-
PDF
- Split View
-
Views
-
Cite
Cite
Chiara Bucciarelli-Ducci, Nina Ajmone-Marsan, The year in cardiovascular medicine 2022: the top 10 papers in cardiovascular imaging, European Heart Journal, Volume 44, Issue 7, 14 February 2023, Pages 554–556, https://doi.org/10.1093/eurheartj/ehac812
Close - Share Icon Share
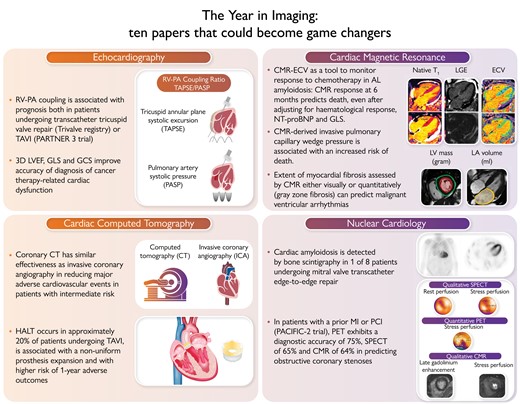
The year in imaging: 10 papers that could become game changers. RV, right ventricle; PA, pulmonary artery; TAVI, transcatheter aortic valve implantation; LVEF, left ventricular ejection fraction; GLS, global longitudinal strain; GCS, global circumferential strain; CT, computed tomography; HALT, hypoattenuating leaflet thickening; CMR, cardiac magnetic resonance; ECV, extracellular volume of distribution; NT-proBNP, Nterminal pro B-type natriuretic peptide; LV, left ventricular; LA, left atrial; MI, myocardial infarction; PCI, percutaneous coronary intervention; SPECT, single photon emission computed tomography.
Echocardiography
The global Trivalve registry tested the use of right ventricle-pulmonary artery (RV-PA) coupling to optimize risk-stratification in 444 patients undergoing transcatheter tricuspid valve repair or replacement (TTVR).1 At the multivariable Cox regression analysis, a TAPSE/PASP ratio < 0.406 was independently associated with an increased risk of all-cause mortality [hazard ratio (HR): 0.57; 95% confidence interval (CI): 0.35–0.93; P = 0.023]. TAPSE and PASP were not correlated, suggesting that RV-PA coupling may depict the cardiopulmonary haemodynamics better than the other two parameters alone, thus improving TTVR patient selection.
Similar results were also observed from 570 patients with severe aortic stenosis (AS) included in the Placement of Aortic Transcatheter Valves Trial (PARTNER) 3 trial.2 Baseline RV-PA uncoupling (TAPSE/PASP ≤ 0.55) was independently associated (with E/E′) with a two-fold increase in the primary composite endpoint at 2 years (all-cause mortality, stroke, rehospitalization). It maintained its prognostic value across multiple subgroups based on the treatment cohort, clinical factors, and echocardiographic parameters.
A recent study in 136 women with human epidermal growth factor 2 (HER2)-positive breast cancer identified a sequential algorithm to diagnose cancer therapy related cardiac dysfunction (CTRCD) [using cardiac magnetic resonance (CMR) as reference] by combining echocardiographic 3D left ventricular ejection fraction (LVEF), global longitudinal strain (GLS), and global circumferential strain (GCS).3 This approach showed to provide a timely diagnosis of CTRCD during routine surveillance with greater accuracy than using the three measures individually or biomarkers and a probability of CTRCD of only 1.0% when results for all three tests were negative.
Cardiac MRI
Chemotherapy is prolonging survival in systemic light-chain amyloidosis, but improved biomarkers of response to treatment are warranted. Changes of extracellular volume fraction (ECV) (novel CMR biomarker) as a response to chemotherapy were evaluated in 176 patients diagnosis, 6, 12, and 24 months after starting chemotherapy.4 CMR regression (≥0.05 decrease in ECV) was observed in 3% at 6 months, in 22% at 1 year, and 38% at 2 years. CMR progression (≥0.05 increase in ECV) was seen in 32% at 6 months, in 22% at 1 year, and 14% at 2 years. CMR response at 6 months predicted death (progression HR 3.82; 95% CI: 1.95–7.49; P < 0.001), even after adjusting for haematological response, N-terminal pro B-type natriuretic peptide (NT-proBNP), and GLS (P < 0.01).
Garg et al.5 challenged this notion that LV filling pressure cannot be estimated by CMR by investigating 835 patients with suspected heart failure. CMR-derived LV mass and left atrial size were associated with invasive pulmonary capillary wedge pressure (PCWP). The CMR-derived PCWP showed moderate correlation with right heart catheterization (HR = 0.55; 95% CI: 0.41–0.66, P < 0.0001), good specificity (92%), and negative predictive value (78%), whilst filling pressure by echocardiography was concordant with invasive PCWP in only 25% of cases. CMR-derived PCWP was prognostic, associated with an increased risk of death (HR = 1.77, P = 0.001), comparable to invasive PCWP (≥ 15 mmHg).
Implantable cardioverter-defibrillators (ICDs) are recommended both in primary and secondary prevention, but improved patients’ selection is warranted. In 700 patients undergoing CMR, visual myocardial fibrosis predicted sudden cardiac death (SCD) (HR: 26.3; 95% CI: 3.7–3337; negative predictive value:100%) but also arrhythmic endpoints (sub-distribution HR: 19.9; 95% CI: 6.4–61.9; negative predictive value:98.6%).6 Quantitative grey zone fibrosis >17 g was associated with highest risk of SCD (HR: 44.6; 95% CI: 6.12–5685) and the arrhythmic endpoint (sub-distribution HR: 30.3; 95% CI: 9.6–95.8). Adding visual and quantitative myocardial fibrosis led to reclassification of 39% patients for SCD and 50% for the arrhythmic endpoint, whilst LVEF was not predictive.
Cardiac computed tomography
Coronary computed tomography (CT) is changing the clinical pathway of patients with chest pain. The diagnostic imaging strategies for patients with stable chest pain and intermediate risk of artery disease trial (DISCHARGE)7 investigated the effectiveness of cardiac CT vs. invasive coronary angiography (ICA) to reduce the frequency of major adverse cardiovascular events in patients with intermediate risk of coronary artery disease. In 3561 patients, the risk of major adverse cardiovascular events was similar in the CT vs. ICA (2.1% vs. 3%) (HR = 0.70; 95% CI: 0.46–1.07; P = 0.10), whilst the frequency of major procedure-related complications was lower with an initial CT vs. ICA strategy (0.5% vs. 1.9%) (HR = 0.26; 95% CI: 0.13–0.55).
Transcatheter aortic valve implantation (TAVI) is a widely used therapy for AS, but there are concerns on the occurrence of hypoattenuating leaflet thickening (HALT) and possible associated risk of reduced long-term prosthesis durability. In 565 patients undergoing cardiac CT for HALT screening at 30 days after TAVI implantation,8 HALT incidence was ∼20% (9% anti-coagulated patients), independently associated with a non-uniform prosthesis expansion (frame deformation, smaller neosinus volume) and also associated with a higher risk of 1-year adverse outcomes.
Nuclear cardiology
Direct comparison of ischaemia testing is scarce. The prospective head to head comparison of coronary CT angiography, myocardial perfusion SPECT, PET and hybrid imaging for diagnosis of ischemic heart disease using fractional flow reserve as index for functional severity of functional stenosis-2 (PACIFIC-2) study9 investigated the diagnostic performance of qualitative 99mTc-tetrofosmin single-photon emission CT (SPECT) vs. quantitative [15O]H2O positron emission tomography (PET) vs. qualitative CMR in patients with a prior myocardial infarction or percutaneous coronary intervention (PCI). When using as reference fractional flow reserve (FFR) ≤ 0.80, SPECT had a sensitivity 67%, specificity 65% vs. PET sensitivity 81%, specificity 65%. CMR's sensitivity was 66% and specificity 62%. PET diagnostic accuracy was 75% (68%–81%), not significantly different than SPECT (65%, 58%–72%, P = 0.03) or CMR (64%, 57%–72%, P = 0.052).
Consecutive patients undergoing transcatheter edge-to-edge repair (TEER) were screened for concomitant cardiac amyloidosis using bone scintigraphy.10 The prevalence of CA was of 1 in 8 (significantly higher than reported in general referral for bone scintigraphy) and associated with disproportionally increased troponin values, thicker LV posterior wall, conduction abnormalities, and carpal tunnel syndrome. Despite CA may pose anatomical challenges, TEER was technically feasible with good magnetic resonance (MR) reduction. However, CA was associated with 2.5-fold higher risk for developing heart failure at mid-term follow-up after TEER.
References
Author notes
Conflict of interest: C.B.-D. is the chief executive officer (part-time) of the Society for Cardiovascular Magnetic Resonance; speaker's fees from Circle Cardiovascular Imaging, Bayer and Siemens Healthineers; she also participated in the medical advisory board of Bayer. N.A.M.: Speaker fees from GE Healthcare, Philips Ultrasound, and Abbott Vascular; research grant from Alnylam, Pie Medical, and Netherlands Hartstichting.



