-
PDF
- Split View
-
Views
-
Cite
Cite
Filippo Crea, Hot topics in congenital heart disease: tetralogy of Fallot, Ross operation, immunodeficiency, cardiac arrest, and end-stage heart failure, European Heart Journal, Volume 44, Issue 34, 7 September 2023, Pages 3201–3204, https://doi.org/10.1093/eurheartj/ehad549
Close - Share Icon Share
 For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
Owing to the great advances in the care for children with congenital heart disease (CHD) by paediatric cardiac surgeons and cardiologists, there are ever increasing numbers of patients with CHD who reach adult life.1–11 This Focus Issue on CHD contains the State of the Art Review article ‘Common diagnostic errors in adults with congenital heart disease’ by David Celermajer from the University of Sydney in Australia, and colleagues.12 The authors note that at some stage during the late teenage years or soon after, children with CHD ‘transition’ from paediatric cardiac care to surveillance by cardiologists who look after adults. Many such specialists, however, are more familiar with commoner acquired heart problems such as coronary disease, heart failure, and arrhythmia in structurally normal hearts and less familiar with CHD. For this reason, international guidelines have suggested that the care of young adults with CHD takes place in designated specialist adult CHD centres. It remains very important, however, for general cardiologists to have a good understanding of many aspects of adult CHD, including common pitfalls to avoid and, importantly, when to refer on to a specialist centre. To help healthcare providers across the spectrum of cardiology practice to address common themes in adult CHD, this state-of-the-art review provides a series of case vignettes to illustrate frequent diagnostic problems that the authors have seen in their tertiary-level adult CHD centres, which are sometimes encountered in general cardiology settings. These include commonly ‘missed’ diagnoses, or errors with diagnosis or management, in these often very complex patients.
Tetralogy of Fallot (TOF) is the most common form of cyanotic CHD, accounting for 3–5 of 10 000 live births. In a Viewpoint article entitled ‘Electrophysiology testing before transcatheter pulmonary valve replacement in patients with repaired tetralogy of Fallot’, Jeremy Moore from UCLA Medical Center in Los Angeles, CA, USA, and colleagues indicate that operative repair of TOF is highly successful, and long-term survival is now expected for most patients.13 An improved ability to detect and treat latent ventricular arrhythmia (VA) substrates in repaired TOF with excellent freedom from recurrence has shifted the weight of evidence towards universal screening before self-expanding transcatheter pulmonary valve replacement (PVR) in the native right ventricular outflow tract (RVOT). The natural history of TOF VA and the well-described electrophysiological substrates that are rendered inaccessible to catheter ablation following PVR are the major drivers for this approach. The authors’ viewpoint is that comprehensive electrophysiological evaluation with potential catheter ablation of pathological ventricular tachycardia substrates should be routinely performed by experienced electrophysiologists before native RVOT transcatheter valve implantation.
In a Meta-analysis article entitled ‘Paediatric aortic valve replacement: a meta-analysis and microsimulation study’, Maximiliaan L. Notenboom from the Erasmus University Medical Centre in Rotterdam, the Netherlands, and colleagues aim to support decision-making in children undergoing aortic valve replacement (AVR) by providing a comprehensive overview of published outcomes after paediatric AVR, and microsimulation-based age-specific estimates of outcome with different valve substitutes.14 A systematic review of published literature reporting clinical outcome after paediatric AVR (mean age <18 years) published between 1 January 1990 and 11 August 2021 was conducted. Publications reporting outcome after paediatric Ross procedure, mechanical AVR (mAVR), homograft AVR (hAVR), and/or bioprosthetic AVR were considered for inclusion. Early risks (<30 days), late event rates (>30 days), and time-to-event data were pooled and entered into a microsimulation model. Sixty-eight studies, of which one was prospective and 67 were retrospective cohort studies, were included, encompassing a total of 5259 patients (median follow-up: 5.9 years). Pooled early mortality for the Ross procedure, mAVR, and hAVR was 3.7, 7.0, and 10.6%, respectively, while the late mortality rate was 5%/year, 1.0%/year, and 1.4%/year, respectively. Microsimulation-based mean life expectancy in the first 20 years was 18.9 years after Ross and 17.0 years after mAVR. Microsimulation-based 20-year risk of aortic valve reintervention was 42.0% after Ross and 17.8% after mAVR (Figure 1).
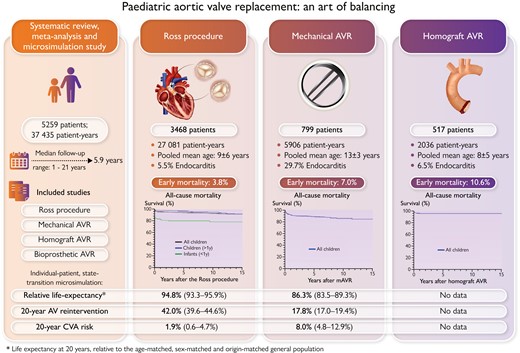
Summary of clinical outcome after paediatric aortic valve replacement (AVR) with a pulmonary autograft (Ross procedure), mechanical prosthesis, or homograft.14
The authors conclude that results of paediatric AVR are currently suboptimal, with substantial mortality especially in the very young, with considerable reintervention hazards for all valve substitutes, but the Ross procedure provides a survival benefit over mAVR. Pros and cons of substitutes should be carefully weighed during paediatric valve selection. The contribution is accompanied by an Editorial by Yves d’Udekem from the Children’s National Medical Center: Children’s National Hospital in Washington, DC, USA, and colleagues.15 They note that there is now no more doubt that the Ross procedure is the best option for AVR in the paediatric population. A strategy of primary repair followed by the Ross procedure at a later age seems to be the only option that appears superior to the primary Ross procedure because it provides a longer longevity of the autograft. There is no doubt that the results of this procedure will improve as we have realized what were the pitfalls of the technique and identified the best way to prevent them. We now have to figure out the best way to train the existing and the future generations of surgeons to the subtleties of this procedure.
In a Clinical Research article entitled ‘Immunodeficiency is prevalent in congenital heart disease and associated with increased risk of emergency admissions and death’, Gerhard-Paul Diller from the Adult Congenital and Valvular Heart Disease University Hospital Muenster in Münster, Germany, and colleagues sought to provide population-based data on the prevalence and clinical significance of immune deficiency syndromes (IDS) associated with CHD.16 Utilizing administrative German Health System data, the prevalence of increased susceptibility to infection (ISI) or confirmed IDS was assessed in CHD patients and compared with an age-matched non-congenital control group. Furthermore, the prognostic significance of IDS was assessed using all-cause mortality and freedom from emergency hospital admission. A total of 54 449 CHD patients were included. Of these, 27% had ISI and 5.6% had a documented IDS (compared with 2.9% of the age-matched general population). During an observation period of ∼400 000 patient-years, 3824 CHD patients died, and 31 017 patients experienced a combined event of all-cause mortality or emergency admission. On multivariable Cox proportional hazard analysis, the presence of ISI [hazard ratio (HR) 2.14, P < .001] or documented IDS (HR 1.77, P = .035) emerged as independent predictors of all-cause mortality. In addition, ISI and confirmed IDS were associated with a significantly higher risk of emergency hospital admission (P = .01 for both on competing risk analysis) during follow-up.
The authors conclude that limited immune competence is common in CHD patients and associated with an increased risk of morbidity and mortality. This highlights the need for structured IDS screening and collaboration with immunology specialists as immunodeficiency may be amenable to specific therapy. Furthermore, studies are required to assess whether IDS patients might benefit from intensified antibiotic shielding or tailored prophylaxis. This manuscript is accompanied by an Editorial by Anselm Uebing and Marc-Phillip Hitz from the University Hospital of Schleswig-Holstein in Kiel, Germany.17 The authors note that immunodeficiency may have a shared genetic underpinning with CHD. Further research on candidate genes for CHD followed by functional genetics may find genes that are implicated in both the modulation of immune response and cardiac morphogenesis. As immune cells are involved in the embryogenesis of the heart, alterations in immune cell function could be partly attributable to both immunodeficiency and cardiac maldevelopment.15 Furthermore, one can speculate that thymectomy, commonly part of neonatal heart surgery, contributes to altered immune function in patients with CHD. To answer these questions, a well-described population of CHD patients is needed with in-depth data on the clinical history, detailed information on the technique of operations, the anatomical and functional phenotype, and ideally access to genome-sequenced patients with biomaterial. Such data can only be provided by large multicentre registries and biobanks, and, fortunately, such registers do exist and are growing.
While out-of-hospital cardiac arrest (OHCA) has been extensively assessed in non-CHD patients,18–21 the risk, characteristics, and outcome of OHCA in patients with CHD remain scarcely investigated. In a Clinical Research article entitled ‘Outcomes of out-of-hospital cardiac arrest in adult congenital heart disease: a Danish nationwide study’, Carlo Alberto Barcella from the Copenhagen University Hospital in Denmark, and colleagues looked into this matter.22 An epidemiological registry-based study was conducted. Using time-dependent Cox regression models fitted with a nested case–control design, HRs with 95% confidence intervals of OHCA of presumed cardiac cause (2001–2019) associated with simple, moderate, and severe CHD were calculated. Moreover, using multiple logistic regression, the authors investigated the association between pre-hospital OHCA characteristics and 30-day survival, and compared 30-day survival in OHCA patients with and without CHD. Any type of CHD was found to be associated with higher rates of OHCA compared with the background population (simple CHD, HR 1.37; moderate CHD, HR 1.64; and severe CHD, HR 4.36). Pre-hospital cardiopulmonary resuscitation and defibrillation were both associated with improved 30-day survival in patients with CHD, regardless of CHD severity. Among patients with OHCA, simple, moderate, and severe CHD had a similar likelihood of 30-day survival compared with no CHD.
Barcella et al. conclude that a higher risk of OHCA is found throughout the spectrum of CHD. Patients with and without CHD showed the same 30-day survival, which relies on the pre-hospital chain of survival, namely cardiopulmonary resuscitation and defibrillation. The contribution is accompanied by an Editorial by Victor Waldmann from the Hôpital Européen Georges Pompidou in Paris, France, and colleagues.23 The authors note that an interesting observation from this study is the significant burden of associated comorbidities in adult CHD patients, in particular cardiovascular risk factors and coronary artery disease. Among CHD patients who presented sudden cardiac death (SCD), 57% had ≥1 cardiovascular risk factor (vs. 57% in non-CHD) and 28% had an ischaemic heart disease (vs. 26% in non-CHD). As the CHD population ages, the importance of considering associated conditions is increasingly recognized. In the SCD context, and because coronary artery disease is the main cause of OHCA in the overall population, ischaemia may be the cause of SCD in a significant proportion of patients, rather than the CHD itself, or could at least be a trigger for ventricular arrhythmias in some defects, with suitable substrate and/or coronary abnormalities resulting in supply–demand mismatch. While screening for and aggressively managing cardiovascular risk factors and co-existing comorbidities appears to impact outcomes favourably in non-CHD populations, comparable data specific to adults with CHD are still lacking and is an area needing further research to understand the relative contribution of different factors.
In a Clinical Research article entitled ‘End-stage heart failure in congenitally corrected transposition of the great arteries: a multicentre study’, Alexandra van Dissel from AMC in Amsterdam, the Netherlands, and colleagues point out that for patients with congenitally corrected transposition of the great arteries (ccTGA), factors associated with progression to end-stage congestive heart failure (CHF) remain largely unclear.24 This multicentre, retrospective cohort study included adults with ccTGA seen at a CHD centre. Clinical data from initial and most recent visits were obtained. The composite primary outcome was mechanical circulatory support (MCS), heart transplantation, or death. From 558 patients (48% female, age at first visit 36 years, median follow-up 8.7 years), the event rate of the primary outcome was 15.4 per 1000 persons-years. Patients experiencing the primary outcome were older and more likely to have a history of atrial arrhythmia. The primary outcome was highest in those with both moderate/severe right ventricular (RV) dysfunction and tricuspid regurgitation (TR), and uncommon in those with mild/less RV dysfunction and TR (P < 0.001). Outcomes were not different based on anatomical complexity, or history of tricuspid valve surgery or of sub-pulmonic obstruction. New CHF admission or VA were associated with the primary outcome. Individuals who underwent childhood surgery had more adverse outcomes than age- and sex-matched controls. Multivariable Cox regression analysis identified older age, prior CHF admission, and severe RV dysfunction as independent predictors for the primary outcome (Figure 2).
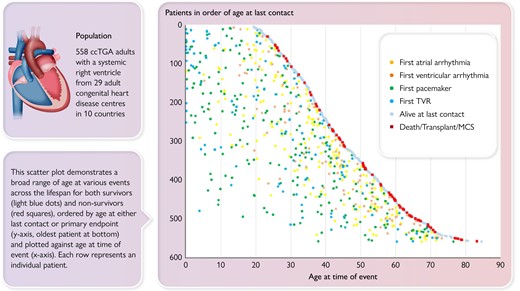
The authors conclude that patients with ccTGA have variable deterioration to end-stage HF or death over time, commonly between their fifth and sixth decade. Predictors include arrhythmic and CHF events and severe RV dysfunction, but not anatomy or need for tricuspid valve surgery. The manuscript is accompanied by an Editorial by Magalie Ladouceur from the Hopital Europeen Georges Pompidou in Paris, France.25 Ladouceur concludes that the future prospects are to use integrated multimodal data to develop a comprehensive decision support system to automate the mapping of clinical trajectories for accurate prediction. This system would enhance risk stratification, identify patients with higher risk of progression, and guide personalized treatment approaches based on individual predicted trajectories.
The issue is also complemented by one Discussion Forum contribution. In a commentary entitled ‘Instrumental variables, in silico trial simulation, and cutting-edge analysis in cardiology: with great power comes great responsibility’ by Brídóg Nic Aodha Bhuí, and John William McEvoy from the University of Galway School of Medicine in Ireland comment on the recent publication ‘Surgical or percutaneous coronary revascularization for heart failure: an in silico model using routinely collected health data to emulate a clinical trial’ by Suraj Pathak from the University of Leicester in the UK.26,27
The editors hope that this issue of the European Heart Journal will be of interest to its readers.
Dr. Crea reports speaker fees from Abbott, Amgen, Astra Zeneca, BMS, Chiesi, Daiichi Sankyo, Menarini outside the submitted work.
With thanks to Amelia Meier-Batschelet, Johanna Huggler, and Martin Meyer for help with compilation of this article.




