-
PDF
- Split View
-
Views
-
Cite
Cite
D Munhoz, C Collet, T Mizukami, J Sonck, H Matsuo, H Ando, K Sakai, T Storozhenko, C Berry, D Perera, E Christiansen, T Shinke, B Ko, B De Bruyne, N Johnson, PPG Global Study Team, Influence of pathophysiological patterns of coronary artery disease on the safety and efficacy of percutaneous coronary intervention, European Heart Journal, Volume 45, Issue Supplement_1, October 2024, ehae666.1396, https://doi.org/10.1093/eurheartj/ehae666.1396
Close - Share Icon Share
Abstract
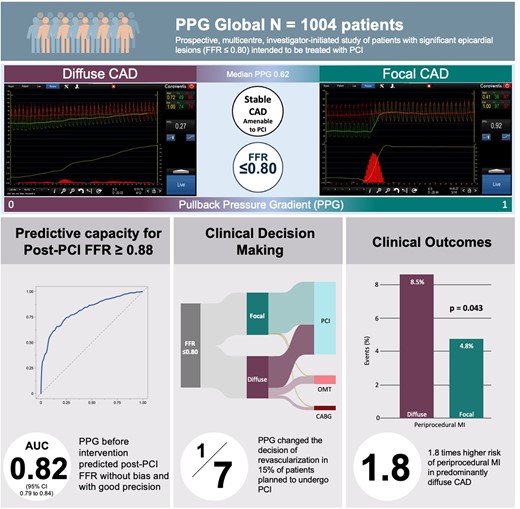
Impaired blood flow after PCI, reflected by low FFR, portends a worse prognosis. Prior to intervention, pressure gradient distributions offer insights into the likelihood of subsequent PCI success. The pullback pressure gradient (PPG) serves as a quantifiable measure of CAD patterns: values approximating 1 signify focal disease, while values approaching 0 suggest diffuse disease. This study aimed to assess the impact of pathophysiological CAD patterns on the safety and efficacy of PCI.
PPG Global was a prospective, investigator-initiated, multicenter study, single-arm that enrolled patients with at least one lesion with an FFR ≤ 0.80 scheduled to be treated by PCI. The study enrolled 1004 patients (1057 vessels). A standardised physiological assessment was performed, including online PPG calculation from manual FFR pullbacks. CAD patterns were defined as predominantly focal or diffuse disease based on the median PPG value. The study was powered to ascertain the predictive capacity of PPG for optimal PCI results (defined as FFR≥0.88 after PCI) as assessed by the AUC. Immediate PCI outcomes were assessed using post-PCI FFR and CFR. Following PCI, biomarkers (troponin) were collected. An independent clinical events committee adjudicated periprocedural myocardial infarction. The assessment of peri-procedural myocardial infarction (MI) adhered to the criteria outlined in the 4th Universal Definition of Myocardial Infarction. Target vessel failure (TVF) was defined as cardiac death, myocardial infarction and target vessel revascularisation.
One thousand and four patients with 1057 vessels were included. The mean FFR was 0.68 ± 0.12, PPG 0.62 ± 0.17, post-PCI FFR 0.87 ± 0.07, and post-PCI CFR was 3.19 ± 1.93. PPG was significantly correlated with the change in FFR after PCI (r=0.65, 95% CI: 0.61-0.69, p<0.001) and showed an area under the curve of 0.82 (95% CI: 0.79-0.84) to predict optimal revascularisation. Suboptimal FFR (<0.88) after an angiographically successful PCI occurred in 471 vessels (53.5%) and was significantly higher in patients with diffuse disease (37.1% vs 74.0%, p<0.001). The change in CFR was sixfold higher in patients with high PPG (delta CFR focal 1.18 ± 1.94 and diffuse 0.19 ± 1.52, p<0.001). The rate of in-hospital TVF was similar between patients with focal vs diffuse disease (5.1% vs 8.5%, p=0.060). The incidence of periprocedural MI was significantly higher in patients with diffuse disease (5.9% vs 9.8%, p=0.050; OR 1.83, 95% CI 1.02 to 3.34).
PPG and Revascularisation Outcomes
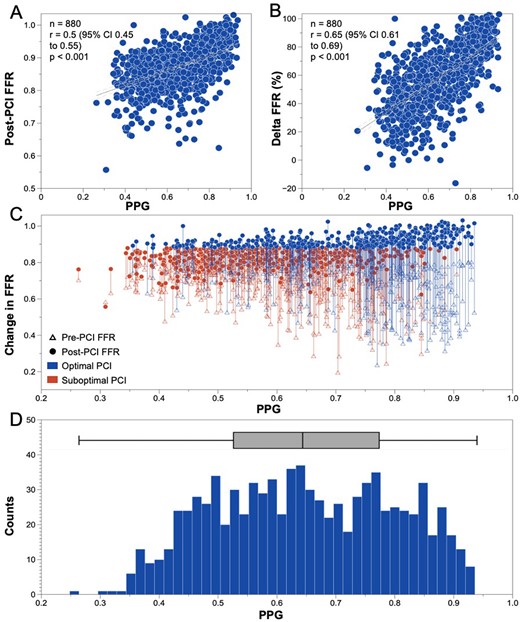
PPG and FFR correlation Pre and Post-PCI
Author notes
Funding Acknowledgements: Type of funding sources: Private grant(s) and/or Sponsorship. Main funding source(s): The study was sponsored by the Cardiovascular Research Institute (CRI) Aalst with an unrestricted grant from Abbott Vascular.



