-
PDF
- Split View
-
Views
-
Cite
Cite
J Wang, J Dai, C Fang, B Yu, Coronary plaque characteristics associated with reduced thrombolysis in myocardial infarction flow in st-segment elevation myocardial infarction patients with plaque erosion, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.2468, https://doi.org/10.1093/ehjci/ehaa946.2468
Close - Share Icon Share
Abstract
It has been reported that the lumen factors of the culprit lesions are related to Thrombolysis in Myocardial Infarction (TIMI) flow grade in ST-Segment–Elevation Myocardial Infarction (STEMI) patients, but the factors of reduced TIMI flow in plaque erosion have not been studied.
329 STEMI patients with plaque erosion who underwent pre-intervention optical coherence tomography after thrombectomy were included and divided into 2 groups according to preprocedural TIMI flow grade [TIMI 0–1 (n=219) and TIMI 2–3 (n=110)].
The patients with older age (55.7±11.1yrs vs. 51.8±10.6yrs, P=0.003) and diabetes patients (18.3% vs. 8.2%, P=0.015) had poorer TIMI flow, and the patients with reduced TIMI flow grade have lower initial cTnI (1.2ng/mL vs. 2.1ng/mL, P=0.023). The lesion in the LAD had better blood flow than the lesion in RCA (P=0.003), and the patients in TIMI 0–1 grade had more lipid plaques (53.9% vs. 41.8%, P=0.039), more macrophage (59.8% vs. 41.8%, P=0.002), and more calcification (34.2% vs. 21.8%, P=0.020). There was no statistically significant difference in the descriptive indicators of lipid or lumen between the two groups. And In a multivariate logistic regression model, the independent correlation factors of reduced TIMI flow grade in erosion patients were age, diabetes mellitus, lesion vessel, and macrophage.
In STEMI patients with plaque erosion non-lumen factors greatly affect flow, which suggests that systemic treatment is as important as local treatment for plaque erosion.
Clinical, angiographic and OCT Findings
| Variables . | Overall (n=329) . | TIMI 0–1 (n=219) . | TIMI 2–3 (n=110) . | P-value . |
|---|---|---|---|---|
| Age, years | 54.4±11.1 | 55.7±11.1 | 51.8±10.6 | 0.003 |
| Diabetes mellitus, n (%) | 49 (14.9) | 40 (18.3) | 9 (8.2) | 0.015 |
| initial cTnI, ng/mL | 1.4 (0.2–8.1) | 1.2 (0.2–5.3) | 2.1 (0.5–12) | 0.023 |
| Culprit vessel LAD, n (%) | 206 (62.6) | 128 (58.4) | 78 (70.9) | 0.003 |
| Culprit vessel RCA, n (%) | 94 (28.6) | 75 (34.2) | 19 (17.3) | 0.003 |
| Pre-MLD, mm | 0.4±0.6 | 0.1±0.3 | 1.0±0.6 | <0.001 |
| Pre-DS, % | 88.2±18.2 | 98.1±8.2 | 68.9±16.7 | <0.001 |
| Lipid plaque, n (%) | 164 (49.8) | 118 (53.9) | 46 (41.8) | 0.039 |
| Mean lipid arc, ° | 220.8±47.8 | 221.9±47.1 | 218.1±50.0 | 0.649 |
| Macrophage, n (%) | 177 (53.8) | 131 (59.8) | 46 (41.8) | 0.002 |
| Calcification, n (%) | 99 (30.1) | 75 (34.2) | 24 (21.8) | 0.020 |
| Variables . | Overall (n=329) . | TIMI 0–1 (n=219) . | TIMI 2–3 (n=110) . | P-value . |
|---|---|---|---|---|
| Age, years | 54.4±11.1 | 55.7±11.1 | 51.8±10.6 | 0.003 |
| Diabetes mellitus, n (%) | 49 (14.9) | 40 (18.3) | 9 (8.2) | 0.015 |
| initial cTnI, ng/mL | 1.4 (0.2–8.1) | 1.2 (0.2–5.3) | 2.1 (0.5–12) | 0.023 |
| Culprit vessel LAD, n (%) | 206 (62.6) | 128 (58.4) | 78 (70.9) | 0.003 |
| Culprit vessel RCA, n (%) | 94 (28.6) | 75 (34.2) | 19 (17.3) | 0.003 |
| Pre-MLD, mm | 0.4±0.6 | 0.1±0.3 | 1.0±0.6 | <0.001 |
| Pre-DS, % | 88.2±18.2 | 98.1±8.2 | 68.9±16.7 | <0.001 |
| Lipid plaque, n (%) | 164 (49.8) | 118 (53.9) | 46 (41.8) | 0.039 |
| Mean lipid arc, ° | 220.8±47.8 | 221.9±47.1 | 218.1±50.0 | 0.649 |
| Macrophage, n (%) | 177 (53.8) | 131 (59.8) | 46 (41.8) | 0.002 |
| Calcification, n (%) | 99 (30.1) | 75 (34.2) | 24 (21.8) | 0.020 |
Values are mean ± SD, median (25th, 75th percentiles), or n (%). OCT, optical coherence tomography; LAD, left anterior descending artery; LCX, left circumflex artery; and TIMI, Thrombolysis In Myocardial Infarction.
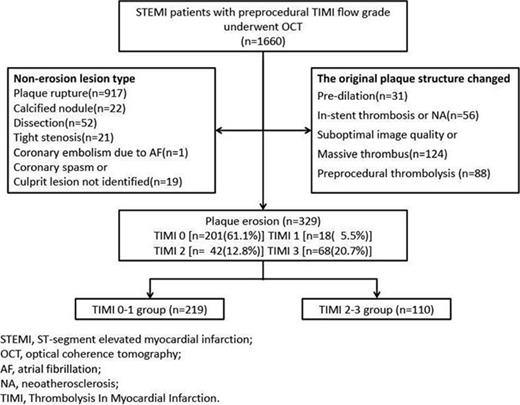
Flow Chart
Type of funding source: Foundation. Main funding source(s): National Natural Science Foundation of China (81827806, 81801861), National Key R&D Program of China (2016YFC1301100)
- angiogram
- st segment elevation myocardial infarction
- diabetes mellitus
- vascular flow
- anterior descending branch of left coronary artery
- circumflex branch of left coronary artery
- china
- macrophages
- natural sciences
- thrombectomy
- lipids
- systemic therapy
- coronary plaque
- timi grading system
- timi trial
- cardiac troponin i
- erosion
- optical coherence tomography
- calcification
- fluid flow



