-
PDF
- Split View
-
Views
-
Cite
Cite
T.J Jernberg, E.O Omerovic, E.H Hamilton, K.L Lindmark, L.D Desta, J.A Alfredsson, A.L Lundberg, T.K Kellerth, D.E Erlinge, Prevalence and prognostic impact of left ventricular systolic dysfunction after acute myocardial infarction, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.1796, https://doi.org/10.1093/ehjci/ehaa946.1796
Close - Share Icon Share
Abstract
Left ventricular dysfunction after an acute myocardial infarction (MI) is associated with poor outcome. The PARADISE-MI trial is examining whether an angiotensin receptor-neprilysin inhibitor reduces the risk of cardiovascular death or worsening heart failure (HF) in this population. The aim of this study was to examine the prevalence and prognosis of different subsets of post-MI patients in a real-world setting. Additionally, the prognostic importance of some common risk factors used as risk enrichment criteria in the PARADISE-MI trial were specifically examined.
In a nationwide myocardial infarction registry (SWEDEHEART), including 87 177 patients with type 1 MI between 2011–2018, 3 subsets of patients were identified in the overall MI cohort (where patients with previous HF were excluded); population 1 (n=27 568 (32%)) with signs of acute HF or an ejection fraction (EF) <50%, population 2 (n=13 038 (15%)) with signs of acute HF or an EF <40%, and population 3 (PARADISE-MI like) (n=11 175 (13%)) with signs of acute HF or an EF <40% and at least one risk factor (Age ≥70, eGFR <60, diabetes mellitus, prior MI, atrial fibrillation, EF <30%, Killip III-IV and STEMI without reperfusion therapy).
When all MIs, population 1 (HF or EF <50%), 2 (HF or EF <40%) and 3 (HF or EF <40% + additional risk factor (PARADISE-MI like)) were compared, the median (IQR) age increased from 70 (61–79) to 77 (70–84). Also, the proportion of diabetes (22% to 33%), STEMI (38% to 50%), atrial fibrillation (10% to 24%) and Killip-class >2 (1% to 7%) increased. After 3 years of follow-up, the cumulative probability of death or readmission because of heart failure in the overall MI population and in population 1 to 3 was 17.4%, 26.9%, 37.6% and 41.8%, respectively. In population 2, all risk factors were independently associated with death or readmission because of HF (Age ≥70 (HR (95% CI): 1.80 (1.66–1.95)), eGFR <60 (1.62 (1.52–1.74)), diabetes mellitus (1.35 (1.26–1.44)), prior MI (1.16 (1.07–1.25)), atrial fibrillation (1.35 (1.26–1.45)), EF <30% (1.69 (1.58–1.81)), Killip III-IV (1.34 (1.19–1.51)) and STEMI without reperfusion therapy (1.34 (1.21–1.48))) in a multivariable Cox regression analysis. The risk increased with increasing number of risk factors (Figure 1).
Depending on definition, post MI HF is present in 13–32% of all MI patients and is associated with a high risk of subsequent death or readmission because of HF. The risk increases significantly with every additional risk factor. There is a need to optimize management and improve outcomes for this high risk population.
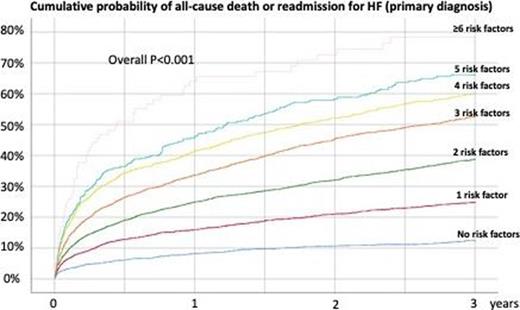
Figure 1
Type of funding source: Private company. Main funding source(s): Novartis
- heart failure, acute
- acute coronary syndromes
- myocardial infarction, acute
- angiotensins
- atrial fibrillation
- myocardial infarction
- st segment elevation myocardial infarction
- diabetes mellitus
- ventricular dysfunction, left
- heart failure
- reperfusion therapy
- follow-up
- infarction
- neprilysin
- patient readmission
- patient prognosis
- killip class
- ejection fraction
- left ventricular systolic dysfunction
- post myocardial infarction
- cox proportional hazards models
- cardiovascular death
- swedeheart registry



