-
PDF
- Split View
-
Views
-
Cite
Cite
Antoni Bayes-Genis, Domingo Pascual-Figal, Making STRONGer the transition phase: personalized GDMT through NT-proBNP monitoring, European Heart Journal, Volume 44, Issue 31, 14 August 2023, Pages 2963–2965, https://doi.org/10.1093/eurheartj/ehad356
Close - Share Icon Share
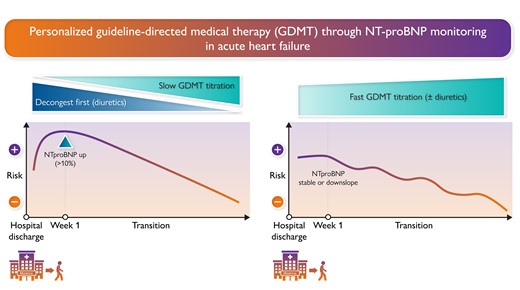
Personalized GDMT through NT-proBNP monitoring. Patients whose NT-proBNP levels are elevated during the first week following discharge (>10%) may benefit from more intensive decongestion before advancing guideline-directed medical therapy (GDMT) up-titration (left). In contrast, patients with stable or decreasing NT-proBNP levels may benefit from early and aggressive up-titration of GDMT (right).
This editorial refers to ‘NT-proBNP and high intensity care for acute heart failure: the STRONG-HF trial’, by M. Adamo et al., https://doi.org/10.1093/eurheartj/ehad335.
‘You never know how STRONG you are, until being STRONG is your only choice’
Bob Marley
Heart failure (HF) is a leading cause of hospitalization, and patients with HF have a high rate of readmission after discharge. This often indicates a gap in care during the transition from hospital to the home environment.1,2 Poor coordination of resources or follow-up after hospitalization can leave HF patients vulnerable to deterioration and rehospitalization. To address this issue, post-hospitalization HF disease management programmes have been developed. These programmes include education, self-management, weight monitoring, dietary advice, exercise recommendations, and medication review.3
Advancing guideline-directed medical therapy (GDMT) during the transition phase after hospital discharge is key to improve outcomes in patients with HF. Very recent studies have evaluated novel approaches to optimize GDMT during this phase. The BETTER-CARE-HF study demonstrated that an automated, patient-specific, electronic health record-embedded alert system improved mineralocorticoid receptor antagonist (MRA) prescribing compared with usual care or a message.4 The IMPLEMENT-HF pilot study found that a virtual, multidisciplinary ‘GDMT Team’ intervention increased GDMT optimization scores and improved HF therapeutic optimization without serious adverse events.5
Despite these promising findings using sophisticated strategies, in-person and personalized care team support has provided the STRONGest evidence for advancing GDMT during the transition phase. Indeed, the STRONG-HF study, a multinational, randomized trial, investigated the optimal dose and pace of up-titration of GDMT for patients with acute HF. The high-intensity care group received up-titrated treatments to 100% of recommended doses within 2 weeks of discharge and close monitoring of clinical status, laboratory values, and N-terminal probrain natriuretic peptide (NT-proBNP) concentrations. Results showed that the intensive treatment strategy reduced symptoms, improved quality of life, and reduced the risk of 180-day all-cause death or HF readmission compared with usual care.6
The STRONG-HF study recommended repeating NT-proBNP measurements at follow-up visits in the high-intensity care group and advised physicians to increase diuretic doses when levels were >10% higher than at pre-discharge. A pre-specified subgroup analysis showed a trend towards greater benefit of high-intensity care in patients with NT-proBNP levels above the median, but with no significant interaction.6 The STRONG-HF investigators carried out a subanalysis which is published in the current issue of the European Heart Journal.7 The main findings of this subanalysis indicate that rapid up-titration of oral HF medications before and after hospital discharge, performed under high-intensity care, is both safe and effective in reducing HF rehospitalization or mortality regardless of baseline NT-proBNP values. The STRONG-HF subanalysis confirms that NT-proBNP levels before discharge are associated with more severe HF and comorbidities such as atrial fibrillation/flutter, as well as poorer outcomes.7 Therefore, clinicians should not hesitate to implement GDMT for patients with a more severe clinical profile, as evidenced by elevated NT-proBNP levels and other indicators of disease risk, during the discharge process. The study also revealed that an early increase in NT-proBNP levels (>10%) 1 week after discharge was associated with a poorer outcome up to 90 days, but not at 180 days, in patients receiving high-intensity care. To address this issue, the investigators devised a personalized approach that involved adjusting the up-titration of GDMT and increasing diuretic dosage based on changes in NT-proBNP levels. With this approach, the benefits of high-intensity care remained consistent, irrespective of early post-discharge fluctuations in NT-proBNP levels7 (Graphical Abstract).
Natriuretic peptides are widely acknowledged as reliable biomarkers for diagnosing HF, and they are incorporated into major HF guidelines. Additionally, natriuretic peptides play a critical role in stratifying patient risk. The initial finding from this substudy, which supports previous research, underscores the significance of NT-proBNP in within-patient risk stratification during the transition phase.
As the medical field moves towards personalized medicine in HF, this study helps to clarify the uncertainty surrounding the use of natriuretic peptide monitoring and its value in guiding a within-individual therapy. Indeed, the usefulness of NT-proBNP in guiding the up-titration and monitoring of GDMT for HF has conflicting evidence. The GUIDE-IT study investigated whether a strategy of NT-proBNP-guided therapy based on a fix threshold (1000 pg/mL) is superior to usual care in improving outcomes in high-risk patients with HF and reduced ejection fraction (HFrEF). The study was stopped for futility with no significant differences observed between the biomarker-guided group and the usual care group in the primary or secondary endpoints.8 The PRIMA II trial, which investigated in-hospital NT-proBNP-guided therapy based on the 30% change threshold, also failed to demonstrate a reduction in readmissions or mortality after discharge.9 The limited availability of GDMT during hospitalization may have hindered its clinical impact. More recently, PIONEER-HF and EMPULSE demonstrated the effectiveness of sacubitril/valsartan and empagliflozin, respectively, in reducing NT-proBNP levels during hospitalization in HF patients. The PIONEER-HF trial showed that sacubitril/valsartan reduced NT-proBNP levels more than enalapril without significant safety concerns.10 The initiation of sacubitril/valsartan during hospitalization resulted in a rapid decrease in NT-proBNP levels, which was statistically significant upon discharge. A sustained and positive response in NT-proBNP reduction over time was associated with better prognosis in TRANSITION.11 In EMPULSE, empagliflozin resulted in an effective and sustained decongestion, lowered the risk of death or HF hospitalization after 90 days, and also decreased NT-proBNP levels in patients hospitalized for acute HF.12,13
The transition phase can be a challenging time for patient care, but also an opportunity to optimize GDMT, which may result in early clinical benefits. During this phase, absolute NT-proBNP values may not be predictive of outcomes, but changes in NT-proBNP levels can provide important independent prognostic information.14 Serial monitoring of NT-proBNP concentrations may aid in optimizing HF management, as changes in NT-proBNP levels can reflect within-patient alterations in various parameters such as ejection fraction, ventricular volumes, filling pressures, and neurohormonal status. Indeed, this subanalysis of the STRONG-HF trial highlights the significance of NT-proBNP level monitoring, particularly in the first weeks after hospital discharge. Patients with increased NT-proBNP levels (>10%) during this period, indicating persistent or worsening myocardial stress and congestion, experienced greater benefits from aggressive decongestion using diuretics followed by gradual uptitration of beta-blockers and renin–angiotensin system (RAS) inhibitors. Ultimately, this stepwise approach resulted in successful decongestion and GDMT up-titration, leading to similarly positive outcomes at 180 days compared with patients without elevation of NT-proBNP levels.
Comparing patients in whom NT-proBNP levels increased by 10% between the intervention and usual care groups could have provided valuable insights into whether recommendations to increase diuretics and slow down GDMT improved prognosis. However, it appears that the study only analysed data from the intervention group in this regard, potentially due to a lack of retrospective NT-proBNP level measurements in the usual care group after discharge.
It should be noted that while natriuretic peptides are commonly used to monitor HF congestion, solely relying on NT-proBNP levels may not provide a complete picture of patient congestion status. Incorporation of lung ultrasound (LUS) or other biomarkers such as CA125 may provide complementary information for a more comprehensive assessment of HF congestion.15
To summarize, it is crucial to ensure that patients with HF receive the best possible medical treatment. Making STRONGer the transition period by monitoring NT-proBNP can give clinicians the confidence they need to titrate GDMT at the appropriate pace for each patient.
Declarations
Disclosure of Interest
A.B.-G. reports personal fees or advisory boards from Abbott, AstraZeneca, Boehringer Ingelheim, Bayer, Novartis, NovoNordisk, Roche Diagnostics, and Vifor Pharma. D.P.-F has no conflicts to declare.
References
Author notes
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.



