-
PDF
- Split View
-
Views
-
Cite
Cite
Z A Dakhil, HASAN Farhan, Smokers paradox in non-ST elevation acute coronary syndromes: does it exist?, European Heart Journal, Volume 43, Issue Supplement_1, February 2022, ehab849.089, https://doi.org/10.1093/eurheartj/ehab849.089
Close - Share Icon Share
Abstract
Type of funding sources: None.
In Iraq; about third of males and 4% of females are smokers. There is no data from Middle eastern countries including Iraq on impact of smoking on prognosis in ACS
to assess if there is smokersˈ paradox in patients with NSTE-ACS in terms of lower adverse in-hospital outcomes in smokers
Patients with NSTE-ACS were prospectively included. GRACE score was calculated. Patients were categorised into two groups: smokers vs non-smokers
n.=200, 34.5% were smokers, smokers were younger 53.6 ± 11.2 vs 61.46 ± 11.2, p < 0.001. smokers were males in 89.9% vs 60.3%, p < 0.001 and were hypertensive in 55.1% vs 77.1% p = 0.001. No significant differences between two groups in having DM, IHD, positive family history of IHD nor in troponin positivity. Smokers had higher GFR 91.4 ± 21.9 vs 79.4 ± 22.1, p = 0.001 and higher haemoglobin 13.8 ± 1.9 vs 13.2 ± 2.1, p = 0.04. AF was recorded in 2.9% of smokers vs 11.5%. No statistical difference between groups regarding prescribed drugs including aspirin, P2Y12 inhibitors, B-blockers, ACEI/ARBs, CCB, nitrate, anticoagulant, statin, MRA or diuretic. Smokers were at high GRACE risk class in 21.7% vs 38.2%, p = 0.01, yet, they were catheterized in 76.8% vs 65.6% in non-smokers, p = 0.1. For those who were catheterized, timing to catheterisation did not differ with smoking, p = 0.06. There was no significant difference between the two groups regarding developing in-hospital acute heart failure, ongoing ischaemic chest pain, life-threatening arrhythmias, cardiogenic shock, stroke or death.
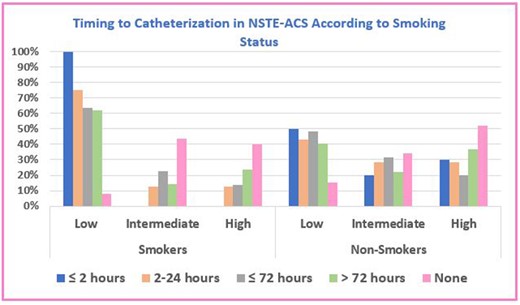
Abstract Figure.
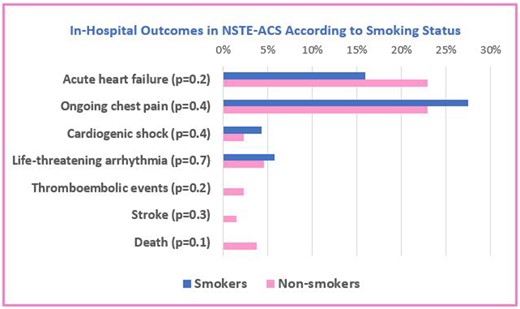
Abstract Figure.
- heart failure, acute
- acute coronary syndromes
- angina pectoris
- angiotensin-converting enzyme inhibitors
- anticoagulants
- cardiac arrhythmia
- aspirin
- nitrate
- smoking
- troponin
- diuretics
- hypertension
- statins
- cardiovascular diseases
- cerebrovascular accident
- ischemic stroke
- angiotensin receptor antagonists
- cardiogenic shock
- smoking cessation
- glomerular filtration rate
- hemoglobin
- catheterization
- comorbidity
- iraq
- mortality
- risk reduction
- non-st-segment acute coronary syndromes
- prevention
- p2y12 receptor antagonists
- smokers
- non-smokers



