-
PDF
- Split View
-
Views
-
Cite
Cite
A Pavlovic, D.G Milasinovic, Z Mehmedbegovic, D Jelic, S Zaharijev, V Zobenica, M Radomirovic, J Dudic, M Asanin, V Vukcevic, G Stankovic, Prognostic impact of atrial fibrillation in patients undergoing primary PCI with versus without left ventricular function impairment, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.2522, https://doi.org/10.1093/ehjci/ehaa946.2522
Close - Share Icon Share
Abstract
Atrial fibrillation (AF) and impaired left ventricular (LV) function have both been separately associated with increased risk of mortality following primary percutaneous coronary intervention (PCI) in patients with ST-elevation myocardial infarction (STEMI).
Our aim was to comparatively evaluate the impact of LV dysfunction and AF on the risk of mortality in primary PCI-treated patients.
This analysis included 8561 patients admitted for primary PCI during 2009–2019, from a prospectively kept, electronic registry of a high-volume tertiary center, from whom echocardiographic parameters were available. LV dysfunction was defined as EF<40%. Adjusted Cox regression models were used to assess 30-day and 1-year mortality hazard.
AF was present in 3.2% (n=273), whereas 37% had LV dysfunction (n=3189). Crude mortality rates were increased in the presence of either AF or LV dysfunction, and were the highest in the group of patients having both AF and impaired LV function, at 30 days (1.8% in no AF and no LV dysfunction vs. 5.4% if AF only vs. 7.0% if EF<40% only vs. 14.9% if AF and LV dysfunction concurrently present, p<0.001) and at 3 years (10.5% if no AF and no LV dysfunction vs. 35.8% if AF only vs. 28.5% if EF<40% only vs. 60.3% if AF and LV dysfunction both present, p<0.001). After multivariable adjustment for other significant mortality predictors, including age, previous stroke, MI, diabetes, hyperlipidemia, anemia and Killip≥2, LV dysfunction alone and in combination with AF was an independent predictor of mortality at both 30 days (HR=2.2 and HR=2.5, respectively, p<0.001 for both) and at 3 years (HR=1.9 and HR=2.9, respectively, p<0.001 for both). However, presence of AF alone, in the absence of an impaired LV function, was not independently associated with mortality at 30 days (HR 1.34, CI 95% 0.58–3.1, p=0.48), but rather at 3 years (HR 1.74, CI 95% 1.91–2.54, p=0.004).
Atrial fibrillation is associated with long-term mortality in STEMI patients undergoing primary PCI, irrespective of the LV function. Conversely, short-term prognostic relevance of atrial fibrillation in STEMI is dependent on the presence of LV dysfunction.
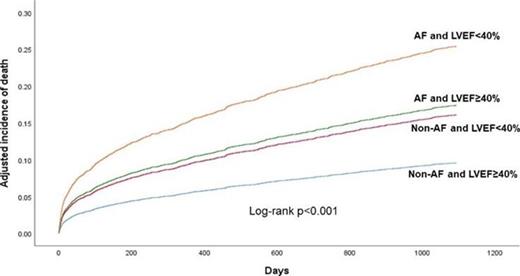
Kaplan Meier curve_AF_LV dysfunction
Type of funding source: None
- anemia
- atrial fibrillation
- percutaneous coronary intervention
- st segment elevation myocardial infarction
- ventricular function, left
- hyperlipidemia
- echocardiography
- diabetes mellitus
- ventricular dysfunction, left
- cerebrovascular accident
- ischemic stroke
- left ventricle
- diabetes mellitus, type 2
- mortality
- patient prognosis
- cox proportional hazards models



