-
PDF
- Split View
-
Views
-
Cite
Cite
R Sun, J Wang, M Li, G Y H Lip, B Liu, Y Pan, L Zhang, R Sun, Association of insulin resistance with cardiovascular disease and all-cause mortality in type 1 diabetes mellitus: systematic review and meta-analysis, European Heart Journal, Volume 45, Issue Supplement_1, October 2024, ehae666.2920, https://doi.org/10.1093/eurheartj/ehae666.2920
Close - Share Icon Share
Abstract
Insulin resistance (IR) is a key factor in the pathogenesis of type 2 diabetes mellitus (T2DM) and is associated with a higher risk of cardiovascular disease (CVD) and mortality. However, the association between IR and these outcomes in type 1 diabetes mellitus (T1DM) is less clear. This systematic review and meta-analysis aimed to investigate the associations between CVD outcomes and IR in T1DM.
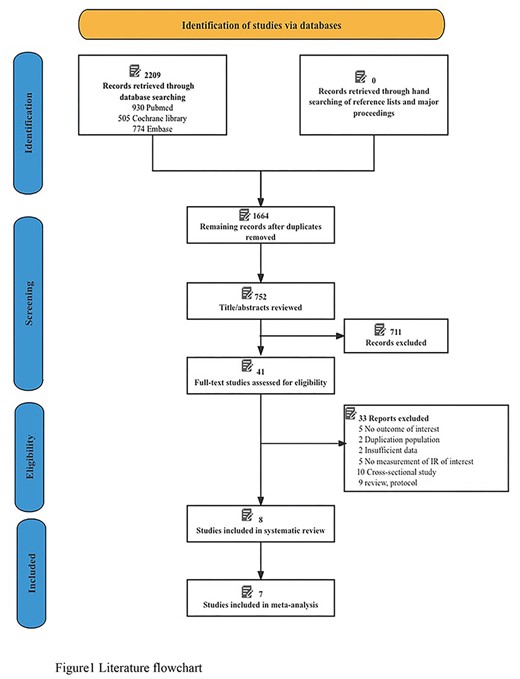
PubMed, EMBASE, and the Cochrane Library databases were searched from inception to 15 March 2023 and updated on 31 October 2023. Observational studies (cohort studies or post hoc analysis of clinical trials) reporting the associations between IR measured by estimated glucose disposal rate (eGDR) level and the risk of CVD and all-cause mortality in individuals with T1DM were eligible. Data, pooled by random effects models, were presented as hazard ratios (95% confidence intervals, CI). The primary outcomes were the composite CVD outcome and all-cause mortality.
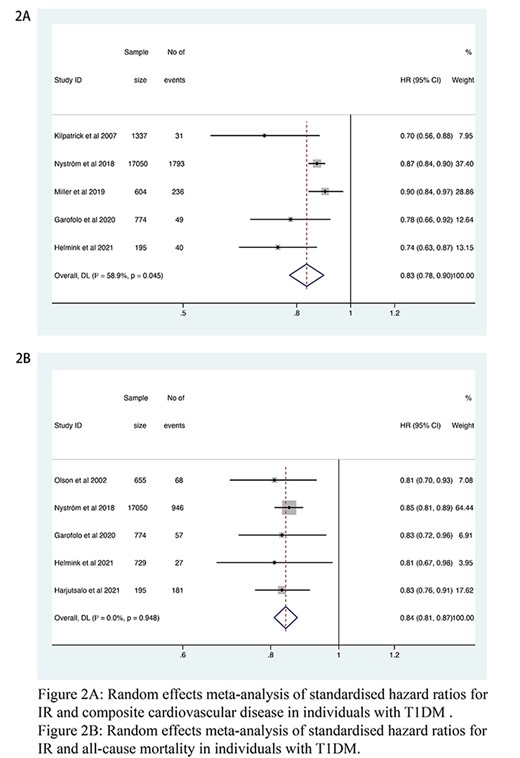
Eight studies involving 21,930 individuals were included, of which five studies involving 19,960 T1DM individuals reported the risk of CVD. During a median follow-up of 10 years, there were 2,149 cases of incident CVD. The pooled hazard ratio for composite CVD outcome per 1-unit increase in the eGDR index was 0.83 (95% CI 0.78–0.90, I2 = 58.9%). Five studies involving 19,403 T1DM individuals reported the risk of all-cause mortality. During a median follow-up of 10 years, a total of 1,279 deaths were observed. The pooled hazard ratio for all-cause mortality per 1-unit increase in the eGDR index was 0.84 (95% CI 0.81–0.87, I2 = 0%).
Author notes
Funding Acknowledgements: Type of funding sources: Public grant(s) – National budget only. Main funding source(s): This work was supported by the National Key R&D Program of China (Grant No. 2022YFC3500101).



