-
PDF
- Split View
-
Views
-
Cite
Cite
M Chen, Y Ning, C Zhao, J An, M Tang, G Tse, S Chan, X Lei, H Qiang, H Yu, C Bai, Y Yan, D Wang, G Li, Degree of joint risk factor control and incident all cause dementia in hypertensive patients, European Heart Journal, Volume 45, Issue Supplement_1, October 2024, ehae666.2603, https://doi.org/10.1093/eurheartj/ehae666.2603
Close - Share Icon Share
Abstract
Hypertension (HT) is a known modifiable risk factor for dementia. This study evaluates the impact of effectively controlling multiple modifiable risk factors in HT patients on the incidence of dementia.
Data from the UK Biobank (2006-2010) were used in this longitudinal study, including essential HT patients and non-HT participants, excluding those with pre-existing dementia or less than two years of follow-up. The study focused on seven risk factors: physical activity, smoking status, blood pressure, body mass index, glycosylated hemoglobin levels, lipids, and urinary Albumin-to-Creatinine Ratio. The Cox model evaluated the association between the degree of risk factor control and the incidence of dementia, while linear regression models analyzed the brain abnormalities among different risk factor control groups.
Of 291,720 participants, 86,675 had HT. Over a median follow-up of 14.3 years, dementia developed in 2,002 HT and 1,379 non-HT participants. Compared with non-HT individuals, a gradual decrease in dementia risk in HT patients with the number of well-controlled risk factors was observed (hazard ratio: 2.01 [95% confidence interval (CI) 1.73-2.34] to 1.25 [95% CI 1.13-1.40]). While within HT patients, with the highest level of control lowering the risk to 0.63 (95% CI [0.54-0.73]). Moreover, HT patients with better well-controlled risk factors had lower geometric mean for white matter hyperintensity volume and increased total brain parenchymal volume, gradually narrowing the gap with non-HT individuals.
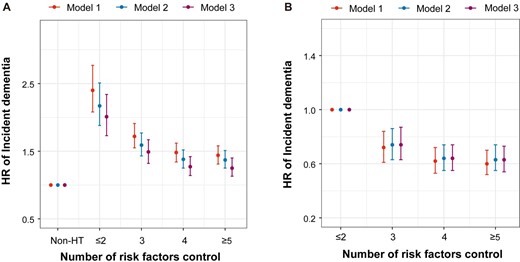
HRs of all-cause dementia in patients
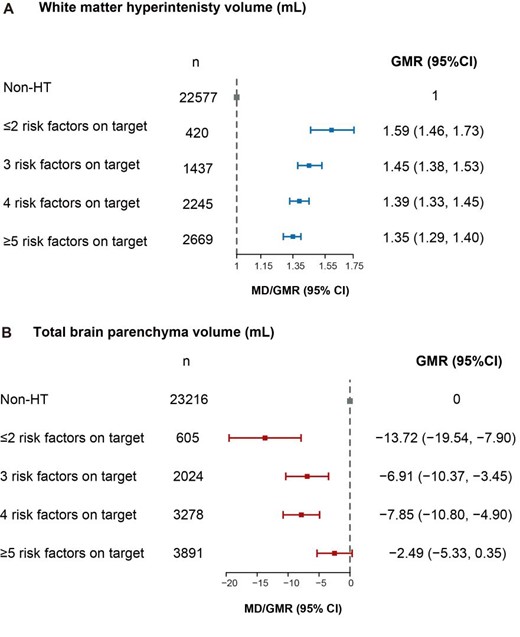
GMRs of different risk factors on target
Author notes
Funding Acknowledgements: Type of funding sources: Public hospital(s). Main funding source(s): This research was supported by the Clinical Research Award of the First Affiliated Hospital of Xi'an Jiaotong University, China.



