-
PDF
- Split View
-
Views
-
Cite
Cite
Maria Grazia Bongiorni, Giulio Zucchelli, Blood stream infection in defibrillator recipients: cardiac imaging for all patients or sometimes skillful neglect?, European Heart Journal, Volume 45, Issue 14, 7 April 2024, Pages 1278–1280, https://doi.org/10.1093/eurheartj/ehae025
Close - Share Icon Share
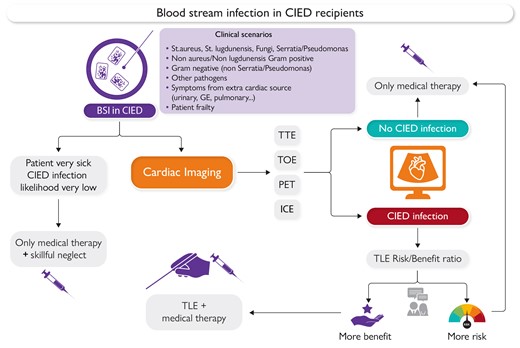
Current management of blood stream infections. BSI, blood stream infection; GE, gastro-enteric; CIED, cardiac implantable electronic device; TTE, trans-thoracic echocardiography; TOE, trans-oesophageal echocardiography; PET, positron emission tomography; ICE, intracardiac echocardiograpy; TLE, transvenous lead extraction
This editorial refers to ‘Cardiac implantable electronic devices and bloodstream infections: management and outcomes’, by T. Özkartal et al., https://doi.org/10.1093/eurheartj/ehae127.
The management of patients with a cardiac implantable electronic device (CIED) during hospitalization for blood stream infection (BSI) can be challenging, and associated outcomes are often poor. In this issue of the European Heart Journal, Özkartal et al. offer new insights into this topic, but they do not entirely resolve the current uncertainty regarding how to properly manage BSI in these specific patients.1 In this retrospective single-centre study, they investigated all consecutive defibrillator recipients implanted over a 10-year period in a specific region of Switzerland. They found that 37 out of 515 patients (7.2%) had been hospitalized with 47 BSI episodes over a median follow-up of 59 months. Most of these patients were treated in non-cardiology units, over half of the BSI episodes were not assessed with cardiac imaging, and only three patients underwent transvenous lead extraction (TLE). Eventually, BSI was associated with a seven-fold higher rate of all-cause mortality at 4 years.
The impact of infection on the outcome of CIED recipients is well established and contributes significantly to public health expenditure, particularly when TLE is not performed or when the intervention is delayed.2,3 Although local infections should not be mistakenly considered benign and have to be promptly treated, systemic infections have a more pronounced effect on major clinical outcomes, especially on mid-term mortality.4,5 Different pathogens, including a high prevalence of Staphylococcus aureus, affecting the CIED in the case of systemic infection, could explain this difference.5 In the case of bacteraemia, an early treatment has a pivotal role, as delayed CIED extraction has been linked to a higher incidence of septic shock, acute kidney injury, respiratory failure, and decompensated heart failure.5 In particular, patients with BSI seem to have a higher incidence of sepsis and multiorgan failure compared with CIED endocarditis with negative cultures.6
For the above-mentioned reasons, the higher mortality in the study of Özkartal et al. reported for BSI infections in ICD recipients is not surprising. However, it cannot be solely attributed to undiagnosed CIED infection and the lack of subsequent device removal. Due to the limited use of advanced cardiac imaging methods, such as trans-oesophageal echocardiography (TOE) and positron emission tomography (PET), CIED infection was not assessable in >60% of patients. In this large slice of the cohort, no definitive conclusions can be drawn about the real cause of death. The multimorbidity of this subgroup may be a significant factor contributing to the poor outcome, considering that chronic kidney disease and a history of myocardial infarction were predictive factors for BSI in this study. The limited use of cardiac imaging in this potentially life-threatening condition might be due to the lack of awareness when patients are hospitalized outside the cardiology ward, the invasiveness of certain exams (TOE), or occasionally the unavailability of specific tests (TOE and PET). It also possible that a deliberate decision to neglect care, the so-called skillful neglect, was applied in some elderly patients with severe frailty.7 In a worldwide survey promoted by the European Heart Rhythm Association (EHRA) on clinical practice and management of CIED infection, the use of TOE ranged between 50% and 83%, with an infrequent PET implementation in the diagnostic work-up. It is important to note that these results are likely to be optimistic and only attainable when a CIED specialist is involved in managing the infection.8
It is essential to recognize that BSI is not a single clinical scenario, and guidelines suggest different management approaches based on culture results when no pocket infection or CIED endocarditis is diagnosed. For instance, confirmed bacteraemia or fungaemia with S. aureus, coagulase-negative staphylococci (CoNS), Cutibacterium spp., or Candida spp. should prompt immediate TLE. In contrast, only Gram-negative (non-Pseudomonas/Serratia) and certain Streptococcus/Enterococcus cases should be treated in the case of recurrence when no other identifiable source is found.9,10
The relatively high rate of infections originating from the urinary tract, with >40% being Gram-negative infections, which notoriously have a low pre-test probability for CIED infection, may explain the conservative approach to diagnosis and therapy in the study of Özkartal et al. However, it is worth considering that the rate of CIED infection may be higher than expected in BSI cases due to non-S. aureus Gram-positive cocci, which should be taken into account when deciding whether or not to perform cardiac imaging (Graphical Abstract).11
What is concerning is that, even in the 16 BSIs (34%) where the authors identified a definite or possible CIED infection, only three patients were referred for TLE. The limited access to TLE for CIED infection is a major issue accounting for the high mortality in this setting. In a recent paper, Sciria et al. reported that only 11.5% of CIEDs with endocarditis were managed with TLE in the USA, with even fewer patients having access to the therapy among females, older people, and those with cognitive or renal impairment.12 Clear data now show that even a delayed TLE procedure is superior to medical therapy alone,13 particularly if a non-powered technique is performed avoiding a femoral approach.14 In the future, the choice of more appropriate devices at implant could significantly influence the outcome of patients at risk of bacteraemia, especially when the pathogens are capable of producing a biofilm. Leadless devices and subcutaneous/extravascular implantations for defibrillators should always be considered in patients at high risk of BSI, such as patients with severe renal failure, or multimorbidity.15 In the study of Özkartal et al., although the implant rate was quite marginal, no BSI infection was diagnosed in S-ICD recipients.
In conclusion, the authors are to be congratulated for their efforts to contribute to our understanding of the current management of patients with suspected CIED infection, shedding light on a significant but underestimated problem. Their work should stimulate the international medical community to seek solutions for improving outcome. An international registry coordinated by the European Society of Cardiology, similar to the Electra registry for TLE, would be desirable to gain a better understanding of the impact of BSI due to cardiac and extra-cardiac sources on the outcomes of CIED recipients.14
Declarations
Disclosure of Interest
All authors declare no disclosure of interest for this contribution.
References
Author notes
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.



