-
PDF
- Split View
-
Views
-
Cite
Cite
D Garcia Vega, S Cinza-Sanjurjo, P Mazon-Ramos, D Rey-Aldana, M Portela-Romero, M Rodriguez-Manero, M Sestayo-Fernandez, R Lage-Fernandez, R Lopez-Lopez, J R Gonzalez-Juanatey, Electronic consultation from primary care to a cardiology department improves outcomes in patients with cancer, European Heart Journal, Volume 45, Issue Supplement_1, October 2024, ehae666.3546, https://doi.org/10.1093/eurheartj/ehae666.3546
Close - Share Icon Share
Abstract
The number of cancer patients with known cardiovascular (CV) disease is increasing due to improved cancer prognosis.
The objective of this study is to assess the long-term results of cancer patients referred to a cardiology department by primary care using electronic consultation (e-consultation).
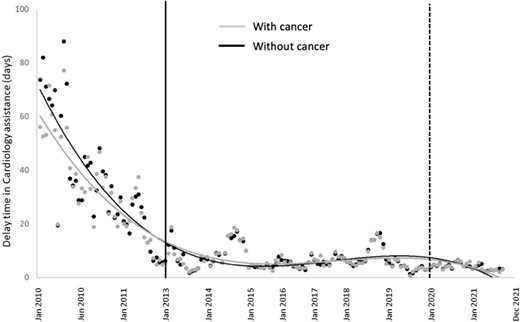
We analysed the patients with previous diagnosis of cancer referred to a cardiology department (CD) from 2010 to 2021 (n=6.889), selected from a total of 68.518 patients (61.629 without cancer), and compared two assistance models: in-person practice (from 2010 to 2012) and e-consultation (from 2013 to 2021). In the first period, all the patients referred by primary care physicians (PCPs) were seen in an in-person consultation and in the e-consultation model the cardiologist reviewed the electronic records (e-consultation) and decided to solve without any visit or, if it was necessary, with an in-person consultation. The outcomes between both periods were analysed using an interrupted time series regression model: 1) delay time to cardiology assistance; 2) all-cause and cardiovascular hospital admissions, and 3) all-cause and cardiovascular mortality during the first year after the initial consultation or e-consultation to the CD.
Among cancer patients referred to cardiology consultation, the introduction of e-consultation decreased waiting times to cardiology care by 51,8% (95% CI: 51,7%-51,9%) (Fig 1). Over 60% of referrals were resolved in less than 8 days, with this proportion significantly higher after the e-consultation program was introduced (p<0,001). Furthermore, we observed a reduction in the one-year rate of outcomes, with an incidence rate ratio (iRR) [IC 95%] of 0,75 [0,73-0,77] for CV-related hospitalizations (Fig 2b), 0,43 [0,42-0,44] for all-cause hospitalization (Fig 2a), and 0,87 [0,86-0,88] for all-cause mortality. In the multivariate analysis, the delay in receiving cardiology care was significantly associated with an independent increase in 1-year mortality (OR [95% CI] 1,39 [1,06-1,83]) and hospital admission (OR [95% CI] 1,25 [1,02-1,52]). Furthermore, the implementation of the e-consult model was associated with a reduction in hospital admission rates (OR [95% CI] 0,19 [0,14-0,25]).

Author notes
Funding Acknowledgements: None.



