-
PDF
- Split View
-
Views
-
Cite
Cite
Filippo Crea, Persistent challenges following percutaneous interventions: paravalvular regurgitation, in-stent restenosis, and antiplatelet treatment-related bleeding, European Heart Journal, Volume 44, Issue 15, 14 April 2023, Pages 1287–1290, https://doi.org/10.1093/eurheartj/ehad212
Close - Share Icon Share
 For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
This Focus Issue on interventional cardiology contains the Special Article ‘Overcoming professional barriers encountered by women in interventional cardiology: an EAPCI statement’ by Gill Louise Buchanan from the North Cumbria Integrated Care NHS Foundation Trust in Carlisle, UK, and colleagues.1 We are witnessing growing interest in sex-related inequalities regarding not only health issues but also leadership in academic institutions and scientific societies.2–9 The authors point out that despite the increasing proportion of female medical and nursing students, there is still a significant under-representation of women working as healthcare providers in interventional cardiology, with very few of them reaching senior leadership, academic positions, or acting principal investigators, as well as very few actively involved in company advisory boards. In this position paper, the authors describe the current status of women working in interventional cardiology across Europe. They also provide an overview of the most relevant determinants of the under-representation of women at each stage of the interventional cardiology career path and offer practical suggestions for overcoming these challenges.
The Issue continues with a second Special Article entitled ‘Renal denervation in the management of hypertension in adults. A clinical consensus statement of the ESC Council on Hypertension and the European Association of Percutaneous Cardiovascular Interventions (EAPCI)’ by Emanuele Barbato from the Sapienza University of Rome, Italy, and colleagues. Optimal treatment of hypertension is a pillar of cardiovascular (CV) prevention.10–12 The authors note that since the publication of the 2018 European Society of Cardiology/European Society of Hypertension (ESC/ESH) Guidelines for the Management of Arterial Hypertension, several high-quality studies, including randomized, sham-controlled trials on catheter-based renal denervation (RDN), have been published, confirming both the blood pressure (BP)-lowering efficacy and safety of radiofrequency and ultrasound RDN in a broad range of patients with hypertension, including resistant hypertension.13 A clinical consensus document by the ESC Council on Hypertension and the European Association of Percutaneous Cardiovascular Interventions (EAPCI) on RDN in the management of hypertension was considered necessary to inform clinical practice. This expert group proposes that RDN is an adjunct treatment option in uncontrolled resistant hypertension, confirmed by ambulatory BP measurements, despite best efforts at lifestyle and pharmacological interventions. RDN may also be used in patients who are unable to tolerate antihypertensive medications in the long term. A shared decision-making process is a key feature and preferably includes a patient who is well informed on the benefits and limitations of the procedure. The decision-making process should take (i) the patient’s global CV risk and/or (ii) the presence of hypertension-mediated organ damage or CV complications into account. Multidisciplinary hypertension teams involving hypertension experts and interventionalists should evaluate the indication and facilitate the RDN procedure. Interventionalists require expertise in renal interventions and specific training in RDN procedures. Centres performing these procedures require the skills and resources to deal with potential complications. Future research is needed to address open questions and investigate the impact of BP lowering by RDN on clinical outcomes and potential clinical indications beyond hypertension.
Transcatheter aortic valve implantation (TAVI) is changing our approach to severe aortic stenosis.14,15 In a Fast Track Clinical Research article entitled ‘Treatment of late paravalvular regurgitation after transcatheter aortic valve implantation: prognostic implications’, Uri Landes from the Tel-Aviv University in Israel, and colleagues investigated the effect of transcatheter interventions to treat paravalvular regurgitation (PVR) after the index TAVI.16 Consecutive patients who underwent transcatheter intervention for ≥ moderate PVR after the index TAVI were enrolled at 22 centres. Principal outcomes were residual aortic regurgitation (AR) and mortality at 1 year after PVR treatment. A total of 201 patients were identified: 43% underwent redo-TAVI, 39% plug closure, and 18% balloon valvuloplasty. Median TAVI-to-re-intervention time was 207 days. The failed valve was self-expanding in 64% of patients. At 30 days, AR ≥ moderate persisted in 17% of patients: 9.9% after redo-TAVI, 26% after plug, and 22% after valvuloplasty (P = 0.036). Overall mortality was similar after redo-TAVI, plug, and valvuloplasty. Regardless of treatment strategy, patients in whom AR was reduced to ≤ mild had lower mortality at 1 year compared with those with AR persisting ≥ moderate (8% vs. 21%; P = 0.007) (Figure 1).
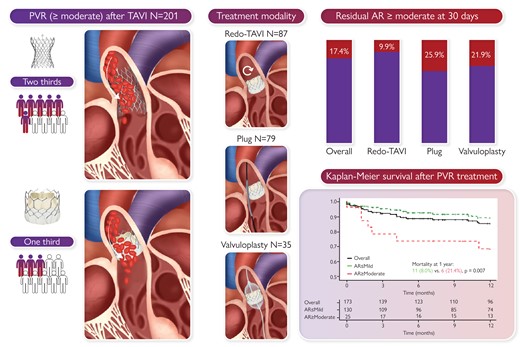
Transcatheter treatment of paravalvular regurgitation (PVR) after transcatheter aortic valve implantation (TAVI) using redo-TAVI, plug closure, or balloon valvuloplasty. Out of 201 patients, the failed valve was self-expanding in two-thirds and balloon-expandable in one-third of the patients. There were 87 patients (43%) who underwent redo-TAVI, 79 (39%) plug closure, and 35 (18%) balloon valvuloplasty. At 30 days, aortic regurgitation (AR) ≥ moderate persisted in 33 (17.4%): 8 (9.9%) after redo-TAVI, 18 (25.9%) after plug closure, and 7 (21.9%) after valvuloplasty (P = 0.036). Regardless of treatment strategy, patients with persistent AR ≥ moderate had higher 1-year mortality compared with those in whom AR was reduced to ≤ mild.16
The authors conclude that their study shows the efficacy of transcatheter treatments for PVR after TAVI. As patients in whom PVR is successfully reduced have better prognosis. The selection of patients and optimal PVR treatment modality require further investigation. The contribution is accompanied by an Editorial by Catherine Otto and Christine Chung from the University of Washington, Seattle, WA, USA.17 Chung and Otto note that one interesting finding from this study is that redo TAVI was often effective at reducing PVR, suggesting that valve undersizing, underexpansion, and/or malpositioning probably contributed to the presence of PVR in these cases. Another striking finding is that two-thirds of the cohort were female, which is not the case for the broader population of patients undergoing TAVI. The observation of a majority female cohort, the majority of whom received a self-expanding valve, proceeding to have moderate or greater PVR, raises the question of whether there is a greater propensity for this unfavourable outcome to occur in smaller annuli.
The best interventional strategy for the treatment of drug-eluting stent (DES) in-stent restenosis (ISR) is still unclear, and no data from randomized trials beyond 3-year follow-up are available.18 In a Clinical Research article entitled ‘Coronary artery restenosis treatment with plain balloon, drug-coated balloon, or drug-eluting stent: 10-year outcomes of the ISAR-DESIRE 3 trial’, Daniele Giacoppo from the Technische Universität München in Germany, and colleagues aimed to define the 10-year comparative efficacy and safety of plain balloon (PB), paclitaxel-coated balloon (PCB), and paclitaxel-eluting stent (PES) for percutaneous coronary intervention (PCI) of DES-ISR.19 Clinical follow-up of patients randomly assigned to PB, PCB, and PES in the ISAR-DESIRE 3 trial was extended to 10 years and events were independently adjudicated. The primary endpoint was a composite of cardiac death, target vessel myocardial infarction, target lesion thrombosis, or target lesion revascularization. Primary results were further assessed by landmark, lesion-level, per-protocol, and competing risk analyses. A total of 402 patients (500 lesions) with DES-ISR were randomly assigned to PB angioplasty, PCB angioplasty, and PES implantation. At 10 years, the primary composite endpoint occurred in 72% assigned to PB, 56% assigned to PCB, and 62% assigned to PES (P < 0.001). The pairwise comparison between PCB and PES resulted in a non-significant difference. At landmark analyses, an excess of death and cardiac death associated with PES compared with PCB was observed within 5 years after PCI, though 10-year differences did not formally reach the threshold of statistical significance after adjustment for multiplicity. Competing risk regression confirmed a non-significant difference in target lesion revascularization between PCB and PES, and showed an increased risk of death associated with PES compared with PCB.
Giacoppo et al. conclude that 10 years after PCI for DES-ISR, the primary and major secondary endpoints between PCB and PES are not significantly different. An excess of death and cardiac death within 5 years associated with PES and the results of the competing risk analysis are challenging to interpret and warrant further analysis. Notably, PES and PCB significantly reduce target lesion revascularization compared with PB. The contribution is accompanied by an Editorial by Alaide Chieffo and Domitilla Gentile from IRCCS San Raffaele Scientific Institute in Milan, Italy, and Mario Iannaccone from the San Giovanni Bosco Hospital in Turin, Italy.2. The authors conclude that the long-term results of the ISAR-DESIRE 3 trial may be considered as a milestone in the treatment of ISR with drug-coated balloons (DCBs), yet further studies are needed to evaluate the role of DCBs in different clinical subsets and lesion anatomies.
Dual antiplatelet therapy (DAPT) with aspirin and a potent P2Y12 inhibitor is the standard treatment for patients with acute coronary syndrome (ACS) undergoing PCI.21,22 In a Clinical Research article entitled ‘Dual antiplatelet therapy de-escalation in acute coronary syndrome: an individual patient meta-analysis’, Jeehoon Kang from the Seoul National University College of Medicine, Republic of Korea, and colleagues point out that de-escalation of the potent P2Y12 inhibtor is an appealing concept to balance the ischaemic and bleeding risks after PCI.23 An individual patient data meta-analysis was performed to compare de-escalation vs. standard DAPT in patients with ACS. Electronic databases, including PubMed, Embase, and the Cochrane database, were searched to identify randomized clinical trials (RCTs) comparing the de-escalation strategy with the standard DAPT after PCI in patients with ACS. Individual patient-level data were collected from the relevant trials. The co-primary endpoints of interest were the ischaemic composite endpoint (a composite of cardiac death, myocardial infarction, and cerebrovascular events) and bleeding endpoint (any bleeding) at 1-year post-PCI. Four RCTs (the TROPICAL-ACS, POPular Genetics, HOST-REDUCE-POLYTECH-ACS, and TALOS-AMI trials) comprising 10 133 patients were analysed. The ischaemic endpoint was significantly lower in patients assigned to the de-escalation strategy than in those assigned to the standard strategy [2.3% vs. 3.0%, hazard ratio (HR) 0.761, log rank P = 0.029]. Bleeding was also significantly lower in the de-escalation strategy group (6.5% vs. 9.1%, HR 0.701, log rank P < 0.001). No significant intergroup differences were observed in terms of all-cause death and major bleeding events. Subgroup analyses revealed that compared with guided de-escalation, unguided de-escalation had a significantly larger impact on bleeding endpoint reduction (P for interaction = 0.007); no intergroup differences were observed for the ischaemic endpoints (Figure 2).
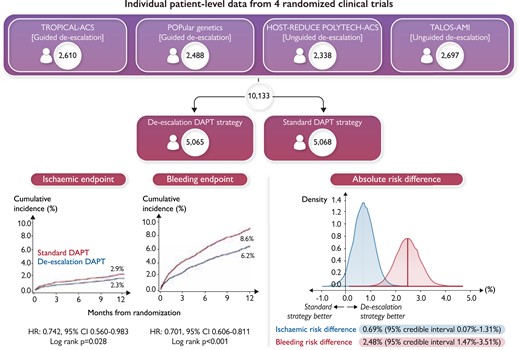
A total of 10 133 patients from four randomized clinical trials were analysed. During the first year after percutaneous coronary intervention, the de-escalation strategy was associated with a lower risk of the ischaemic and bleeding endpoints. The absolute risk difference of endpoints between the two strategies was 0.69% for the ischaemic endpoint and 2.48% for the bleeding endpoint. CI, confidence interval; DAPT, dual antiplatelet therapy; HR, hazard ratio.23
The authors conclude that in this individual patient data meta-analysis, DAPT de-escalation is associated with a decrease in both ischaemic and bleeding endpoints. Reduction in bleeding endpoints is more prominent for the unguided than the guided de-escalation strategy. The manuscript is accompanied by an Editorial by Adnan Kastrati and Gjin Ndrepepa from the Technische Universität München in Germany.24 The authors conclude that antiplatelet de-escalation strategies still remain the subject of intense clinical research. Yet, DAPT de-escalation strategies such as those assessed in the meta-analysis by Kang et al. are poised to offer a valuable option of modulated platelet inhibition in patients with ACS especially in consideration of the lack of specificity of current bleeding risk scores.
The issue is also complemented by two Discussion Forum contributions. In a commentary entitled ‘Prednisone for inflammatory cardiomyopathy: more than just an immunosuppressive agent’, Chao Liu from the Hebei Medical University in China and colleagues comment on the recent publication ‘Immunosuppressive therapy in virus-negative inflammatory cardiomyopathy: 20-year follow-up of the TIMIC trial’ by Andrea Frustaci from the Sapienza University of Rome, Italy, and colleagues.25,26 Frustaci et al. respond in a separate comment.27
The editors hope that this issue of the European Heart Journal will be of interest to its readers.
Dr. Crea reports speaker fees from Abbott, Amgen, Astra Zeneca, BMS, Chiesi, Daiichi Sankyo, Menarini outside the submitted work.
With thanks to Amelia Meier-Batschelet, Johanna Huggler, and Martin Meyer for help with compilation of this article.




