-
PDF
- Split View
-
Views
-
Cite
Cite
L Oberg Arouca Bassoli, V E E Rosa, L J N T Pires, P N Cavalvante, C E Rochitte, M P Lopes, J R C Fernandes, R O Sampaio, F Tarasoutchi, Postoperative assessment of interstitial myocardial fibrosis in aortic valve pathologies: insights from a cardiac magnetic resonance study, European Heart Journal, Volume 45, Issue Supplement_1, October 2024, ehae666.1782, https://doi.org/10.1093/eurheartj/ehae666.1782
Close - Share Icon Share
Abstract
Data on the characteristics of diffuse myocardial fibrosis (DMF) among patient undergoing valve surgery for aortic regurgitation (AR), high-gradient aortic stenosis (HG-AS), and low-flow low-gradient aortic stenosis with low ejection fraction (LFLG-AS) are limited.
To assess the postoperative characteristics of DMF and to compare post- and pre-operative cardiac magnetic resonance imaging (CMR) data.
Patients diagnosed with AR (38), HG-AS (62), and LFLG-AS (39), who met criteria for surgical intervention, were prospectively included. Pseudo-severe AS was excluded. Post-operative CMR was performed 6 to 8 months after surgery, and a comparison between post- and pre-operative data was made (delta=Δ). Quantitative analysis included assessment of extracellular volume fraction (ECV), indexed ECV (iECV), and myocardial mass (MM).
There were differences in baseline characteristics among patients with AR, HG-AS, and LFLG-AS concerning age (54±14 vs 63±8 vs 67±8 years, respectively; p<0.01), male gender (75% vs 50% vs 82%, respectively; p<0.01), NYHA functional class III and IV (37.5% vs 55.2% vs 30.8%, respectively; p=0.03), EuroSCORE II (1.16±0.5 vs 1.26±0.46 vs 3.39±2.65%, respectively; p<0.01), and STS (0.74±0.29 vs 1.11±0.5 vs 3.21±2.11%, respectively; p<0.01). Global ECV was similar between groups (29.2±5.6 vs 27.0±3.6 vs 29.4±5.9%, respectively; p=0.01), MM was different between groups (215±76 vs 161±51 vs 203±51g, respectively; p<0.01), and iECV was different between groups and significantly higher in AS patients (50.1±31.0 vs 21±8 vs 34.2±10.2ml/m², respectively; p<0.01). All patients underwent valve surgery and there were differences regarding extracorporeal circulation time (94±25 vs 97±20 vs 75±41min, respectively; p<0.01), and 30-day mortality (0% vs 3% vs 15%, respectively; p<0.01). Post-surgery data from patients with AR (32), HG-AS (62), and LFLG-AS (21) demonstrated a comparable decrease across all groups concerning preoperative MM (ΔMM: -39.3±41.5 vs -33.4±30.9 vs -23.4±34.2g, respectively; p=0.36) (Figure 1). In contrast, iECV decreased post-surgery only in AR, remaining stable in HG-AS and LFLG-AS (ΔiECV: -19.1±22.5 vs -1.4±7.4 vs 0.9±12ml/m², respectively; p<0.01). Thus, postoperative ECV maintained commensurate values in AR, while increasing in HG-AS and LFLG-AS (ΔECV: -0.1±4.5 vs 1.5±5.1 vs 2.9±4.9%, respectively; p=0.09). Δ left ventricular ejection fraction (LVEF) was similar across groups (ΔLVEF: -1.5±10.6 vs 1.1±11.7 vs 2.6±16%, respectively; p=0.44).
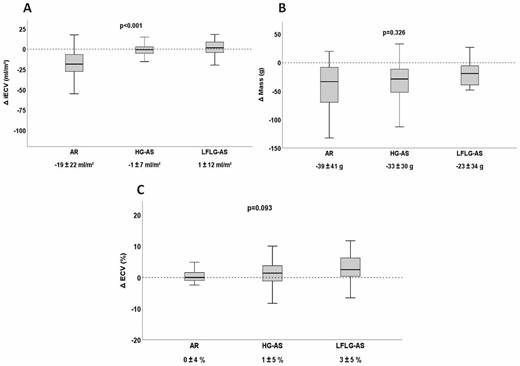
Delta iECV, LV mass and ECV measures
Author notes
Funding Acknowledgements: None.
- aortic valve
- aortic valve insufficiency
- aortic valve stenosis
- myocardium
- phenotype
- left ventricular ejection fraction
- myocardial fibrosis
- extracorporeal circulation
- male
- preoperative care
- surgical procedures, operative
- mortality
- ejection fraction
- external cephalic version
- cardiac mri
- new york heart association classification
- heart valve surgery
- european system for cardiac operative risk evaluation
- fluid flow



