-
PDF
- Split View
-
Views
-
Cite
Cite
J Boeddinghaus, A Sanzone, P Lopez-Ayala, L Koechlin, T Nestelberger, M Rubini Gimenez, K Wildi, D Keller, O Miro, M Christ, C Mueller, Advantageous Predictors of Acute Coronary Syndromes Evaluation (APACE), Prevalence and outcome of clinical misdiagnosis of non-ST-elevation myocardial infarction, European Heart Journal, Volume 44, Issue Supplement_2, November 2023, ehad655.1532, https://doi.org/10.1093/eurheartj/ehad655.1532
Close - Share Icon Share
Abstract
The prevalence of clinical misdiagnosis of non-ST-elevation myocardial infarction (NSTEMI) and its impact on patient outcomes is largely unknown.
We prospectively enrolled adult patients presenting with suspected acute coronary syndromes at 12 sites in five European countries. All patients provided written informed consent and were managed as per local clinical care using conventional, sensitive or high-sensitivity cardiac troponin (hs-cTn) assays. Study blood samples were taken at presentation and serially thereafter for measurements of hs-cTn concentrations. Final diagnoses were adjudicated by two independent cardiologists according to current guidelines and the 4th universal definition of myocardial infarction using all information including serial hs-cTnT measurements and imaging. The primary diagnostic endpoint was the prevalence of clinical NSTEMI misdiagnosis. Co-primary prognostic endpoints were 30 day and two year all-cause and cardiovascular (CV) death.
In 7,678 patients (median age 61 [IQR 48-73], 34% women), the prevalence of adjudicated and clinical NSTEMI was 17.8% and 12.3%, respectively (P<0.001). Among 1,363 patients with an adjudicated NSTEMI (77% type 1 MI, 23% type 2 MI), 470/1,363 (34%) had a clinical NSTEMI misdiagnosis. These patients were older, more often female, had lower median cTn concentrations, and were more likely managed at centers using non-hs-cTn assays at time of enrolment. Compared to patients with an adjudicated and clinical NSTEMI diagnosis, missed patients were less likely to undergo coronary angiography or revascularization and less often discharged on evidence-based treatment (dual antiplatelet therapy 24% vs 79%, statin 64% vs 92%, betablocker 68% vs 81%, all P<0.001). Finally, patients with a clinical NSTEMI misdiagnosis were at much higher risk of premature all-cause (HR 1.51, 95% CI 1.18-1.94, P<0.001) and CV (HR 1.93, 95%CI 1.42-2.63, P<0.001) death.
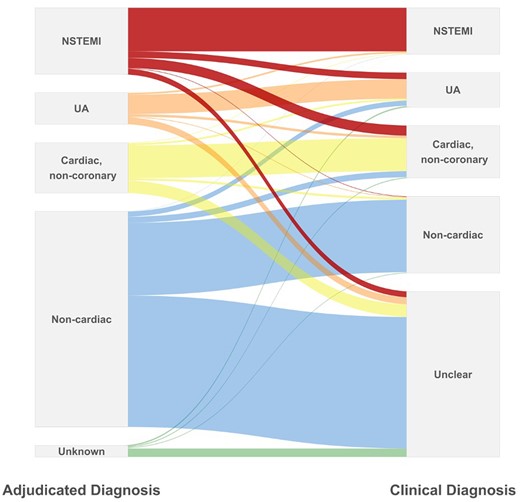
Alluvial plot
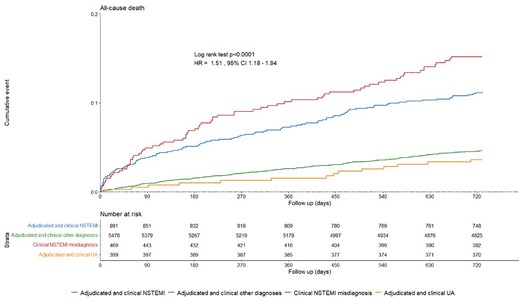
All-cause death at 2-years
- acute coronary syndromes
- myocardial infarction
- non-st elevated myocardial infarction
- coronary angiography
- statins
- cardiologists
- informed consent
- adult
- cardiovascular system
- european continental ancestry group
- diagnosis
- diagnostic imaging
- guidelines
- patient prognosis
- revascularization
- misdiagnosis
- death, premature
- surrogate endpoints
- cardiac troponin measurement
- patient-focused outcomes
- evidence-based treatment
- dual anti-platelet therapy
Author notes
Funding Acknowledgements: Type of funding sources: Foundation. Main funding source(s): Swiss Heart Foundation
Swiss National Science Foundation



