-
PDF
- Split View
-
Views
-
Cite
Cite
Ana Molinero, Luis M Ruilope, Salvador Tous, José A Fornos, Inés Mera, Nicanor F Andrés, Montserrat Iracheta, Xin Xia, Thomas Beaney, Neil R Poulter, Enrique Rodilla, Fernando Martínez, Teresa Gijón-Conde, May Measurement Month 2017: an analysis of blood pressure screening in Spain—Europe, European Heart Journal Supplements, Volume 21, Issue Supplement_D, April 2019, Pages D107–D110, https://doi.org/10.1093/eurheartj/suz070
Close - Share Icon Share
Abstract
May Measurement Month 2017 is a global initiative aimed at raising awareness of high blood pressure (BP) and to act as a temporary solution to the lack of screening programs worldwide, in which Spain participated actively. The primary objective was to raise awareness and increase control of BP in Spain. An opportunistic cross-sectional survey of volunteers aged ≥18 was set up in May 2017. Following the design of the International Society of Hypertension, data were collected from the 17 autonomous communities in which Spain is divided, mainly in community pharmacies, primary care centres and some hypertension (HT) units, and cardiovascular departments in hospitals. No additional training of volunteers was necessary. A total of 3849 individuals were screened. After multiple imputation, our data showed that 1923 (50.0%) had HT. In those not receiving antihypertensive medication, 17.5% were hypertensives, in individuals receiving antihypertensive medication, 33.9% had uncontrolled BP. May Measurement Month 2017 was the largest BP screening campaign undertaken in Spain. In total, 17.5% of people with HT did not receive medication. One-third of hypertensive participants receiving treatment did not have their BP controlled. These results confirm that an opportunistic screening can identify a significant number of subjects with and untreated and inadequately treated BP.
Background
Raised blood pressure (BP) is a growing burden worldwide.1,2 Hypertension (HT) is the most prevalent chronic disease in Spain. According to the latest national study on Nutrition and Cardiovascular Risk in Spain, performed on a representative sample of the non-institutionalized population of Spain aged ≥18 years, 33.3% were hypertensive, 59.4% were aware of their condition, 78.8% were treated among those who were aware, and 48.5% were controlled among those aware and treated (22.7% of all hypertensives).3 Recent data of The National Statistical Institute report that (HT-related) cardiovascular disease is still the main cause of death in Spain,4 representing 29.2% of all deaths (32.8% in women and 25.6% in men). Of all deaths in Spain, 7.8% corresponded to ischaemic heart disease, 6.6% to cerebrovascular disease, 4.3% to heart failure, and 2.9% to hypertensive disease.5 The aim of May Measurement Month 2017 (MMM17) participation in Spain was to raise awareness, treatment, and control of BP in Spain.
Methods
The MMM Spain cross-sectional survey was set up between 1st and 31st of May 2017. Volunteers were recruited through the Spanish Society of Hypertension (SEH-LELHA) and the Spanish Society of Community Pharmacy (SEFAC). Communication and distribution of the protocol, essential training material, videos, and marketing information were shared using the bespoke MMM website. Blood pressure measurements and a questionnaire about demographic, lifestyle, and cardiovascular risk factors, according to the MMM17 protocol, were carried out. Hypertension was defined as systolic BP (SBP) ≥140 mmHg and/or diastolic BP (DBP) ≥90 mmHg, or on reported current use of antihypertensive medication. Blood pressure was measured mostly with automated devices and included three seated recordings taken on the left arm. Participants with BP ≥140 and/or 90 mmHg were provided with printed evidence-based dietary and lifestyle suggestions and advice. Submitted data were analysed centrally by the MMM project team using Stata version 14.2.3
Results
The mean age of the 3849 participants was 57.4 ± 16.7 years, (39.9% males), 39.4% were taking antihypertensive medication. In total, 13.0% were diabetics, 4.7% reported a history of myocardial infarction, and 3.4% of stroke. In total, 22.5% declared alcohol consumption once or more per week, 19.8% were smokers, and 1.7% of females declared being pregnant. The mean body mass index was 26.9 kg/m2 ± 4.7.
Blood pressure decreased on average by 3.7/1.6 mmHg between the first and third BP readings. Multiple imputations were used to calculate the mean of the second and third readings based on any single reading reported.3 After imputation, of the 3848 individuals for whom data were available or known to be on antihypertensive treatment, 1923 (50.0%) participants were hypertensive. Of participants not on antihypertensive medication, 17.5% were found to have HT, while 513 (33.9%) of 1515 participants receiving treatment had uncontrolled BP.
The age and sex standardized mean BP was 120.6/74.8 mmHg. After adjustment for age and sex, significantly higher BP values in people receiving antihypertensive treatment and lower BP values in those with previous myocardial infarction and previous stroke were found (Figure 1). Systolic BP was higher in those with type 2 diabetes. Alcohol intake was associated with a significant increase in DBP (Figure 1).
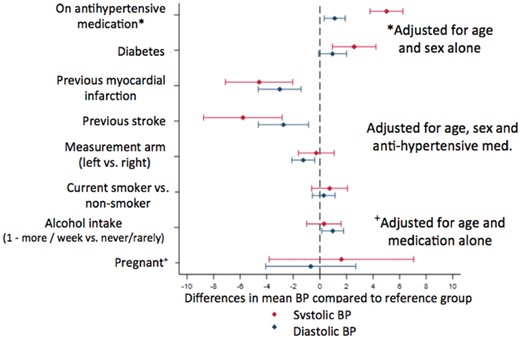
Difference in mean blood pressure according to individual characteristics from linear regression model adjusted for age, sex and, antihypertensive medication.
Obese people showed significantly higher SBP and DBP while overweighed individuals only had significantly higher SBP (Figure 2).
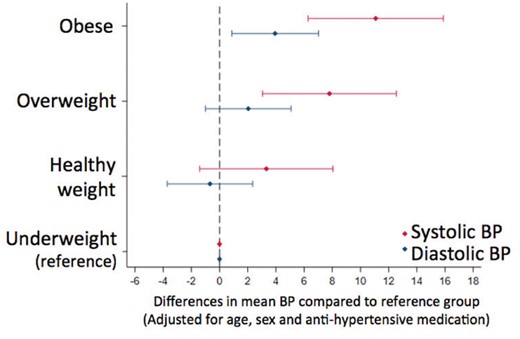
Difference in mean blood pressure according to body mass index from linear regression model, adjusted for age, sex, and antihypertensive medication, with underweight as the reference category.
Discussion
The Spanish sample was 3.5% of the European sample while, according to the objective, it should have been 9.1%.4 This discrepancy was probably due to the short preparation time of the campaign. However, the quality of the registry was adequate. The percentage of Spanish hypertensives (39.4%) was higher than previously described in Spain.3 On the other hand, it was lower than the one described by Europeans countries (55%) and in agreement with the global population (34.9%).6,7 Systolic BP mean was the same as worldwide and 3.5 mmHg lower than European; DBP was 2.0 mmHg lower than worldwide and 2.5 mmHg than European.6,7
The frequency of HT in Spanish participants who were not receiving treatment was similar to the frequency in the world population (17.5% and 17.3%, respectively), but lower than in the European population (26.3%). In individuals receiving antihypertensive medication, 33.9% had uncontrolled BP. These data are lower than the proportion of uncontrolled hypertensives worldwide (46.3%) and in the European population (63.6%).6,7
Conclusions
May Measurement Month 2017 was the largest BP screening campaign undertaken in Spain. One-third of hypertensive participants receiving treatment did not have their BP controlled. These results confirm that opportunistic screening can identify significant numbers of subjects with untreated and inadequately treated BP.
Acknowledgements
We thank all volunteers and participants.
Conflict of interest: none declared.
References
Defunciones según la causa de la muerte en España. Informe del Instituto Nacional de Estadística 2016. http://www.ine.es/prensa/np963.pdf (24 October
Las 15 causas más frecuentes de muerte en España Instituto Nacional de Estadística 2016. https://public.tableau.com/views/CAUSASDEMUERTE1/Dashboard1?:showVizHome=no&:embed=true (24 October



