-
PDF
- Split View
-
Views
-
Cite
Cite
L M Lugo Gavidia, D Burger, S Robinson, J Nolde, R Carnagarin, V B Matthews, M P Schlaich, Circulating extracellular vesicles correlate with nocturnal blood pressure and vascular organ damage and may serve as an integrative biomarker of vascular health., European Heart Journal, Volume 43, Issue Supplement_1, February 2022, ehab849.144, https://doi.org/10.1093/eurheartj/ehab849.144
Close - Share Icon Share
Abstract
Type of funding sources: Public Institution(s). Main funding source(s): National Council on Science and Technology, Mexico (CONACYT).
Elevated blood pressure (BP) has been associated with increased levels of circulating extracellular vesicles (EVs) which could potentially serve as a novel integrative biomarker for vascular health.
The present study therefore aimed to assess the relationship between increased EV release, blood pressure and macrovascular organ damage.
A total of 83 patients with BP ranging from normal to high were included in the present analysis. Extracellular vesicles were evaluated by flow cytometry (CD41+/Annexin v+). BP evaluation included unobserved automated office BP (AOBP) and ambulatory BP monitoring (24hr-BP, day-BP and night-BP). Carotid-femoral pulse wave velocity (PWV) was measured by the SphygmoCor XCEL as a marker of macrovascular organ damage.
Hypertensive patients (n = 73, BP 132.9 ± 17.4/79.4 ± 14.0) compared to normotensive patients (n = 10, BP 113.4 ± 10.4/71.3 ± 9.6) had higher levels of EVs (10.6 ± 8.2 vs 6.5 ± 4.5 EV/µL; p = 0.02). Circulating EVs were positively correlated with nocturnal systolic BP (r= 0.3; p = 0.01) and night-time dipping (r= -0.26; p = 0.02) in univariable analysis. In contrast, systolic AOBP, 24hr-BP and day-BP did not show significant associations. No significant correlations were found with diastolic BP. EVs were significantly correlated with PWV (r = 0.26 p = 0.02).While all BP measures were associated with PWV, average systolic night-time BP demonstrated the strongest correlation with PWV (r = 0.55; p < 0.001) compared to systolic AOBP (r = 0.51; p < 0.001), 24hr-BP (r = 0.46; p < 0.001), and average day-BP (r = 0.48; p < 0.001). Multivariable regression models confirmed robustness of the models.
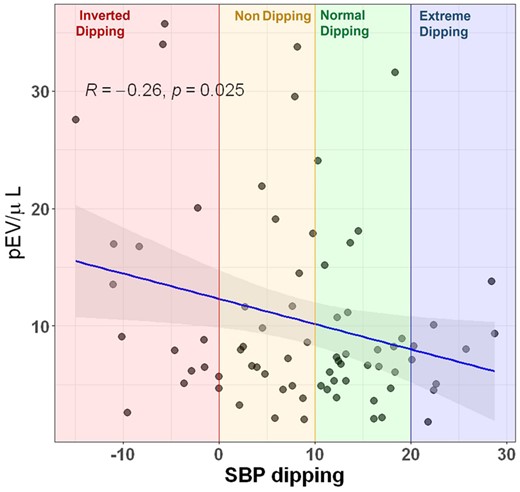
Abstract Figure.
- hypertension
- heart disease risk factors
- systolic blood pressure
- blood pressure
- flow cytometry
- annexins
- biological markers
- ambulatory blood pressure monitoring
- mexico
- multivariate analysis
- systole
- diastolic blood pressure
- cardiovascular event
- night time
- pulse wave velocity
- extracellular vesicles
- carotid-femoral pulse wave velocity



