-
PDF
- Split View
-
Views
-
Cite
Cite
Helmut Baumgartner, Bernard Iung, David Messika-Zeitoun, The Year in Cardiovascular Medicine 2024: the top 10 papers in valvular heart disease, European Heart Journal, Volume 46, Issue 18, 7 May 2025, Pages 1702–1704, https://doi.org/10.1093/eurheartj/ehaf071
Close - Share Icon Share
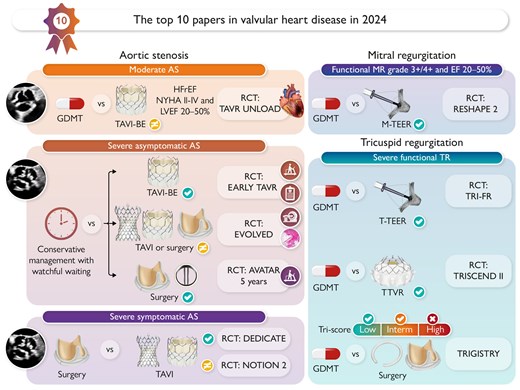
The top 10 papers in valvular heart disease in 2024. AS, aortic stenosis; BE, balloon expandable; EF, ejection fraction; GDMT, guideline-directed medical therapy; HFrEF, heart failure with reduced ejection fraction; MR, mitral regurgitation; M-TEER, mitral transcatheter edge-to-edge repair; RCT, randomized controlled trial; TAVI, transcatheter aortic valve implantation; TR, tricuspid regurgitation; T-TEER, tricuspid transcatheter edge-to-edge repair; TTVR, transcatheter tricuspid valve replacement. RCTs:  means superiority and
means superiority and  no difference between groups; registry:
no difference between groups; registry:  means superiority,
means superiority,  benefit in subgroups, and
benefit in subgroups, and  no difference.
no difference.
Introduction
With further increasing numbers of publications this year including an unusually high number of randomized controlled trials (RCTs), we had a very difficult task to select the 10 ‘best’ papers on valvular heart disease. We restricted our selection to publications in the New England Journal of Medicine, Journal of the American Medical Association, Lancet, European Heart Journal, Circulation, and Journal of the American College of Cardiology. The 10 papers were chosen based on a consensus between the three authors, weighting quality, potential impact on clinical practice and future research as well as expected interest for our readership. We acknowledge that many more would have deserved to be mentioned.
Intervention in asymptomatic severe aortic stenosis
The management of asymptomatic severe aortic stenosis (AS) remains controversial, with three RCTs published this year addressing this critical question.1–3 The extended follow-up (median 63 months) of AVATAR which enrolled 157 relatively young patients at low surgical risk [mean age 67 years, median Society of Thoracic Surgeons (STS) score 1.7%, and normal exercise test] continued to demonstrate better clinical outcomes with early surgical aortic valve replacement (SAVR) over clinical surveillance with regard to its primary composite endpoint—all-cause death, acute myocardial infarction, stroke, or unplanned hospitalization for heart failure (23% vs. 47%, P = .002), all-cause mortality, and HF hospitalizations but not cardiovascular mortality.1 EARLY TAVI2 randomly assigned 901 patients (mean age 76 years, median STS score 1.8%, and 84% low surgical risk) to undergo early transfemoral transcatheter aortic valve implantation (TAVI) or close clinical surveillance. The primary endpoint, a composite of death, stroke, or unplanned hospitalization for cardiovascular causes occurred in 27 vs. 45% (P < .001). However, this difference was mainly driven by less hospitalizations while death rate was similar (8.4% vs. 9.2%). After a median follow-up of 3.8 years, 87% of patients in the conservative group eventually underwent TAVI with no differences in procedure-related adverse events compared to the early TAVI group. Finally, EVOLVED3 randomized 224 patients (mean age 73 years) with severe asymptomatic AS (no mandatory exercise testing) but proven myocardial fibrosis (midwall late gadolinium enhancement in magnetic resonance imaging) to early intervention (TAVI or SAVR) or clinical surveillance. The trial was terminated early because of recruitment difficulties (originally planned sample size 356 patients). The primary outcome, a composite of all-cause death or unplanned AS-related hospitalization, did not differ between arms (18% vs. 23%, P = .44). Rate of all-cause death was similar (14% vs. 13%) while unplanned AS-related hospitalization tended to be lower with early intervention (6% vs. 17%). Critically, there were marked differences between the three RCTs in the delay between randomization and early intervention (median 55 days in AVATAR, 14 days in Early-TAVR, and 5 months in EVOLVED) and in the incidence of interventions in the conservative groups. Taken together, current evidence suggests that an early intervention in patients with severe asymptomatic AS is safe leads to a significant reduction of unplanned hospitalizations but does not seem to provide a consistent improvement in survival and thus could be considered in selected low-risk patients’ subsets. It is also critical to balance these short- or mid-term results with long-term risks (prosthetic valve related complications, re-intervention), and longer follow-up comparing the two strategies is clearly needed.
Transcatheter or surgical treatment of aortic stenosis
Transcatheter aortic valve implantation is increasingly performed in AS and expanding to younger patients at low surgical risk causing an ongoing debate. This year, two further RCTs addressing this hot topic were published.4,5 The academic-funded trial, DEDICATE,4 randomized 1414 patients with low to intermediate surgical risk (mean age 74 years; median STS score 1.8%). The primary outcome, a composite of all-cause death or fatal or nonfatal stroke at 1 year, occurred in 5.4% with TAVI vs. 10.0% with SAVR (P < .001 for noninferiority). The incidence of death from any cause was 2.6% and 6.2%, respectively. The study by design demonstrated noninferiority but surprised by the magnitude of the differences favouring TAVI. NOTION-25 randomized 370 low-risk patients (mean STS score 1.1%) aged ≤75 years (mean 71) and was the first RCT also including patients with bicuspid valves (n = 100). The risk of the primary endpoint, a composite of all-cause mortality, stroke, or rehospitalization at 12 months was not statistically different for the entire population although numerically higher for TAVI (10.2% vs. 7.1%). Patients with TAVI had lower risk of major bleeding and new-onset atrial fibrillation and higher risk of non-disabling stroke, permanent pacemaker implantation, and moderate or greater paravalvular regurgitation. Although not statistically powered for such analyses, the risk of the primary endpoint was similar between groups in patients with tricuspid valves (8.7% vs. 8.3%) but markedly worse for TAVI in those with bicuspid valves (14.3% and 3.9%). Taken together, short-term results for TAVI in ‘younger’ low-risk patients seem to be comparably or even better than for SAVR in tricuspid valves while caution is warranted and further research required for patients with bicuspid valves. Longer follow-up and lifetime considerations (expected re-interventions and TAVI explantations) are even more critical to consider in the younger AS population.
Intervention in moderate aortic stenosis patients with HF
Neurohormonal modulation and afterload reduction are key for treatment of HF with reduced ejection fraction. In patients with concomitant moderate AS, TAVI may therefore be complementary to guideline-directed medical therapy (GDMT). TAVI-UNLOAD is the first RCT addressing this important question but was prematurely stopped after enrolment of 178 patients (mean age 77 years, 56% in NYHA class III or IV).6 Transcatheter aortic valve implantation was associated with better quality of life but not superior to surveillance for the primary endpoint which was the hierarchical occurrence of: (i) all-cause death; (ii) disabling stroke; (iii) disease-related hospitalizations and HF equivalents; and (iv) improvement of quality-of-life score (win-ratio 1.3, P = .14). In addition to its small sample size, 43% of patients in the conservative group underwent TAVI within a median of 12 months mostly because of progression to severe AS. There are more ongoing RCTs evaluating the benefit of TAVI in moderate AS.
Transcatheter edge-to-edge repair in ventricular secondary mitral regurgitation
With two contradictory RCTs, it has remained controversial whether mitral transcatheter edge-to-edge repair (TEER) improves outcome in patients with HF and secondary mitral regurgitation (SMR). RESHAPE 27 randomized 505 patients with HF and 3+/4+ SMR to mitral TEER and GDMT or GDMT alone. Intervention was superior in its three primary endpoints: the rate of first or recurrent hospitalization for HF or cardiovascular death at 24 months (37% vs. 60%, P = .002), first or recurrent hospitalization for HF during 24 months (27% vs. 47%, P = .002), and the change between baseline and 12 months in health status. Although this is formally a positive trial, there was no difference in all-cause and cardiovascular mortality as well as overall hospitalizations. There are also concerns regarding methodology (multiple simultaneous tests), the prolonged 8-year recruiting period with multiple protocol modifications, assessment of MR severity, and medical treatment issues. Thus, this study does not end the debate but rather re-stimulate discussions.
Transcatheter and surgical treatment of tricuspid regurgitation
Whether tricuspid TEER can improve outcome—in particular survival—in patients with severe isolated tricuspid regurgitation (TR) remains uncertain. TRI-FR8 randomized 300 patients (mean age 78 years) to tricuspid TEER and GDMT or GDMT alone. The primary outcome was a composite clinical endpoint comprising change in NYHA class, change in patient global assessment, or occurrence of major cardiovascular events at 1 year expressed in a score which improved in 74% of patients with intervention and 41% with GDMT alone (P < .001). The hierarchical composite endpoint of time to death or tricuspid valve surgery, or HF hospitalizations, and improvement of ≥15 points in quality-of-life score at 1 year also favoured TEER with a win ratio of 2.06 (P < .001). There was, however, no difference in rates of survival or major cardiovascular events, and the positive results were mainly driven by improved patient-reported outcome measures.
Transcatheter tricuspid valve implantation (TTVI) is more effective in reducing TR than TEER and may therefore be associated with better outcome. TRISCEND II9 randomized 2:1 patients with severe TR to either TTVI with GDMT (n = 267) or GDMT alone (n = 133). Using a complex hierarchical composite primary outcome of death from any cause, implantation of a right ventricular assist device or heart transplantation, tricuspid-valve intervention, hospitalization for HF, improvement in quality-of-life score, in NYHA functional class, and in 6 min walk distance at 1 year, the win ratio favouring TTVI was 2.02 (P < .001). This was again driven primarily by improvements in symptoms and quality of life while no improvement in survival or significant reduction in HF hospitalization was found. Thirty-day mortality rate was 3.5%, severe bleeding 10.4%, and new pacemaker implantation rate 24%.
These studies indicate once more that patients’ selection is crucial in order to improve the outcome of patients with severe TR. In the international cohort TRIGISTRY,10 survival rates up to 10 years of patients who underwent isolated tricuspid valve surgery (repair or replacement) and those conservatively managed were compared overall and according to TRI-SCORE category (low: ≤3, intermediate: 4–5, and high: ≥6). This score originally developed to predict operative mortality reflects disease stage including signs of cardiac and second organ damage. Higher survival rates were observed with repair than replacement and benefit of intervention declined as TRI-SCORE increased with no benefit of any type of surgery in the high TRI-SCORE category. These results emphasize the importance of timely intervention and patient selection to achieve the best outcomes as well as the need for further RCTs.
Declarations
Disclosure of Interest
H.B. and B.I. have nothing to declare. D.M.-Z. declares: research grants from Edwards Lifesciences, consulting fees from Predisuge, honoraria for lectures from Abbott, and Participation on a Data Safety Monitoring Board/Advisory Board for TWIST.



