-
PDF
- Split View
-
Views
-
Cite
Cite
Tuğba Kemaloğlu Öz, Luigi Paolo Badano, Can three-dimensional echocardiography change the game for the pulmonary valve?, European Heart Journal, Volume 44, Issue 9, 1 March 2023, Pages 703–705, https://doi.org/10.1093/eurheartj/ehac772
Close - Share Icon Share
Can three-dimensional echocardiography change the game for the pulmonary valve?
‘What we know is a drop, what we don’t know is an ocean.’—Isaac Newton
The pulmonary valve (PV) has an essential role as any other heart valve. However, it has rarely received the attention it deserves. Although the PV is the most anterior valve of the heart, its echocardiographic visualization is more complex than for the other heart valves, and usually, only one or two cusps can be simultaneously imaged by 2D echocardiography (2DE). Pulmonary valve lesion severity should be graded in a similar way to other heart valves using both qualitative and quantitative parameters. Thanks to the technological developments in the field of cardiac imaging and the rapid attack of interventional cardiology, we have had the opportunity to better understand right-sided valves and related right ventricular (RV) remodelling. With the improvement of the resolution of three-dimensional echocardiography (3DE) devices and increased clinical experience, we have started to gain more insight into PV anatomy and pathophysiology.
Why are conventional methods inadequate to evaluate the pulmonary valve?
A comprehensive anatomic and haemodynamic analysis is necessary for the proper assessment of both stenotic and regurgitant PV lesions. Unfortunately, the PV is the heart valve least studied by 2DE among the four heart valves.
Conventional classification of pulmonary stenosis severity is based on trans-pulmonary peak velocity and peak gradient.1 There are some sources of error for gradient and velocity calculations such as misalignment of the Doppler beam, missing the optimal transducer window, and contamination with a different flow. Additionally, the peak transvalvular gradient and peak velocity can be affected by heart rate and changing flow conditions, as it occurs in patients with left-to-right shunt lesions, regurgitation of right heart valves, and RV volume overload. The limitations of 2DE methods can lead to the misclassification of pulmonary stenosis severity.2 When conventional 2DE is used, it is often not possible to acquire the short-axis view of the PV, hampering the proper assessment of valve morphology and the possibility to planimeter the PV’s area.
Although mild pulmonary regurgitation (PR) occurs in almost three of every four patients,3 severe PR is uncommon and usually occurs in patients with pulmonary hypertension, or either anatomical or congenital lesions of the PV. In patients with PR, it is essential to understand the underlying aetiology and determine the severity of regurgitation. Unfortunately, the vast majority of semi-quantitative and quantitative parameters that help us determine the grade of valve regurgitation are not defined for the PV. Moreover, there is no objective reference for the measurement of PR severity.
Incremental value of three-dimensional echocardiography for evaluating pulmonary valve
In patients with good-quality 2DE of the PV, it is possible to acquire transthoracic 3DE data sets of the PV from either the parasternal or the subcostal short-axis views. The difficulty in visualizing the PV is due to its anatomical location in a high anterior plane and its proximity to the left upper lobe of the lung as well as thin PV leaflets which make them less echogenic.
The transoesophageal approach should be considered in PV diseases when the transthoracic acoustic window is insufficient. However, because of the anterior position of the PV in the chest, the transthoracic approach is often superior to the transoesoephageal. Apart from anatomical considerations, the longer-than-expected learning curve supports the fact that operator skill plays a pivotal role in the success of PV imaging.4
Pulmonary valve stenosis is often associated with valve thickening, which increases the 3D echogenicity and image quality. Three-dimensional echocardiography allows accurate and detailed functional and morphological analysis of the entire PV including leaflets, annulus, pulmonary artery and RV outflow tract. Accordingly, it is possible to obtain an enface view of the PV (Figure 1A), planimeter the residual PV area (Figure 1B), assess the leaflet types, and classify stenosis severity with 3DE.5 Measurement of the narrowest PV area (Figure 2, Supplementary material online, Video S1) using direct 3D planimetry overcomes the limitations of the classification based on peak gradient/velocity as it is not affected by volume flow. Three-dimensional echocardiography can be used for quantifying the stenotic subvalvular or subravalvular area by direct planimetry from an optimally oriented perpendicular cut plane obtained by multiplanar reconstruction.5
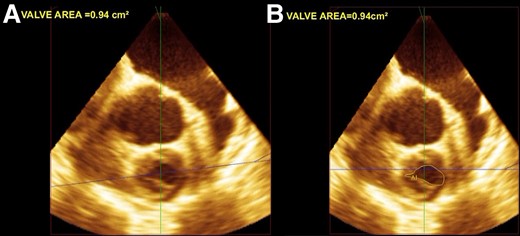
(A) An enface view of the pulmonary valve and (B) the planimetric calculation of the pulmonary valve area.
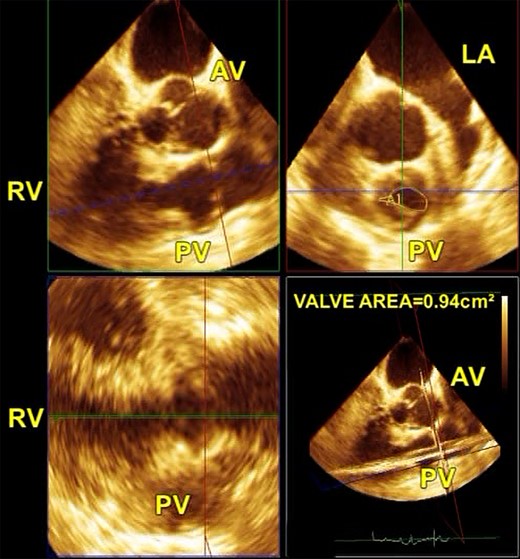
A multiplane reconstruction mode from a 3D full-volume data set to obtain the optimal en face view of the pulmonary valve area for measurement by planimetry. AV, aortic valve; LA, left atrium; PV, pulmonary valve; RV, right ventricle.
In addition, intra- and inter-observer variability of 3D planimetry of both the PV area and the pulmonary artery diameters was found to be excellent.5 However, their accuracy and feasibility mainly depend on the image quality.
There is only one study that assesses the correlation of PR measurement by comparing 3DE to conventional 2DE.6 In this study, 82 adult patients with PR were evaluated, and 3D vena contracta areas (VCAs) were found irregularly shaped in 81 patients. Since 3DE offers multiple views, the 3D jet width was found significantly larger than the 2D jet width. The VCA threshold values of <0.20, 0.21–0.45, 0.46–1.15, and >1.15 cm2 have been defined to classify PR severity from Grades 1 to 4.6
The measurement of VCA using 3D colour Doppler was not optimal because the 3D colour Doppler had lower image quality and frame rate than the 2D colour Doppler. However, technological advancement in newly released devices has overcome pre-existing limitations but the quality of 3DE colour Doppler images is extremely dependent on colour gain settings and the experience of operators.
Conclusion
Three-dimensional echocardiography is a promising new tool for multiplanar and 3D rendering of the PV, and it should be used as a complement to 2DE in PV evaluation. In addition to technological developments, as the interest and experience in PV increases, the planimetric calculation of the PV area and VCA using 3DE may be helpful to overcome the limitations of the conventional 2DE.
Supplementary data
Supplementary data are available in European Heart Journal online.
Funding
All authors declare no funding for this contribution.
Data availability
No new data were generated or analysed in support of this research.
References
Author notes
Conflict of interest: T.K.O.: Global Society of Cardiology, Presidency/Unpaid, Menarini, Honararium, L.P.B.: Italian Ministry of Health, National grant/payment to the institution, Philips Medical System, Research grant and equipment/to the institution, Corcym Sp.A, Echo Core-Lab contract/payment to Institution, Edwards LifeSciences, Clinical Event Committee (personal payment), GE Healthcare, Lectures and courses/personal payment, Philips Medical System, lectures and courses/personal payment, Abbott Sp.A, lectures and courses/personal payment, EsaOte Sp.A, consulting/personal payment.



