-
PDF
- Split View
-
Views
-
Cite
Cite
M.G Solberg, E.N Aagaard, T Berge, P.S Roenningen, S Enger, S Nygaard, O Pervez, E.B Orstad, B.A Kvisvik, M.N Lyngbakken, H Rosjo, K Steine, A Tveit, Norwegian atrial fibrillation research network , Left atrial dysfunction and dyssynchrony in paroxysmal atrial fibrillation: data from the akershus cardiac examination 1950 study, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.0079, https://doi.org/10.1093/ehjci/ehaa946.0079
Close - Share Icon Share
Abstract
Left atrial (LA) strain measurements by speckle tracking echocardiography (STE) are predictive markers of cardiovascular morbidity, including atrial fibrillation (AF). LA mechanical dispersion (LA MD) is a new parameter derived from STE. A reduction of LA strain is considered to reflect LA dysfunction, while increased LA MD may reflect LA dyssynchrony.
To assess LA dysfunction and dyssynchrony, as measured by STE, in patients with paroxysmal AF (pAF).
A subset of 616 participants in the Akershus Cardiac Examination 1950 Study were divided into three groups: (1) A healthy group (n=179) defined by excluding AF, coronary artery disease, stroke, hypertension, chronic obstructive pulmonary disease, body mass index >30, left ventricular ejection fraction <50%, transmitral E/e' >14 or E/A >2.0, (2) A non-healthy group (n=350) of participants without pAF, but with any of the above conditions, (3) A group with pAF, but in sinus rhythm at examination (n=87). LA reservoir strain (LASr), conduit strain (LAScd) and contractile strain (LASct), as well as LA MD were assessed by STE. MD was defined as the standard deviation (SD) of time from ECG R to peak atrial longitudinal strain (SD-TPS), and corrected by RR-interval (SD-TPS/RR), expressing LA MD as a percentage of the cardiac cycle. Comparisons were made by Mann-Whitney U-test due to non-normal distributions.
Mean age was 63.5±0.5 years and 46.6% were women. LASr, LAScd and LASct were significantly lower, and LA MD significantly higher in the pAF group compared to the healthy and non-healthy groups (Table; Figure).
The present study has demonstrated LA dysfunction and dyssynchrony in patients with pAF, which may reflect LA remodeling and increased fibrosis.
Table. Echocardiographic indices
| . | Healthy (n=179) . | Non-healthy (n=350) . | pAF (n=87) . |
|---|---|---|---|
| . | Median (IQR) . | Median (IQR) . | Median (IQR) . |
| LASr (%) | 34.6 (29.2–43.3)‡ | 34.2 (28.9–42.4)‡ | 25.5 (21.3–29.9) |
| LAScd (%) | 17.0 (14.2–23.1)‡ | 16.7 (13.3–21.8)‡ | 13.7 (9.9–17.3) |
| LASct (%) | 16.8 (13.7–20.8)‡ | 17.7 (13.7–21.9)‡ | 12.9 (9.5–14.9) |
| LA MD (ms) | 31.7 (18.8–48.4)† | 31.0 (15.3–47.4)‡ | 40.2 (22.9–56.9) |
| LA MD corrected (%) | 3.1 (1.7–5.0)* | 3.0 (1.5–4.7)† | 3.8 (2.2–5.6) |
| LAVimax (ml/m2) | 24.5 (21.1–29.1)‡ | 27.6 (23.0–32.0)‡ | 31.5 (25.6–36.6) |
| . | Healthy (n=179) . | Non-healthy (n=350) . | pAF (n=87) . |
|---|---|---|---|
| . | Median (IQR) . | Median (IQR) . | Median (IQR) . |
| LASr (%) | 34.6 (29.2–43.3)‡ | 34.2 (28.9–42.4)‡ | 25.5 (21.3–29.9) |
| LAScd (%) | 17.0 (14.2–23.1)‡ | 16.7 (13.3–21.8)‡ | 13.7 (9.9–17.3) |
| LASct (%) | 16.8 (13.7–20.8)‡ | 17.7 (13.7–21.9)‡ | 12.9 (9.5–14.9) |
| LA MD (ms) | 31.7 (18.8–48.4)† | 31.0 (15.3–47.4)‡ | 40.2 (22.9–56.9) |
| LA MD corrected (%) | 3.1 (1.7–5.0)* | 3.0 (1.5–4.7)† | 3.8 (2.2–5.6) |
| LAVimax (ml/m2) | 24.5 (21.1–29.1)‡ | 27.6 (23.0–32.0)‡ | 31.5 (25.6–36.6) |
P-values versus pAF: *<0.05, †<0.01, ‡<0.001. LASr = left atrial reservoir strain, LAScd = left atrial conduit strain, LASct = left atrial contraction strain, LA MD = standard deviation of time to peak positive strain (SD-TPS), LA MD corrected = standard deviation of time to peak positive strain corrected by RR-interval (SD-TPS/RR), LAVImax = left atrial end-systolic volume, corrected by body surface area.
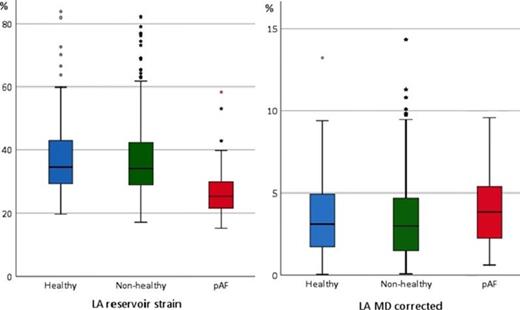
Figure 1
Type of funding source: Public Institution(s). Main funding source(s): South-Eastern Norway Regional Health Authority
- atrial fibrillation
- left ventricular ejection fraction
- coronary arteriosclerosis
- echocardiography
- body mass index procedure
- left atrium
- ventricular end-systolic volume
- tissue doppler
- conduit implant
- cerebrovascular accident
- lung diseases
- ischemic stroke
- atrium
- fibrosis
- body surface area
- cardiovascular system
- muscle contraction
- norway
- diagnostic imaging
- morbidity
- sinus rhythm
- paroxysmal atrial fibrillation
- hypertension, chronic
- cardiac cycle
- rr interval
- predictive marker
- two-dimensional speckle tracking
- longitudinal strain
- examination of heart



