-
PDF
- Split View
-
Views
-
Cite
Cite
M Ramos, Anticoagulation practices and venous thromboembolism in COVID-19 patients in a Philippine tertiary hospital, European Heart Journal, Volume 43, Issue Supplement_1, February 2022, ehab849.119, https://doi.org/10.1093/eurheartj/ehab849.119
Close - Share Icon Share
Abstract
Type of funding sources: None.
INTRODUCTION
COVID-19 poses an increased risk for thrombosis and initiation of prophylactic anticoagulation has been shown to have mortality benefit in earlier studies. However, the use of full dose anticoagulation as prophylaxis and evidence of the efficacy and safety of anticoagulation on COVID-19 patients remains to be a topic of interest. This study aimed to explore the aspects of anticoagulation applied in a tertiary hospital in the Philippines and to further elucidate on its outcomes and development of complications among COVID-19 patients.
METHODS
In this retrospective, observational study, we collected data from the case record forms of 945 patients with COVID-19 from two tertiary centers. Patients given anticoagulant therapy were classified as treated with standard, intermediate and therapeutic dose anticoagulation. The incidence of mortality and venous thromboembolism (VTE) among the three groups were compared as well as the risk for bleeding complications. Categorical variables were analyzed using the Chi-squared test and logistic regression analysis was done to quantify odds for mortality and complications among the treatment groups.
RESULTS
Among available agents, Enoxaparin was the anticoagulant of choice in 96.1% of cases. The percentage of patients given anticoagulation was noted to increase with increasing severity. Overall, there were 168 (17.8%) inpatient deaths wherein 128 received anticoagulation. 51.3% of those who received therapeutic anticoagulation were intubated at any time during their hospital stay (p value 0.00). In-hospital survival for patients given prophylactic anticoagulation was 78.3% with the highest mortality among patients given therapeutic anticoagulation at 53.8%. Using binary logistic regression, there was increasing odds of mortality as anticoagulant dosage increased with an odds ratio of 2.818 for therapeutic anticoagulation (p = 0.00, b = 1.036). There was significantly lower incidence of pulmonary embolism and among patients given standard prophylactic therapy. The odds of incurring VTE (OR = 3.38, p = 0.001) and PE (OR = 4.315, p = 0.000) were found to increase as dosage increased. Major bleeding after given anticoagulant therapy was recorded in 4.7% of patients. Although half of the patients who presented with bleeding were given standard dose prophylaxis, the incidence of bleeding was highest within the intermediate dose category at 9.2%.
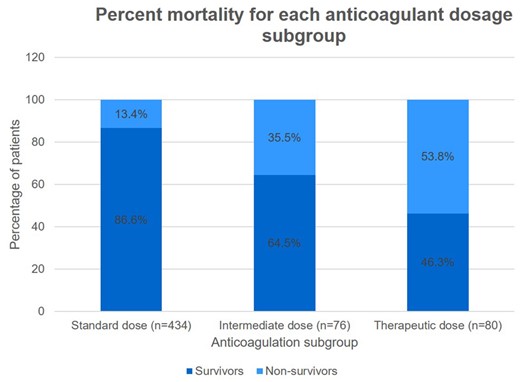
Abstract Figure.
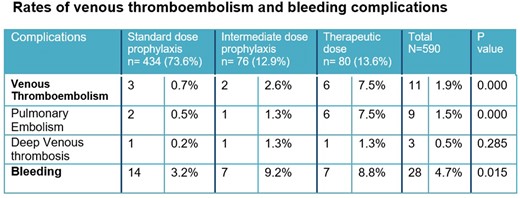
Abstract Figure.



