-
PDF
- Split View
-
Views
-
Cite
Cite
Z Xie, B Z Qi, J M Zhou, Ablation for atrial fibrillation improves the outcomes in patients with heart failure with preserved ejection fraction: a single-center cohort study, European Heart Journal, Volume 44, Issue Supplement_2, November 2023, ehad655.737, https://doi.org/10.1093/eurheartj/ehad655.737
Close - Share Icon Share
Abstract
Patients with heart failure and preserved ejection fraction (HFpEF) are frequently associated with atrial fibrillation (AF), and such clinical condition has worse clinical status than those with sinus rhythm. Whether the use of a strategy to maintain sinus rhythm in patients with HFpEF would affect outcomes remains uncertain.
To investigate whether the strategy of AF ablation to maintain sinus rhythm compared to no ablation is associated with improvement of all-cause death and rehospitalization for worsening heart failure in patients with AF and HFpEF.
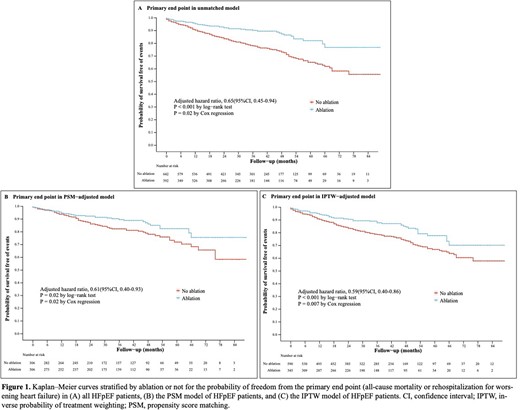
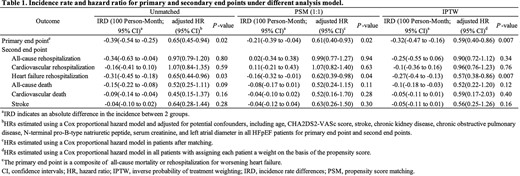
In this retrospective cohort study, a total of 1034 patients with HFpEF and AF (69 [63, 76] years, 478 [46.2%] female) were analyzed, 392 patients who received first-time AF ablation were assigned to the ablation group, and the remaining 642 patients with merely medical therapy were assigned to the no ablation group. The primary end point was a composite of all-cause mortality or rehospitalization for worsening heart failure and was assessed by the Kaplan-Meier method and Cox proportional hazard model. Baseline differences were adjusted by multivariable-adjustment analysis, propensity score-matched analysis, and inverse probability of treatment weighting analysis. Atrial tachycardia/AF recurrence was assessed in a multivariable-adjusted Fine & Gray model, with death treated as a competing risk factor.
After a median follow-up period of 39 months, the cumulative incidence of the primary end point was significantly lower in the ablation group compared to the no ablation group after multivariable adjustment in the overall cohort (adjusted hazard ratio [HR], 0.65 [95% CI, 0.45-0.94], P = 0.02; incidence rate difference [IRD], -0.39 [95% CI, -0.54 to -0.25]). Analyses for secondary outcomes revealed that clinical benefit produced by AF ablation was mainly driven by rehospitalization for worsening heart failure (adjusted HR, 0.65 [95% CI, 0.44-0.96], P = 0.03) with an estimated IRD of -0.31 (95% CI, -0.45 to -0.18). Results were consistent in the propensity score-matched analysis and inverse probability of treatment weighting analysis. In addition, patients in the ablation group had a 34% relative decrease in the atrial tachycardia/AF recurrence (adjusted HR, 0.66 [95% CI, 0.55-0.81], P < 0.001) relative to no ablation group in the multivariate-adjusted Fine & Gray model. Patients who received AF ablation and maintained sinus rhythm during the follow-up period had a lower risk of the primary end point (P < 0.001 by log-rank test).
Author notes
Funding Acknowledgements: Type of funding sources: Public grant(s) – National budget only. Main funding source(s): National key research and development project



