/h systolic BP values (−8 ± 20 mmHg; P < 0.001). The data show greater efficacy of RDN in patients with higher BP values (systolic BP ≥160 and mean BP ≥135 mmHg despite at least three antihypertensive drugs). In this group of patients, the reduction in ambulatory systolic BP was 26.7 mmHg and the mean daily reduction was 12.4 mmHg. The multivariate analysis shows that higher BP levels are associated with a greater reduction in pressure values at 12, 24, and 36 months after RDN.
Meta-analyses of placebo-controlled studies confirmed a significant reduction in 24-h BP and ambulatory systolic BP compared to the placebo group (−3.6 mmHg, P < 0.001 and −5.5 mmHg, P < 0.001, respectively). 16 Further analysis showed that second-generation RDN devices are more effective than first-generation ones in reducing BP values. 17–19 Furthermore, a recent network meta-analysis showed that treatment with extended RDN, in the main branch, as well as in its branches, is more effective in reducing systolic and diastolic BP values in the 24 h. 20
Renal denervation in patients with atrial fibrillation
Hypertension is an important risk factor for atrial fibrillation (AF): facilitating its onset, relapses and persistence. 21 The incidence of AF increases with the presence of ventricular hypertrophy and heart failure, often consequences of non-controlled hypertension (Figure 1). From a pathophysiological point of view, the imbalance of the sympathetic and vagal nervous systems play a key role in both arterial hypertension and atrial fibrillation. It is known that the increase in BP levels, both acute and chronic, cause stretching and dilation of the atrial walls with deleterious effects on electrical activity. Adrenergic activation also represents a trigger on a vulnerable atrial substrate inducing arrhythmias, including AF.
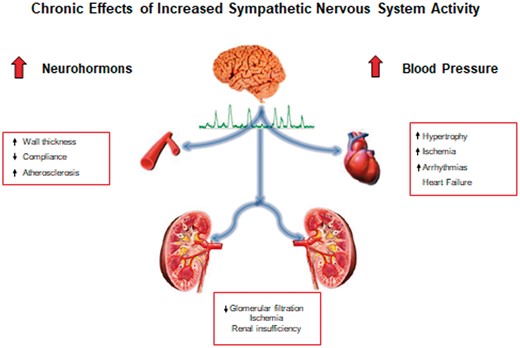
The chronic effects of increased sympathetic activity cause organ damage, dictated by the increase in the vascular wall thickness which in turn leads to an increase in resistance and an acceleration of atherosclerosis. This cascade of events involves parietal hypertrophy with reduced ventricular compliance leading to heart failure and arrhythmias such as atrial fibrillation. All these changes also lead to a reduction in renal function.
The antiarrhythmic effect of RDN is based on the reduction in the activity of the sympathetic nervous system highlighted through the reduction of the norepinephrine spillover.
Pulmonary vein isolation (PVI) is a therapeutic option used for the treatment of symptomatic atrial fibrillation in both paroxysmal and persistent forms. However, in patients with altered atrial substrate further interventions may be necessary to optimize the antiarrhythmic response. BP control is one of the therapeutic strategies that can have a favourable impact in reducing triggers that arise from the pulmonary veins. Experimental and subsequent clinical studies have shown that RDN can reduce relapses of atrial fibrillation after isolation of the pulmonary veins. Ablation of the afferent pathways of the sympathetic nervous system can attenuate the triggers of the autonomic nervous system on atrial fibrillation as well as improving pressure control.
Preclinical studies have shown numerous antiarrhythmic effects of RDN. In experimental studies, RDN was associated with a reduction in the inducibility and complexity of atrial fibrillation, and in treated patients, greater control of the ventricular rate, a reduced shortening of the atrial refractory period, reduced neurohormonal activation and reduced atrial fibrosis were observed. 22
Based on these observations, a small randomized pilot study was conducted on 27 patients with paroxysmal or persistent AF and resistant hypertension. Patients undergoing RDN had a lower incidence of AF episodes and 69% of treated patients had no AF episodes at 1 year. This important prospective pilot study demonstrated that RDN has a positive role in reducing recurrent AF episodes in patients with hypertension and AF undergoing pulmonary vein isolation procedures. In patients treated with RDN, there was an improvement in systolic and diastolic BP values at 1 year of follow-up. 23
Based on these encouraging first experimental data, prospective randomized trials have recently been conducted with the aim of evaluating the effects of pulmonary vein isolation and RDN in patients with atrial fibrillation and uncontrolled hypertension. 24–26
Table 2 shows the six most important prospective randomized studies that evaluated the effectiveness of RDN as an adjunct therapy to the isolation of the pulmonary veins in patients with AF. Ukena et al. conducted a meta-analysis including 689 patients with hypertension and AF. 27 This meta-analysis included five studies in patients with uncontrolled arterial hypertension despite treatment with three antihypertensive drugs. Pulmonary vein isolation was performed with the radiofrequency catheter in 387 patients and with cryoablation in 302 patients. Results at 12 months showed a significant reduction in BP in patients treated with RDN, while in patients treated with pulmonary vein isolation without RND, no significant reduction in BP was observed. The recurrence of atrial fibrillation in patients treated with PVI and RDN was significantly lower than in patients with PVI but without RDN (mean odds ratio 0.43—95% confidence interval). No major complications were reported in patients treated with RDN. Further prospective studies to evaluate the efficacy of RDN in patients with AF treated with PVI are currently underway and the results will be particularly useful to underline the importance of this therapeutic strategy in this particular patient setting.
 |
 |
The most important prospective randomized studies that have demonstrated the efficacy of renal denervation (RDN) as an adjunct therapy to pulmonary vein isolation (IVP) in patients with resistant arterial hypertension and atrial fibrillation. Follow-up showed, in patients treated with pulmonary vein isolation, a significant reduction in systemic blood pressure compared to patients not treated with renal denervation. In addition, a significant reduction in atrial fibrillation recurrence (mean odds ratio 0.43—95% confidence interval) was observed in these patients compared to those treated with pulmonary vein isolation alone.
 |
 |
The most important prospective randomized studies that have demonstrated the efficacy of renal denervation (RDN) as an adjunct therapy to pulmonary vein isolation (IVP) in patients with resistant arterial hypertension and atrial fibrillation. Follow-up showed, in patients treated with pulmonary vein isolation, a significant reduction in systemic blood pressure compared to patients not treated with renal denervation. In addition, a significant reduction in atrial fibrillation recurrence (mean odds ratio 0.43—95% confidence interval) was observed in these patients compared to those treated with pulmonary vein isolation alone.
Conclusions
Recent studies carried out with the second generation devices for RDN have demonstrated the effectiveness of RDN in reducing BP values in a significant and clinically relevant way. The intensity of the response on BP values if translated to similar effects on BP values obtained from pharmacological studies determines a significant reduction in the risk of cardiovascular events.
These results justify the drafting of new recommendations in the hypertension guidelines for the use of RDN in clinical practice in selected patients.
Furthermore, the modulation achieved with RDN on the sympathetic system has shown to be able not only to reduce the BP values but also to have favourable antiarrhythmic effects in symptomatic patients with AF undergoing PVI, thus representing a further therapeutic strategy.
References
Symplicity HTN-1 Investigators.



