-
PDF
- Split View
-
Views
-
Cite
Cite
M Sudo, N Murata, M Matsumoto, N Matsumoto, W Atsumi, E Tachibana, H Haruta, T Kougo, K Nomoto, M Arai, K Arima, Y Koyama, K Oiwa, Y Okumura, Clinical implications of hepatorenal function in patients undergoing percutaneous coronary intervention: insights from the SAKURA PCI2 registry, European Heart Journal, Volume 45, Issue Supplement_1, October 2024, ehae666.1301, https://doi.org/10.1093/eurheartj/ehae666.1301
Close - Share Icon Share
Abstract
Hepatorenal function is a prognostic predictor for heart failure, cardiac surgery, and transcatheter intervention for structural heart disease. However, the clinical implications of hepatorenal function assessed by the Model for End-stage Liver Disease eXcluding International normalized ratio (MELD-XI) score is still unclear in patients undergoing percutaneous coronary intervention (PCI).
This study aimed to clarify the association between clinical prognosis and the MELD-XI score.
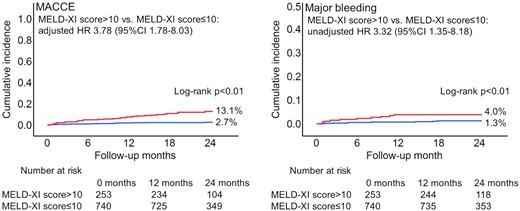
We analyzed 993 patients who underwent PCI from June 2020 to July 2022 in the SAKURA PCI2 registry, a prospective multicenter registry. Patients were stratified into high (>10) or low (≤10) MELD-XI scores. Primary outcome was defined as 2-year major adverse cardio or cerebrovascular event (MACCE), including all-cause death, ischemic stroke, and non-fatal myocardial infarction. Secondary outcome was defined as major bleeding according to the Bleeding Academic Research Consortium 3 or 5.
Of study participating patients, 253 patients (25.5%) were stratified into a high MELD-XI score group and had a higher prevalence of the high bleeding risk than patients with a low MELD-XI score (92.5% vs. 53.7%, p<0.01). Patients with a high MELD-XI score were associated with MACCE (13.1% vs. 2.7%, p<0.01; adjusted HR 3.78, 95%CI 1.78-8.03, p<0.01) and major bleeding (4.0% vs. 1.3%, p<0.01: unadjusted HR 3.32, 95%CI 1.35-8.18, p=0.01). Moreover, these associations remained consistent in patients with chronic and acute coronary syndrome (MACCE, p for interaction=0.89; major bleeding; p for interaction=0.64).
Outcomes
Author notes
Funding Acknowledgements: None.
- acute coronary syndromes
- myocardial infarction
- percutaneous coronary intervention
- cardiac surgery procedures
- hemorrhage
- ischemic stroke
- heart failure
- end stage liver disease
- international normalized ratio
- patient prognosis
- structural disorder of heart
- stratification
- risk of excessive or recurrent bleeding
- primary outcome measure



