-
PDF
- Split View
-
Views
-
Cite
Cite
Sabine Bleiziffer, Transcatheter vs. surgical treatment of aortc stenosis: long awaited long-term data, yet a long way to go, European Heart Journal, Volume 45, Issue 13, 1 April 2024, Pages 1125–1126, https://doi.org/10.1093/eurheartj/ehad873
Close - Share Icon Share
This editorial refers to ‘Transcatheter or surgical aortic valve implantation: 10-year outcomes of the NOTION trial’, by H.G.H. Thyregod et al., https://doi.org/10.1093/eurheartj/ehae043.
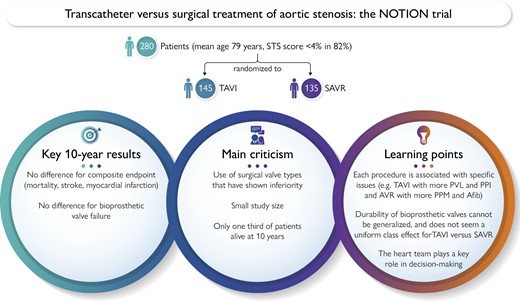
The expansion of indications for transcatheter aortic valve implantation (TAVI), which is now a highly standardized and mature procedure, has led to increased interest in long-term follow-up data. The authors of the NOTION trial,1 published in this issue of the European Heart Journal, are to be congratulated. It is spectacular to finally have 10 years of long-term data comparing surgical and transcatheter treatment of aortic stenosis in a randomized trial that included 280 low-risk patients at a mean age of 79 years. The risk of the composite endpoint of mortality, stroke, and myocardial infarction was 65.5% after TAVI and 65.5% after surgical aortic valve replacement (SAVR; P = .93), with no difference for each individual outcome. The reluctance to offer TAVI to younger, low-risk patients that persists today is based on reference to the lack of long-term data. Can the 10-year NOTION results close this evidence gap?
Some of the major unknowns of TAVI are the durability of the prosthesis and the long-term impact of paravalvular leakage (PVL) and permanent pacemaker implantation (PPI). Criticism of the NOTION trial has focused on the types of prostheses used, particularly surgical valve types such as stented valves with externally mounted pericardium or porcine valves that have shown inferiority in terms of haemodynamics and durability, and the fact that >30% of the surgical prostheses used in the NOTION trial are no longer available today. In fact, 100% of transcatheter prostheses used in the trial are no longer available, as the trial was conducted with an early generation self-expandable transcatheter prosthesis. These issues were addressed by the authors in supplemental analyses that failed to show any significance because of the small size of the subgroups. Pooled data of randomized trials with a self-expandable valve demonstrated an increased structural valve deterioration (SVD) rate of the surgical group after 5 years,2 while different generations of a balloon-expandable valve revealed different results, with no difference from surgery with the latest generation prosthesis type.3 What we can learn from the NOTION study is that durability of bioprosthetic valves cannot be generalized, as different designs and materials of both surgical and transcatheter valves may translate into differences in haemodynamics and durability. It will be of importance for future trials to determine prosthesis type not only in one arm. Bioprosthetic valve deterioration seems not be a uniform class effect of TAVI vs. SAVR. Finally, the NOTION trial did not detect a difference after 10 years between surgery and intervention in terms of durability. Bioprosthetic valve failure according to VARC-3 was 9.7% in the TAVI group and 10.5% in the SAVR group (P = .8). The fact that only a third of the patients in an already small cohort were still alive after 10 years also limits the validity of the results with regard to the long-term durability of the prostheses.
Both moderate/severe PVL rates at any time (25.4% vs. 2.5%, P < .01) and PPI rates (44.7% vs. 14.0%, P < .01) were higher after TAVI in the NOTION study, but the limited sample size of 280 patients prevented demonstration of a potential impact of these parameters on survival in the long term as shown in other studies. On the other hand, the surgical group exhibited a higher rate of atrial fibrillation (52.0% vs. 72.1%, P < .01) or patient–prosthesis mismatch (48.9% vs. 67.8%, P = .0008) after 10 years (Graphical Abstract). Overall, each procedure is associated with some specific issues, but none of these could be associated with survival in this limited sample size. The NOTION trial was not designed to—and is not able to—elucidate or detail these procedure-related risks, the specific impact of which on long-term outcome should inform a decision-making process and patient education.
Being a less invasive procedure, TAVI is considered to lead to a faster recovery, a shorter in-hospital stay, as well as a lower incidence of readmission in the first months after the procedure, all of which may be particularly valuable in older and frail patients. The equivalence or superiority of survival after TAVI in the short term across all risk profiles has recently been challenged by intersecting survival curves at longer follow-up. PARTNER 2A,4 OVSERVANT,5 or GARY6 data show a survival advantage for the surgical arm beyond 2 years. The time-varying effect of TAVI/SAVR on outcomes at 5 years was also discussed in a meta-analysis of seven randomized trials including NOTION data:7 TAVI shows a strong protective effect in the short term that runs out after 1 year. Although not significant, the survival and composite endpoint curves of NOTION also demonstrate a numerical advantage for TAVI within the first 1–2 years and, after that, the curves are superimposed. In accordance with the other previous studies, NOTION shows no survival benefit of TAVI over the long term. This again brings the heart team centre stage because decision-making today and in the future will not rely on survival risk assessment only.
In summary, the NOTION 10-year data confirm current European Guideline recommendations that TAVI in low-risk patients above the age of 75 is indicated and has equal long-term outcomes compared with SAVR. Long-term data on the durability of specific transcatheter and surgical prosthesis types in younger patients are still lacking and will be essential for differentiated decision-making in younger patients. To better understand the significance of certain factors such as PVL or PPI in the long term, we also need more data for differentiated decision-making and to better educate patients.
Declarations
Disclosure of Interest
The author has received speaker fees from Abbott, Boston Scientific, Edwards Lifesciences, and Medtronic.
References
Author notes
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.



