-
PDF
- Split View
-
Views
-
Cite
Cite
Fotios Barkas, Kausik K Ray, The global diagnostic network: what can we learn from half a billion lipid measurements between 2018 and 2020?, European Heart Journal, Volume 44, Issue 25, 1 July 2023, Pages 2319–2321, https://doi.org/10.1093/eurheartj/ehad308
Close - Share Icon Share
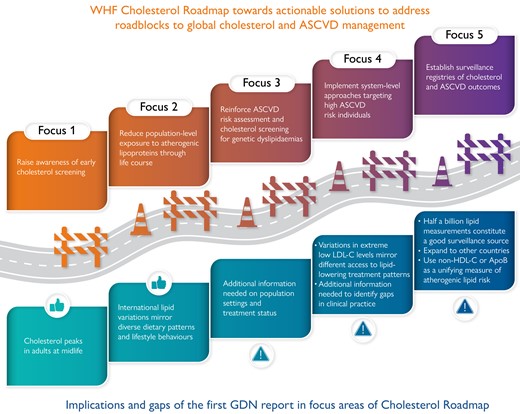
ApoB, apolipoprotein B; ASCVD, atherosclerotic cardiovascular disease; GDN, Global Diagnostic Network; LDL-C, low-density lipoprotein cholesterol; non-HDL-C, non-high density lipoprotein cholesterol; WHF, World Heart Federation.
This editorial refers to ‘Lipid distributions in the Global Diagnostics Network across five continents’, by S.S. Martin et al., https://doi.org/10.1093/eurheartj/ehad371.
The 2022 World Heart Federation (WHF) Cholesterol Roadmap set out an implementation strategy to prevent atherosclerotic cardiovascular disease (ASCVD) through considering cholesterol lowering throughout the life course as a means to reduce ASCVD.1 This means that the measurement of cholesterol is needed as well as the global risk in order to decide what is actionable with respect to reducing lifetime risk.1 FOCUS 5 of that Roadmap was ‘To establish national and regional surveillance of cholesterol and ASCVD outcomes’ (Graphical Abstract).1
With 8 billion people globally living across nearly 200 countries, in this issue of the European Heart Journal, Martin et al. present an interesting study providing contemporary data on lipid distributions in approximately half a billion records from 17 countries across five World Health Organization (WHO) regions.2 This was the first collaborative report of the Global Diagnosis Network (GDN) for individuals aged 20–89 years and tested at GDN laboratories from 2018 to 2020 which have been largely standardized, allowing comparison across countries and over the 3 years to assess time trends.2 Their primary aim was to present the distribution of lipids across different countries so as to guide the implementation of global strategies addressing cholesterol and ASCVD management.2 Despite its size, there are limitations that should be considered that provide context to these data. First, 79% of all measurements came from the USA; Brazil and India were the only low to middle income countries, and relevant data from the African WHO region were not available. Thus, any reference to global lipid variation may be misleading, and the contribution of the present study to the implementation of global health policies to address cholesterol management is therefore somewhat limited. Second, the possibility for repeated measures cannot be excluded as we do not know whether it is the same person or different individuals having the test, whereas individuals lacking access to the healthcare system may not be reflected in this study. The authors also mention that lipid testing was generally community based, but they do not explain why and in whom the test was performed; hence, it is uncertain to what extent these findings could be extrapolated to the national level in the respective countries.
Before outlining the actionable solutions to address cholesterol and ASCVD risk management, the WHF Cholesterol Roadmap underlines the relevance of lipids and lipoproteins to the global ASCVD burden.1 The assessment of total cholesterol alone is uninformative to assess time trends as it masks contradictory trends in HDL cholesterol and non-HDL cholesterol.3 Indeed, countries with a high prevalence of ASCVD, such as Turkey, Saudi Arabia, and India, were among those with the lowest HDL cholesterol levels in the present study, but they were not included among the countries with the highest total cholesterol levels.4 In addition, regions with high prevalence of obesity, type 2 diabetes mellitus, and insulin resistance had low HDL cholesterol and high triglyceride levels, but diverse patterns of total cholesterol levels.5,6 These findings advocate for the use of non-HDL cholesterol or apolipoprotein B as a unifying measure of atherogenic lipid risk in large epidemiological studies, rather than the less useful total cholesterol which is the most readily available measure globally.1
A few points should be considered when interpreting lipid measurements and investigating trends in lipid variations. Variability in the standardization of lipid measurement assays and unknown laboratory coefficients of variation, as well as the method for LDL cholesterol measurement, which in turn will be impacted by fasting status, might account for variations in lipids.1 Although routine analytes with high performance were used in the present study, diverse methods for the calculation of LDL cholesterol were performed.2 Most countries used either beta-quantification, an expensive and usually unavailable method in low to middle income countries which allows accurate measurement of LDL cholesterol, or the Martin–Hopkins formula which allows the estimation of LDL cholesterol from non-fasting lipid profiles.1,7 Nevertheless, seven countries used the Friedwald formula which underestimates LDL cholesterol in non-fasting individuals.1,7 To avoid this limitation, equations allowing estimation of LDL cholesterol from non-fasting samples or non-HDL cholesterol should be universally used in surveillance registries where information on fasting status might not be available.1,7
It should be emphasized that cumulative long-term exposure to cholesterol and other risk factors is what really drives ASCVD development.1 In this regard, the GDN analysis showing a peak in total and LDL cholesterol levels at an adult’s midlife is not novel,8,9 but reinforces the need to improve health literacy and raise awareness about the importance of early cholesterol screening, as explained in FOCUS 1 of the WHF Cholesterol Roadmap (Graphical Abstract).1
As already mentioned, decreased HDL cholesterol and elevated triglyceride levels were noted in countries with a high prevalence of obesity and diabetes in the present study.2 Moreover, high HDL cholesterol and low triglyceride levels were found in Japan and Spain.2 This could be attributed to their similar diet patterns characterized by the increased consumption of fish and plant foods such as rice, vegetables, grains, legumes, and fruit.10,11 Thus lipid variations across different countries may mirror different dietary patterns and lifestyle behaviours, and therefore could guide the implementation of country-specific health policies aiming to reduce population exposure to atherogenic lipoproteins throughout a person’s life span (FOCUS 2, Graphical Abstract).1
The third actionable solution (FOCUS 3) to overcome the roadblocks in cholesterol and ASCVD risk management outlined in the WHF Cholesterol Roadmap is the reinforcement of risk assessment and population screening to reduce underdiagnosis of genetic dyslipidaemias.1 The GDN analysis primarily focused on the proposed WHO risk target of total cholesterol (≥5.00 mmol/L; 193 mg/dL),2 but this refers to untreated healthy individuals.12 Considering the lack of information on the treatment status of the population reported and their concomitant level of cardiovascular risk, Martin et al.’s observation that more than half of the included countries had mean total cholesterol above this threshold is of limited value in terms of global risk evaluation or cholesterol screening (Graphical Abstract).2 The authors also underline the diverse prevalence of LDL cholesterol ≥4.91 mmol/L (190 mg/dL) which ranged from 1% to 10% across the countries included.2 Although such elevated LDL cholesterol levels raise the suspicion for familial hyperchosterolaemia (FH),1 no firm conclusions on FH prevalence can be reached, because diverse population settings (i.e. lipid clinics and tertiary hospitals) and repeat measurements may overestimate the prevalence of LDL cholesterol ≥4.91 mmol/L (190 mg/dL).
Finally, significant differences in the lowest distribution of LDL cholesterol (<1.55 mmol/L; 60 mg/dL) were observed across countries.2 This might mirror different lipid-lowering treatment patterns, namely higher potency statins, combination drugs, and greater availability of more expensive novel lipid-lowering drugs in certain healthcare settings and World Bank regions. Such findings might be relevant to FOCUS 4 of the WHF Cholesterol Roadmap which aims at the implementation of system-levels approaches aiming at robust LDL cholesterol reductions, specifically in individuals at higher ASCVD risk.1 Nevertheless, the lack of information on the setting of cardiovascular prevention, concomitant comorbidities, and lipid-lowering therapies limits the value of these results in identifying the current gaps in clinical practice (Graphical Abstract).
To conclude, the effort of the GDN consortium is to be applauded as it aggregates a huge amount of data from a diverse set of countries across the globe, which in itself is remarkable. This project shows the potential utility of regional surveillance of cholesterol and potentially quality metrics or performance indicators through use of electronic health records. The next step for the authors could be the expansion to other regions and countries, but, more importantly, to see how this resource might be used to improve current practices.
Declarations
Disclosure of Interest
F.B. has received honoraria from Viatris and research grant support from Amgen, Novartis and Novo Nordisk. In addition, he was supported with a grant by the Hellenic Atherosclerosis Society. K.K.R. has received honoraria for consulting, lectures from Kowa, Amgen, Regeneron Pharmaceuticals, Sanofi, Daiichi Sankyo, Pfizer, Viatris, AstraZeneca, Eli Lilly, Esperion, New Amsterdam Pharma, Novartis, Silence Therapeutics, Bayer, Boehringer Ingelheim, Novo Nordisk, SCRIBE, CRISPR, Cargene, Vaxxinity, Abbott, Resverlogix. In addition, he has received research grant support to his institution from Sanofi, Daiichi Sankyo, Amgen, Pfizer and MSD and support from the NIHR Imperial Biomedical Research Centre.
References
Author notes
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.



