-
PDF
- Split View
-
Views
-
Cite
Cite
E C I Woelders, D A M Peeters, S Janssen, J J P Luijkx, P J C Winkler, P Damman, W S Remkes, A W J Van 'T Hof, R J M Van Geuns, The ZON-HR investigators, Complex versus non-complex, should we adjust the antiplatelet strategy to the type of percutaneous coronary intervention? Results from a real world PCI population, European Heart Journal, Volume 45, Issue Supplement_1, October 2024, ehae666.2394, https://doi.org/10.1093/eurheartj/ehae666.2394
Close - Share Icon Share
Abstract
Personalized dual antiplatelet treatment (DAPT) using risk stratification is key to minimize bleeding- and ischemic events after percutaneous coronary intervention (PCI). Known ischemic risk factors include complex procedures which are integrated in the recommendation for extended DAPT in patients with additional ischemic risk factors.
We aimed to provide insight whether a complex PCI (CPCI) should be regarded as an individual risk factor, regardless of other risk factors, to adjust the antiplatelet strategy. Also, we determined the effect of DAPT duration and choice of P2Y12 inhibitor on outcomes.
We included patients from the South East (Zuid Oost) Netherlands Heart Registry (ZON-HR) and excluded patients using oral anticoagulants. This PCI registry prospectively collects baseline-, procedural- and follow-up data including medication use and the intended DAPT duration. Patients were stratified to non-CPCI or CPCI comprising of bifurcation lesions with two stents, venagraft PCI, chronic total occlusion (CTO) or ≥ 60mm stent. Analyses were conducted using Cox regression analysis. Multivariate analysis was performed to adjust for risk factors and baseline differences.
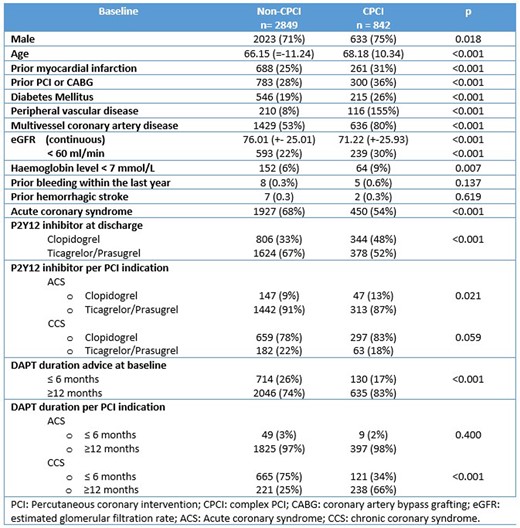
We included 3691 patients (842 CPCI). Table 1 demonstrates the baseline characteristics and DAPT strategy. CPCI was more often required in patients with a high ischemic risk profile based on the extensiveness of atherosclerosis and comorbidities. Non-CPCI patients more often underwent PCI for acute coronary syndrome.
Outcomes are presented in table 2. Compared to non-CPCI, CPCI increased the risk of major adverse cardiac and cerebral events (MACCE) in the second half of the year as opposed to bleeding events, which more often occurred in the first months after CPCI, driven by access site bleedings (73% in CPCI versus 56% in non-CPCI, p=0.01). All-cause mortality was higher during the overall follow-up period after a CPCI compared to non-CPCI. These findings remain significant when corrected for additional risk factors in both groups.
In patients with CPCI, treatment with ticagrelor or prasugrel strongly reduced MACCE between 6-12 months when compared to clopidogrel (multivariate HR: 0.28, 95% CI: 0.08-0.98), but did not influence bleeding events or all-cause mortality. No effect of extended DAPT was observed.
Author notes
Funding Acknowledgements: None.
- acute coronary syndromes
- atherosclerosis
- anticoagulants, oral
- clopidogrel
- percutaneous coronary intervention
- stents
- ischemia
- hemorrhage
- comorbidity
- follow-up
- netherlands
- brain
- heart
- mortality
- drug usage
- stratification
- cox proportional hazards models
- prasugrel
- ticagrelor
- risk of excessive or recurrent bleeding
- p2y12 receptor antagonists
- site of access
- dual anti-platelet therapy




