-
PDF
- Split View
-
Views
-
Cite
Cite
Filippo Crea, Focus on the extreme of the spectrum: myocardial infarction with no obstructive coronary arteries and ischaemic cardiomyopathy, European Heart Journal, Volume 46, Issue 5, 1 February 2025, Pages 399–403, https://doi.org/10.1093/eurheartj/ehae891
Close - Share Icon Share
With thanks to Amelia Meier-Batschelet, Johanna Huggler, and Martin Meyer for help with compilation of this article.
 For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
This Focus Issue on ischaemic heart disease contains the State of the Art Review ‘Interplay between platelets and coagulation: from protective haemostasis to pathological arterial thrombosis’ by Gemma Vilahur from the Hospital de la Santa Creu i Sant Pau in Barcelona, Spain and Valentin Fuster from the Icahn School of Medicine at Mount Sinai in New York, NY, USA.1 The authors note that haemostasis refers to the physiological process aimed at repairing vessel injury and preventing bleeding. It involves four interlinked stages culminating in the formation of a platelet–fibrin haemostatic plug that is eventually dissolved once the vessel heals.2–4 In contrast, arterial thrombosis is a pathological condition resulting from atheroma exposure, triggering the formation of a platelet-rich thrombus that may obstruct blood flow, leading to the clinical manifestations of ischaemic cardiovascular disease. This review provides a comprehensive overview of the finely regulated endogenous antithrombotic mechanisms responsible for maintaining the haemostatic balance and preventing intravascular thrombosis. It further details the different stages and mechanisms governing the intricate interplay between the vessel, platelets, and the coagulation cascade in haemostasis, highlighting the most recent advances in platelet biology and function, to further elucidate the differential traits and players contributing to pathological arterial thrombus growth. The review also delves into the impact of emerging cardiovascular risk factors on tilting the haemostatic balance towards a prothrombotic state, thereby increasing the patient’s vulnerability to thrombotic events. Finally, it underscores the importance of early screening for subclinical atherosclerosis through advanced imaging technologies capable of quantifying plaque burden and metabolic activity since they may set the stage for an increased thrombotic risk. Implementing proactive interventions to halt atherosclerosis progression or inducing its regression at early stages is crucial for preserving haemostasis and reducing the likelihood of ischaemic atherothrombotic disease.
There is growing interest in coronary microvascular dysfunction.5–13 The microvascular resistance reserve (MRR) is a novel invasive index of the microcirculation, which is independent of epicardial stenoses, and has both diagnostic and prognostic implications. In a Fast Track Congress article entitled ‘Microvascular resistance reserve: impact on health status and myocardial perfusion after revascularization in chronic coronary syndrome’, Laust Dupont Rasmussen from the Aalborg University Hospital in Denmark, and colleagues investigate whether MRR is associated with health status outcomes in patients with moderate coronary stenoses.14 Consecutive patients with stable chest pain and moderate stenoses (30%–90% diameter reduction) on invasive coronary angiography (n = 222) underwent invasive physiology assessment. Revascularization was performed according to guideline recommendations. At baseline and follow-up, health status and myocardial perfusion were assessed by the Seattle Angina Questionnaire (SAQ) and positron emission tomography. The primary endpoint was freedom from angina at follow-up, with secondary endpoints including changes in health status by SAQ domains and myocardial perfusion by MRR, and revascularization status. Low MRR was defined as ≤3.0. Freedom from angina occurred in 38/173 patients. In multivariate analyses, a lower MRR was associated with freedom from angina at follow-up (odds ratio [OR] 0.860). In addition, patients with normal MRR who did not undergo revascularization, and patients with abnormal MRR who underwent revascularization, exhibited a significant improvement in health status. Only patients with abnormal MRR who underwent revascularization had improved myocardial perfusion (Figure 1).

Index of microcirculatory resistance reserve, health status outcomes, and myocardial perfusion. MRR, microvascular resistance reserve; CFR, coronary flow reserve; FFR, fractional flow reserve; Pa, aortic pressure; PET, positron emission tomography; SAQ, Seattle Angina Questionnaire14
Rasmussen et al. conclude that in patients with moderate coronary stenoses, MRR seems to predict the symptomatic and perfusion benefit of revascularization. The contribution is accompanied by an Editorial by Vijay Kunadian and Graziella Pompei from Newcastle University in Newcastle upon Tyne, UK.15 The authors conclude that MRR is an index specific to the coronary microcirculation. There are possibilities of integrating MRR with additional invasive indices within the framework of a standard comprehensive physiological evaluation. However, further large-scale studies are needed to determine the definitive role of MRR in patients undergoing revascularization.
In a Clinical Research article entitled ‘Low ambient temperature and incident myocardial infarction with or without obstructive coronary arteries: a Chinese nationwide study’ Jia Huang from Fudan University in Shanghai, China, and colleagues indicate that although non-optimum ambient temperature is a major non-traditional risk factor for acute myocardial infarction (MI), there is no prior knowledge on whether non-optimum ambient temperature could differentially affect MI with obstructive coronary artery disease (MI-CAD) and MI with non-obstructive coronary arteries (MINOCA).16 Using the Chinese Cardiovascular Association database-Chest Pain Center Registry, a nationwide, time-stratified, case–crossover investigation was conducted from 2015 to 2021. Meteorological data were obtained from an established satellite-based model, and daily exposures were assigned according to the onset of MI in each patient. A conditional logistic regression model combined with distributed lag non-linear models (10 days) was used to estimate the exposure–response relationships. A total of ∼84 000 MINOCA patients and ∼918 000 MI-CAD patients were included. Extremely low temperature was associated with a substantially greater risk of MINOCA (OR 1.58) than of MI-CAD (unmatched, OR 1.32; equally matched by age and sex, OR 1.25), compared with the corresponding reference temperatures. Stronger associations were observed for patients who were aged ≥65 years, female, or resided in the south. There was no significant difference for the impacts of high temperature on MINOCA and MI-CAD (Figure 2).
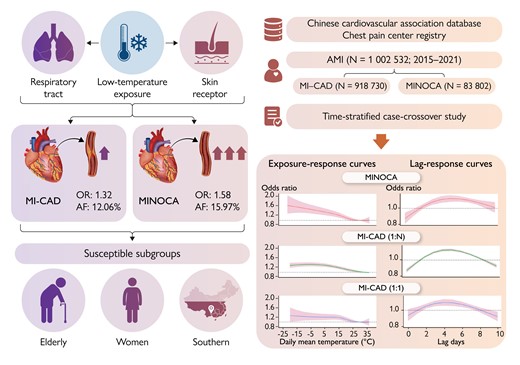
Distinct impact of low-temperature exposure on the onset of myocardial infarction with obstructive coronary artery disease and myocardial infarction with non-obstructive coronary arteries. The risk of acute myocardial infarction associated with low-temperature exposure was more pronounced in patients with myocardial infarction with non-obstructive coronary arteries than in patients with myocardial infarction with obstructive coronary artery disease. These associations were stronger in the elderly, women, and residents of the southern region. AF, attributable fraction; AMI, acute myocardial infarction; MI-CAD, myocardial infarction with obstructive coronary artery disease; MINOCA, myocardial infarction with non-obstructive coronary arteries; OR, odds ratio16
The authors conclude that this nationwide study highlights the particular susceptibility of MINOCA patients to ambient low temperature compared with that of MI-CAD patients. The contribution is accompanied by an Editorial by Magnus Bäck and Robin Hofmann from the Karolinska University Hospital in Stockholm, Sweden.17 The authors note that the definition of ‘warm enough’ for cardiovascular prevention today remains a challenge to be determined for an individual and constantly readjusted for adaptive capacity to optimize the exposure and sensitivity coupling between ambient temperature and cardiovascular event incidence.
The diagnostic indications for cardiac magnetic resonance (CMR) keep increasing.18,19 Microstructural disturbances underlie dysfunctional contraction and adverse left ventricular (LV) remodelling after ST-elevation MI (STEMI). Biphasic diffusion tensor CMR (DT-CMR) quantifies dynamic reorientation of sheetlets (E2A) from diastole to systole during myocardial thickening, and markers of tissue integrity (mean diffusivity [MD] and fractional anisotropy [FA]). In a Clinical Research article entitled ‘Characterization of dynamic changes in cardiac microstructure after reperfused ST-elevation myocardial infarction by biphasic diffusion tensor cardiovascular magnetic resonance’, Ramyah Rajakulasingam from the Imperial College London in the UK, and colleagues investigated whether microstructural alterations identified by biphasic DT-CMR: (i) enable contrast-free detection of acute MI; (ii) associate with severity of myocardial injury and contractile dysfunction; and (iii) predict adverse LV remodelling.20 Biphasic DT-CMR was acquired 4 days (n = 70) and 4 months (n = 66) after reperfused STEMI and in healthy volunteers (HVOLs) (n = 22). Adverse LV remodelling was defined as an increase in LV end-diastolic volume ≥20% at 4 months. Widespread microstructural disturbances were detected post-STEMI. In the acute MI zone, diastolic E2A was raised and systolic E2A reduced, resulting in reduced E2A mobility (all P < .001 vs. adjacent and remote zones and HVOLs). Acute global E2A mobility was the only independent predictor of adverse LV remodelling (OR 0.77; P = .010). MD and FA maps had excellent sensitivity and specificity (all >90%) and interobserver agreement for detecting MI presence and location.
Rajakulasingam and colleagues conclude that biphasic DT-CMR identifies microstructural alterations in both diastole and systole after STEMI, enabling detection of MI presence and location as well as predicting adverse LV remodelling. DT-CMR has the potential to provide a single contrast-free modality for MI detection and prognostication after acute STEMI. This manuscript is accompanied by an Editorial by Sven Plein and Erica Dall’Armellina from the University of Leeds in the UK.21 The authors highlight that dynamic information of the microstructure provided by biphasic DT imaging is an exciting addition to the already broad array of CMR methods to assess the impact of acute MI on remodelling and outcomes. While still in the early stages of its development, the study by Rajakulasingam et al. confirms the potential of cardiac DT imaging as a unique tool for risk stratification that allows us to see the small things that may matter most in remodelling and recovery post-MI.
The diagnostic work-up in supsected angina is highly debated.22 Whether index testing using coronary computed tomography angiography (CTA) improves outcomes in stable chest pain is debated. The risk factor-weighted clinical likelihood (RF-CL) model provides likelihood estimation of obstructive CAD. In another Clinical Research article entitled ‘Clinical risk prediction, coronary computed tomography angiography, and cardiovascular events in new-onset chest pain: the PROMISE and SCOT-HEART trials’, Laust Dupont Rasmussen from the Aalborg University in Denmark, and colleagues investigated the prognostic effect of coronary CTA vs. usual care by RF-CL estimates.23 Large-scale studies randomized ∼14 000patients with stable chest pain to coronary CTA as part of the initial work-up in addition to or instead of usual care including functional testing. Patients were stratified according to RF-CL estimates (RF-CL: very low [≤5%], low [>5%–15%], and moderate/high [>15%]). The primary endpoint was MI or death at 3 years. The primary endpoint occurred in 2.3% of patients. Event rates were similar in patients allocated to coronary CTA vs. usual care. Overall, 33, 44, and 23% of patients had very low, low, and moderate/high RF-CL. Risk was similar in patients with very low or moderate/high RF-CL allocated to coronary CTA vs. usual care. Conversely, patients with low RF-CL undergoing coronary CTA had lower event rates (hazard ratio [HR] 0.67). The number needed to test using coronary CTA to prevent one event within 3 years was 143.
The authors conclude that despite an overall good prognosis, low RF-CL patients have reduced risk of MI or death when allocated to coronary CTA vs. usual care. Risk is similar in patients with very low and moderate/high likelihood. The contribution is accompanied by an Editorial by Bruna R. Scarpa Matuck and Armin Arbab-Zadeh from Johns Hopkins University School of Medicine in Baltimore, MD, USA.24 The authors conclude by indicating that MI risk is consistently lower for patients undergoing coronary CTA compared with stress testing, regardless of the initial risk level. While the effect is smaller in populations with less disease and may not be evident with short follow-up, it nevertheless will be relevant for preventing MIs in thousands of patients among the millions tested for CAD each year. The authors believe that symptomatic patients (requiring CAD testing) should not be deprived of the opportunity to detect their coronary atherosclerotic disease burden and to lower their risk through effective prevention.
In a Rapid Communications article entitled ‘Prognostic impact of inducible ischaemia in ischaemic cardiomyopathy: the REVIVED-BCIS2 trial’, Divaka Perera from King’s College London in the UK, and colleagues note that retrospective observational data suggest that the presence and extent of inducible myocardial ischaemia predicts future adverse cardiac events in patients with ischaemic heart disease.25 However, several randomized trials have failed to identify an association between the burden of inducible ischaemia and outcomes in patients with stable CAD assigned to medical therapy alone or revascularization. Despite this, the presence and extent of ischaemia is commonly used to guide revascularization of stable patients. Notably, many of these analyses excluded patients with impaired LV function. Patients enrolled in REVIVED-BCIS2 trial were eligible for inclusion in this analysis if they had undergone stress perfusion CMR prior to randomization. Visual segmental assessment of myocardial perfusion and late gadolinium enhancement transmurality was performed at an independent core laboratory blinded to trial group assignment and clinical data. Segmental ischaemia was classified in a binary manner, and the patient-level ischaemic burden was expressed in relation to total LV mass, defined as (number of ischaemic segments)/16 × 100. The primary composite outcome was all-cause death or aborted sudden death (defined as an appropriate implantable cardioverter defibrillator therapy or a resuscitated cardiac arrest). In total, 200 of 700 REVIVED patients underwent stress perfusion CMR, of which 181 were of sufficient diagnostic quality to be included in this analysis. At a median of 42 months, a primary outcome event had occurred in 36 of 91 participants in the percutaneous coronary intervention (PCI) arm, and 31 of 90 in the optimal medical therapy (OMT) arm (40% vs. 34%, HR 1.20, P = .49). There was no relationship between ischaemic burden, outcomes, and randomized treatment allocation.
The authors conclude that the REVIVED-BCIS2 cohort is the largest to date of stress perfusion CMR in severe ischaemic LV dysfunction, randomized to PCI and OMT, versus OMT alone. In this cohort, ischaemic burden is not associated with clinical outcomes. Furthermore, no association is seen between ischaemic burden, clinical outcomes, and randomized treatment assignment.
The editors hope that this issue of the European Heart Journal will be of interest to its readers.
Dr. Crea reports speaker fees from Abbott, Amgen, Astra Zeneca, BMS, Chiesi, Daiichi Sankyo, Menarini outside the submitted work.




