-
PDF
- Split View
-
Views
-
Cite
Cite
Cristina Basso, James R Stone, Autopsy in the era of advanced cardiovascular imaging, European Heart Journal, Volume 43, Issue 26, 7 July 2022, Pages 2461–2468, https://doi.org/10.1093/eurheartj/ehac220
Close - Share Icon Share
Abstract
Historically, autopsy contributed to our current knowledge of cardiovascular anatomy, physiology, and pathology. Major advances in the understanding of cardiovascular diseases, including atherosclerosis and coronary artery disease, congenital heart diseases, and cardiomyopathies, were possible through autopsy investigations and clinicopathological correlations. In this review, the importance of performing clinical autopsies in people dying from cardiovascular disease, even in the era of advanced cardiovascular imaging is addressed. Autopsies are most helpful in the setting of sudden unexpected deaths, particularly when advanced cardiovascular imaging has not been performed. In this setting, the autopsy is often the only chance to make the correct diagnosis. In previously symptomatic patients who had undergone advanced cardiovascular imaging, autopsies still play many roles. Post-mortem examinations are important for furthering the understanding of key issues related to the underlying diseases. Autopsy can help to increase the knowledge of the sensitivity and specificity of advanced cardiovascular imaging modalities. Autopsies are particularly important to gain insights into both the natural history of cardiovascular diseases as well as less common presentations and therapeutic complications. Finally, autopsies are a key tool to quickly understand the cardiac pathology of new disorders, as emphasized during the recent coronavirus disease 2019 pandemic.
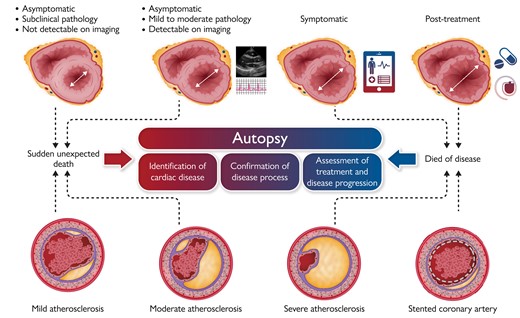
Clinical role of autopsy in patients who die unexpectedly or of known cardiac disease: identification of cardiac disease; confirmation of cardiac disease; and assessment of treatment and disease progression. Top: myocardial disease. Stage 1: Asymptomatic, subclinical (not detectable by current imaging, but detectable at autopsy). Stage 2: Asymptomatic, mildly dilated (detectable by imaging and at autopsy). Stage 3: Symptomatic, dilated (detectable by imaging, confirmed at autopsy). Stage 4: Symptomatic, dilated, post-treatment (assessment of therapy, verification of diagnosis). Bottom: coronary artery disease. Stage 1: Asymptomatic, mild atherosclerosis, complicated by acute thrombosis. Stage 2: Asymptomatic, moderate atherosclerosis, complicated by thrombosis. Stage 3: Symptomatic, severe atherosclerosis. Stage 4: Symptomatic, atherosclerosis post treatment (stent), complicated by thrombosis.
Introduction
There are many benefits from performing clinical autopsies. Autopsies are important for the education of trainees and practitioners. Autopsies also enable identification of new or re-emerging diseases. Autopsies allow for the acquisition of accurate statistics relating to diseases and deaths, and for the surveillance for adverse effects of drugs, devices, and procedures. Thus, they can be invaluable for hospital quality assurance assessments of diagnostic and therapeutic procedures. Furthermore, autopsies allow for the identification of diseases of clinical relevance to the public or relatives, and for the accurate determination of the cause of death in research studies and clinical trials.1–4 Last but not least, autopsies have the ability to improve the completeness and reliability of death certificates, which can impact both families and also public health strategies.
Despite all of the above, the autopsy rate steadily declined in the second half of the last century to fall below 10% in the USA.2,5 As far as Europe is concerned, a 2015 survey of the European Society of Pathology working group of Autopsy Pathology regarding autopsy practice demonstrated a lack of reliable statistics on medical autopsy activity, with no available data from several countries such as France and Germany and very low national rates in other countries such as Spain, Portugal, and Italy, where teaching and non-teaching hospitals were analysed together.6
Many factors may have contributed to this negative trend, such as the elimination of the minimum autopsy rate requirements for accreditation of healthcare organizations. Other factors include an apparent growing lack of clinician awareness about the value of autopsy and the autopsy process itself, the fear of potential legal implications for the treating medical team, and the costs.1–4,7,8 Although the analysis of the various determinants of declining autopsy rates is beyond the scope of this article, we would like to draw attention to the attitude of clinicians and pathologists regarding autopsies.1 Many studies suggest that the decline in hospital autopsy rates is due more to the clinicians’ unwillingness to seek consent for an autopsy than to the relatives’ unwillingness to grant consent. Unwillingness to seek consent for an autopsy can result from a lack of time and clinical pressures, the feeling that the advances in diagnostic imaging and laboratory testing have reduced the value of autopsy, and the assumption that the family is opposed to an autopsy. The attitude of pathologists is equally important, since many pathologists with time commitments in research, teaching, and surgical pathology consider autopsies to be too time-consuming and of little clinical value. The unwillingness of treating clinicians to attend the autopsy or in some instances even discuss the case gives rise to further misconceptions about the clinical value of autopsies. Building a new enthusiasm for autopsy, with an increase in hospital autopsy rates, requires a close interaction between clinicians and pathologists, who should discuss the case before and after the autopsy, possibly having the clinicians attending the autopsy itself. The goal is to provide high quality, pathophysiology-based autopsy reports that are coherent with clinical findings, answering to the clinicians’ questions in a timely manner, rather than a list of abstract anatomical findings. A preliminary report should be distributed soon after the autopsy, and the final report, including microscopic examination, should be finalized in a timely fashion, possibly within 30 days, since delayed reports are less useful for the requesting physicians. When feasible, deaths should be discussed at a multi-disciplinary morbidity and mortality conference where all of the physicians involved in the patient’s care can attend. This approach would improve clinicians’ perception of the value of autopsy.
The authors of this article work at the Medical School Hospital, University of Padua and at the Massachusetts General Hospital, Harvard Medical School, respectively. While Walter Cannon and Richard Cabot inaugurated the clinicopathological conference (CPC) at Harvard Medical School in the early twentieth century, the method of clinicopathological correlation was introduced by Giovanni Battista Morgagni at the University of Padua in the eighteenth century.9,10 The autopsy and CPC are still in use in many academic hospitals, as our own, to teach undergraduate medical students, pathology residents and clinical residents, but also for post-graduate continuing medical education.
Why an article about autopsy and cardiovascular diseases in 2022? There is no doubt that autopsy historically contributed to our current knowledge of cardiovascular anatomy, physiology, and pathology. Major advances in the understanding of cardiovascular diseases, including atherosclerosis and coronary artery disease, congenital heart diseases, and cardiomyopathies, were possible through autopsy investigation and clinicopathological correlations. In this article, we will address some of the reasons to ask for clinical autopsies in people dying from cardiovascular disease (Graphical abstract).
Out-of-hospital death autopsy: the case of sudden cardiac death
Out-of-hospital sudden deaths are typically considered cardiovascular deaths on the death certificates, leading to an overestimation of ischaemic heart disease in the absence of autopsy validation. Post-mortem investigation may represent the first opportunity to make the correct diagnosis, and pathologists are responsible for determining the specific cause and mechanism of sudden death. For this purpose, the Association for European Cardiovascular Pathology has developed guidelines for autopsy investigation which include a detailed protocol for the examination of the heart and recommendations for the selection of histological blocks and appropriate material for toxicology, microbiology, biochemistry, and molecular investigation.11 In sudden cardiac death (SCD), autopsy is an essential step in establishing a diagnosis of inherited cardiac disease and identifying families that require cardiac screening.12 Given the substantial genetic component of SCD in younger people, post-mortem genetic testing may be particularly useful in elucidating etiological factors in the cause of death in this subset. Expert recommendations are available, emphasizing the importance of genetic testing and acquisition of appropriate information regarding the affected individuals, as well as their relatives.13 The recommendations emphasize the importance of increasing the number of autopsies and educating healthcare professionals regarding autopsies. In the setting of potentially inherited conditions, the proband requiring precise phenotyping is the SCD case, and multi-disciplinary collaboration between pathologists, cardiologists, and geneticists is of utmost importance. In such cases, it is important for the autopsy pathologist to freeze blood and/or heart tissue for molecular analyses and to coordinate with treating physicians so that any genetic results can be utilized in the care of living relatives. Moreover, the determination of the cause of SCD at autopsy with the in-depth study of the heart, particularly in young people, may lead to the discovery of new disease entities, as it was for arrhythmogenic right ventricular cardiomyopathy in the 1980s,14 or new variants of already known diseases, such as the non-ischaemic myocardial scar and the arrhythmic mitral valve prolapse syndrome.15,16
In-hospital death autopsy
Post-mortem examination provides the chance for a final consultation before a patient’s file is closed. The statement by Giovanni Battista Morgagni ‘it is impossible to pursue the nature and cause of any disease without dissection of the respective cadavers’17 might sound anachronistic for patients dying in the hospital. However, it is well known that Goldman et al.,18 by examining 100 random autopsies performed in three different eras (i.e. 1960, 1970, and 1980) at a Boston university teaching hospital, found Class 1 errors in about 10% of autopsies in all three decades. Recent studies still show significant unexpected findings at autopsy.19,20 Nowadays, both the duration of hospitalization and the presence of cardiovascular diseases have a significant impact on discrepancies in ante- and post-mortem diagnoses.19 In particular, a short duration of hospitalization before death is one of the most relevant, as a longer stay allows in-depth investigations, thus necessitating autopsy in patients who die in the early days from admission or with limited access to imaging.20
In hospitalized patients with cardiovascular diseases, autopsies are still relevant for furthering our understanding of key issues related to the underlying diseases, despite advancements in cardiac imaging. Autopsies are particularly important for understanding the natural history of cardiovascular disease as well as less common presentations and complications, including those related to medical or interventional therapy.
Autopsy as a reference test for cardiac imaging modalities
Sensitivity and specificity of imaging tests, including echocardiography, computed tomography, cardiac magnetic resonance (CMR), and positron emission tomography, need assessments. Many examples can be made where clinicopathological correlations with advanced imaging modalities provided an insight into the significance of specific imaging findings in various disease entities, such as acute myocardial infarction with reperfusion injury and microvascular obstruction,21 inflammatory diseases,22 and primary and secondary cardiomyopathies23–25 (Figure 1).
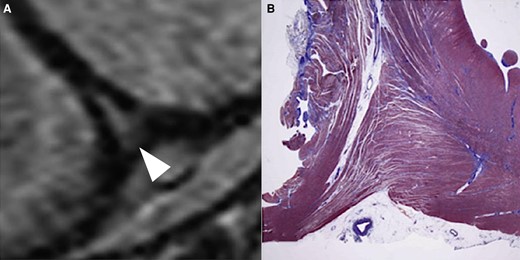
Validation of cardiac imaging findings in dilated cardiomyopathy with pulmonary hypertension. (A) Presence of late gadolinium enhancement in the right ventricular junctional insertion point of the interventricular septum (arrowhead). (B) At autopsy no scar is visible but a marked expansion of the interstitial space due to oedema in the context of disorderly arranged myocytes (modified from De Lazzari et al.24).
One clear example of a disorder where autopsy studies can augment clinical imaging studies is cardiac amyloidosis. In a recent meta-analysis, CMR has been reported to have a sensitivity and specificity for detecting cardiac amyloidosis of around 85–90%.26 However, none of the studies included in the meta-analysis utilized autopsies as the reference test. Thus, the sensitivity and specificity for CMR to detect amyloidosis using a highly sensitive autopsy reference test are largely unknown. Using autopsies to assess the diagnostic accuracy of imaging studies poses additional challenges over using less sensitive but more timely endomyocardial biopsies. However, autopsies can be used as an endpoint in long-term longitudinal studies, particularly in patients with markedly decreased life expectancy such as the elderly, and patients with severe heart failure or metastatic cancer.
In specifically evaluating cardiac transthyretin amyloidosis (ATTR), cardiac scintigraphy, with reagents such as technetium-labelled pyrophosphate, is reported to have a sensitivity of >99% and a specificity of 86%, with false positives largely deriving from the presence of amyloid light chain (AL) amyloidosis.27 However, as with most cardiac imaging modalities, there have not been large autopsy studies confirming these high sensitivities and specificities. Indeed, the studies performed to date demonstrating very high sensitivity and specificity of technetium scintigraphy for ATTR cardiac amyloidosis likely suffer from considerable spectrum bias as subjects were largely selected based on a high likelihood of the presence of ATTR cardiac amyloidosis.28 The phosphate-containing probes used in the scans are clearly not entirely specific for transthyretin and may be binding to microcalcifications in the myocardium, which are more abundant in ATTR compared with AL amyloid deposits.29 Non-amyloid conditions such as myocardial infarcts, hydroxychloroquine toxicity, and hypertrophic cardiomyopathy can also show enhanced uptake of these technetium-labelled phosphate-containing reagents.28–31 Careful studies correlating pre-mortem technetium scintigraphy with autopsy findings would help to clarify the full range of pathological conditions that may yield false-positive scans.
For whole-population incidence of age-related wild-type ATTR (wtATTR) cardiac amyloidosis, autopsy studies are usually utilized.32 At autopsy, ATTR cardiac amyloidosis is typically present in roughly 25% of elderly people aged 85 and older,33 and for most decedents with amyloidosis, the amyloidosis is not diagnosed clinically prior to death. By conventional bone scan, ATTR cardiac amyloidosis is only detected in about 11% of patients aged 85 or older, suggesting the sensitivity of this approach may be closer to 40%.34 More importantly in that study only 3% of the women over age 85 had detectable amyloid on bone scan compared with 23% of women aged 85 or more at autopsy,33 suggesting that routine bone scans have a very low sensitivity for detecting wtATTR cardiac amyloidosis in women. In general, most clinical studies reported a very high male predominance of ∼3:1 for wtATTR,32,34 while pathology-based studies typically showed either no male predominance or a much more subtle male predominance.33 Studies combining cardiac imaging and autopsy could clarify this issue.
Pathologically, amyloid can involve the heart with extensive interstitial deposits and by occlusive vascular deposition involving the small intra-myocardial (penetrating) vessels.35,36 Vascular involvement may occur without extensive interstitial involvement (Figure 2). By obliteration of small vessels, cardiac amyloidosis can lead to an initial presentation mimicking epicardial atherosclerotic coronary artery disease. While imaging studies may have reasonable sensitivity for detecting the extensive interstitial involvement, it is far from clear that current imaging modalities can detect selective occlusive intra-myocardial vascular involvement by amyloid. Autopsy studies can help elucidate such atypical presentations (Figure 3).

Distinct patterns of amyloid deposition in the heart. (A) Congo red stain showing amyloid in a nodular/interstitial pattern (arrows). When extensive, this pattern of amyloidosis is likely identifiable by imaging. (B) Congo red stain showing amyloid in a microvascular specific pattern (arrows). It is unclear if imaging studies can identify this pattern of amyloidosis.
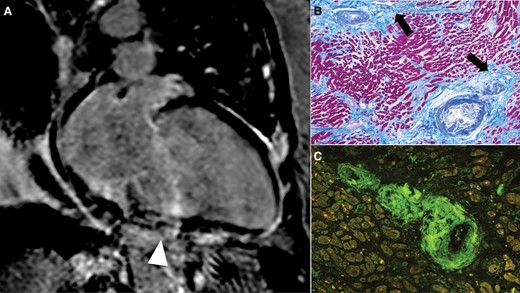
Unexpected histological findings in dilated cardiomyopathy with extensive cardiac imaging investigation during life. (A) Post-contrast cardiac magnetic resonance, two-chamber view: severe left ventricular dilatation and focal late gadolinium enhancement compatible with fibrosis (not coronary-related ischaemic pattern; arrowhead; courtesy of Professor Perazzolo Marra). (B) Histology of the myocardium shows patchy replacement-type fibrosis (arrows) and thickened wall of the small intra-myocardial vessels with lumen subocclusion. (C) Amyloid deposits in the vascular wall are confirmed by Congo red stain by fluorescent microscopy (apple-green birefringence).
Autopsy studies could also be very helpful in understanding the penetrance in hereditary cardiac diseases, such as hereditary forms of ATTR (hATTR) cardiac amyloidosis. While there are over 80 known mutations in the gene encoding transthyretin, the true penetrance for these mutations has largely not been established pathologically. The Val122Ile mutation is one of the more common pro-amyloidogenic mutations, being present in 3.5% of African-Americans.36 Based on echocardiographic wall-thickness measurements, it was suggested that this mutation had a relatively low penetrance of 10–20%.36 However, clinical evaluations have linked this mutation with heart failure with advanced age, suggesting the true penetrance may be much higher.35 For the Phe64Leu form of hATTR, it was recently reported that the penetrance for definitive cardiac involvement based on echocardiography in Italian cohorts was around 47%.37 However, in that study, bone scintigraphy had a sensitivity for detecting cardiac amyloid of only around 10%, using echocardiography as the reference test.37 Well-designed long-term studies involving both pre-mortem cardiac imaging and autopsies in these selected populations could help answer these questions regarding disease penetrance.
Autopsies in the assessment of medical, surgical, and interventional treatment
Autopsy is an important tool of quality assurance in clinical medicine. It serves not only to determine the exact cause of death, but also to unravel unexpected complications of disease processes including adverse or any other either acute or chronic effects of therapy.
After the diagnosis has been made, autopsies can in some settings be very beneficial in assessing the response to treatment. One clear example is in the response of different forms of myocarditis to therapy. Patients with myocarditis may die during treatment and it may be unclear if the death was caused by the damage already done to the heart prior to treatment, or if there was ongoing persistent myocarditis that was resistant to the immunosuppressive regimen. Along this line, it is important to keep in mind that there are multiple forms of myocarditis including lymphocytic myocarditis, giant-cell myocarditis, hypersensitivity myocarditis, and acute necrotizing eosinophilic myocarditis; autopsies can be helpful in clarifying the specific form of myocarditis present. For example, it has recently been shown that high-grade immune checkpoint inhibitor-associated myocarditis can persist at autopsy despite aggressive multi-drug immunosuppressive treatment (Figure 4).38
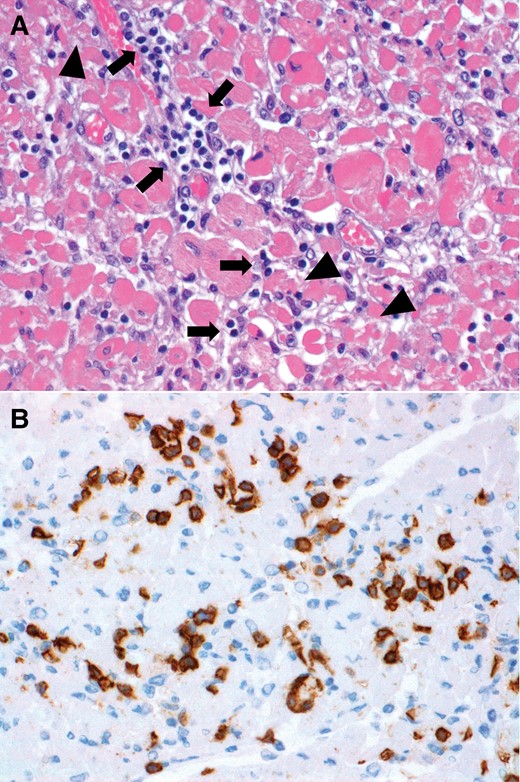
Immune checkpoint inhibitor-associated myocarditis treated with solumedrol and abatacept. Histology of the myocardium at autopsy confirms persistent high-grade myocarditis after treatment. (A) Haematoxylin and eosin-stained section showing infiltration of the myocardium by lymphocytes (arrows) and associated myocyte injury (arrowheads). (B) Immunohistochemical stain for the cytoxic T-cell marker CD8 shows numerous CD8+ lymphocytes.
As far as interventional and surgical therapy is concerned, congenital heart diseases can be used as the paradigm of the contribution of pathologists to the advances in technical procedures, since the observation of the anatomic changes at autopsy in patients either operated or not operated guided surgeons to develop and modify reparative and palliative procedures in the 1960s, 1970s, and 1980s.39–42 The need for the surgeons to see and to touch the hearts led to the development of anatomical collections of hearts with congenital and acquired diseases in many medical centres around the world, such as Saint Paul, Rochester (MN), Washington DC, and Boston in the USA, and London, Amsterdam, and Padua in Europe.
Nowadays, autopsies can still be extremely helpful in elucidating potential acute and chronic complications related to cardiac interventions/surgery, particularly when using novel devices or new technologies. Clinicopathological correlations are essential for quality control in these settings, with information exchange from the cardiology clinic to the pathology laboratory, so that traditional morphological assessment with possible additional biological studies addresses details of the clinical conditions for each device. Analysis of complications detected by autopsy may help to improve the procedures and/or the design of devices by revealing their potential weakness. It is therefore necessary for the pathologists to possess basic knowledge of the most common procedures and available technologies. Because of the large numbers of devices implanted annually in the cardiac surgery and interventional cardiology arena, any examination including autopsy that reveals adverse circumstances and unexpected side effects in the short- and long-term has the potential to have a high impact and supports the need for pathological assessment. The final goal is to improve the quality and longevity of healthcare associated with implanted devices and new therapeutic technologies.
The evolution of percutaneous coronary artery intervention also supports the crucial role of information obtained from human autopsy studies of patients with coronary artery disease to assist clinicians in their daily practice. Remarkable forward steps have been made since the introduction of balloon angioplasty in the 1970s, with the advent of drug-eluting stents (DESs) and a significant reduction of restenosis rates.43 However, new concerns have been raised relating to the long-term safety of DES technology. To address the issue of late in-stent thrombosis, histopathology studies of the vascular response in the stented coronary segments have demonstrated various mechanisms, including a delayed healing with poor re-endothelialization, localized hypersensitivity reaction in sirolimus-eluting stents, strut malapposition in paclitaxel-eluting stents, and neo-atherosclerosis of the in-stent neo-intima. These findings, along with clinical outcomes, have contributed to the development of better devices and new technologies. Moreover, it has been demonstrated that clinical criteria used to classify device complications, such as stent thrombosis, should be validated against an autopsy standard.44
For valvular disease, the experience we had in Padua with the TRI technologies mechanical valve acute failure is an example of how autopsy can save lives. The cardiac surgeon who implanted the prothesis required an autopsy to determine the cause of acute device dysfunction; a pivoting system fracture was found to have caused leaflet detachment from the aortic mechanical valve prosthesis. The post-mortem findings, together with the clinical follow-up of living patients who received the same prosthesis, prompted immediate interruption of the implantation programme, because of the high risk of prosthetic valve structural failure.45
In the era of transcatheter aortic valve implantation (TAVI), a multi-centre autopsy series of patients dying after the procedure showed that in the acute post-implantation time frame, the procedure could be associated with aortic annular rupture and thromboembolic ischaemic stroke.46 In particular, bulky calcification in the left ventricular outflow tract under the left-coronary aortic cusp could be a risk factor for rupture during TAVI47 (Figure 5). Autopsies have also helped to demonstrate that the depth of prosthesis implantation is one of the most important predictors of the need for pacemaker implantation due to conduction disorders soon after transcatheter self-expandable aortic valve implantation.48
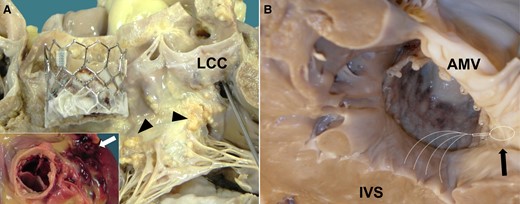
Peri-procedural complications in patients undergoing transcatheter aortic valve implantation. (A) Intra-operative aortic annulus rupture soon after the transcatheter aortic valve implantation procedure with cardiac tamponade (boxed area, external rupture in the pericardial cavity, arrow): in the left ventricular outflow tract region, note the topographic relationship between the bulky calcifications at the level of right and left fibrous trigone (arrowheads) and the rupture at the nadir of the left-coronary cusp (where the probe is passing through; modified from van Tarantini et al.47). (B) Deep implantation of the prosthesis in the left ventricular outflow tract causes compression of subaortic septum, where the specialized conduction system (left bundle branch, white dotted lines) runs superficially with increased incidence of iatrogenic atrioventricular block (arrow indicates atrioventricular node, modified from Fraccaro et al.48). LCC, left-coronary cusp; IVS, interventricular septum; AMV, anterior leaflet of the mitral valve.
Insights from autopsies also shed light on the long-term durability of percutaneous valve prostheses. There is growing concern regarding structural valve deterioration and leaflet thrombosis, which is underdiagnosed in the clinical setting.49 Gaining insight into the mechanisms leading to leaflet thickening is crucial for appropriate clinical management and to develop not only new or modified treatments but also innovations in valve design to prevent structural valve deterioration. The recent finding that there is a time-dependent degeneration in bioprosthetic valves with the primum movens being thrombus formation followed by fibrosis is a clear example of how post-mortem assessment can be of help to improve the long-term durability of percutaneous valve prostheses.50
These data continue to support the role of autopsy in the quickly evolving era of cardiac device technology. Autopsies are well suited to identify uncommon complications of devices. For example, left atrial appendage occlusion devices can be associated with fatal complications including embolization, left atrial appendage wall perforation, pulmonary artery perforation, and cardiac tamponade.51 Autopsies of rare iatrogenic fatalities after pacemaker implantation can reveal anatomic features, such as a paper-thin wall between pectinate muscles in the right atrial appendage, or device-related factors, such as active fixation leads, that increase the risk of wall perforation.52 At the same time, autopsy can reveal the anatomic features favouring a successful catheter ablation and the underlying histological findings.53
Risk scoring systems have been developed in the cardiac surgery and interventional arenas, allowing a reliable comparison of procedural results, but information about patient characteristics and perioperative outcomes is essential. This probably explains why the autopsy rate in the few published reports of post-mortem findings after cardiac/thoracic surgery is significantly higher (24–88%) than that reported for the general in-hospital population. Rastan et al.54 demonstrated a high (23%) overall discrepancy rate between pre-mortem and autopsy diagnoses of the cause of death in a single institution experience with a remarkable autopsy rate (52%). Unknown concomitant diseases, such as unexpected occlusive artery disease, hepatic cirrhosis, and malignant tumours, were invariably found, with potential therapeutic relevance in 19% of cases. Noteworthy, autopsies revealed unrecognized surgery-associated pathological findings in 18% of cases, including coronary artery bypass graft dysfunction, intra-cardiac and prosthetic thrombi, bleeding, tamponade, endocarditis, coronary ostial stenosis after aortic valve replacement, unknown native coronary artery disease, and aortic rupture. The extent of concordance between clinical causes of death and autopsy-proved causes of death depends in part on the underlying causes, with up to 100% concordance for most cerebral, cardiac, and procedure-associated causes and for fatal pulmonary embolism, but only 54% concordance for generalized respiratory distress, 65% concordance for abdominal causes, and 25% for SCD. These data overall emphasize that post-mortem examination in perioperative deaths after cardiac surgery or interventional cardiology procedures must remain a part of our quality assurance programmes.
The value of post-mortem examinations to understand transplant-related diseases, such as infections and tumours, in patients who die after transplantation has been demonstrated since the early stages of transplant medicine in the 1950s to 1970s. Recently, Mund et al.,55 by studying a series of 122 autopsies of transplanted patients including heart transplantation, demonstrated a 5% frequency of malignant tumours identified at autopsy and a 3% prevalence of major discrepancies between the clinical diagnosis and the autopsy findings. Thus, although the rate of missed relevant diagnoses is relatively low, the availability of modern diagnostic techniques does not eliminate the need for autopsies in patients who die after transplantation. Furthermore, the detailed study of transplanted hearts at autopsy can provide insight into the pathophysiology of early and late complications and efficacy of therapies, for acute antibody-medicated and cellular rejection and for cardiac allograft vasculopathy.56,57
Major discrepancy rates between pre-mortem diagnoses and autopsy findings are still reported in critically ill patients in the intensive care unit. Among circulatory support tools, extracorporeal membrane oxygenation (ECMO) is often used in patients affected by severe cardiac failure refractory to inotropic support. Recently, Jia and collaborators58 found major discrepancies between clinical and autopsy diagnoses in patients who underwent ECMO, implying that recognition of clinical signs is challenging in deeply sedated patients. Cardiovascular (mainly myocardial infarction) and neurological (mainly bleeding) events were the most frequent misdiagnoses. In addition to end-stage or acute refractory heart failure, patients requiring ECMO are characterized by severe multi-organ dysfunction and additional side effects/complications related to the artificial device. These ECMO-related complications in part arise from foreign surface/blood contact and cardiac maladaptive changes and include systemic inflammation, haemorrhage, and thrombosis, impaired coagulation, and left ventricular distension. A careful assessment of the impact of ECMO on myocardial integrity is mandatory, taking into account the increasing evidence of unfavourable haemodynamic and metabolic effects on the heart with possible additional myocardial injury. In fact, a constant finding in autopsy series of ECMO patients is the detection of unrecognized myocardial infarction, which may in part be exacerbated by the ECMO itself due to both increased left ventricular afterload and the presence of deoxygenated blood ejected from the left ventricle into the coronary arteries.
Similar considerations should be extended to all percutaneous and surgical ventricular assist devices. Autopsy should remain an important tool in this setting to better understand the complex medical problems, both disease related and device related, and the effects on major organs. In general for in-hospital deaths, autopsies should play a central role in facilitating multi-disciplinary discussions on diagnostic and therapeutic errors through clinical service audits and formal morbidity and mortality conferences.
Autopsy in defining new cardiac diseases
Much of our understanding of cardiac diseases derives from decades of experience during which the pathology of these diseases was elucidated at least in part at autopsy. Autopsies have often given a framework for interpreting imaging findings in the setting of new or potentially new cardiac disorders. This was recently demonstrated during the early phases of the coronavirus disease 2019 (COVID-19) pandemic. Many questions were raised about the significance of elevated serum troponin levels in patients dying from COVID-19, and whether a majority of these patients were experiencing myocarditis. Autopsy studies, besides highlighting the multiplicity of pneumonia phenotypes, including the vascular pattern, allowed us to quickly understand the types of cardiac pathology in these patients.59 Importantly, our multicenter study on COVID-19 patients illustrated how multiple distinct cardiac pathologies were contributing to the elevated serum troponin levels including ischaemic injury, right ventricular strain injury, small vessel thrombi, pericarditis, myocardial macrophage infiltration, and in a minority of patients, actual myocarditis. Autopsies are a key mechanism to quickly understand the cardiac pathology of new disorders.
Now with the COVID-19 pandemic about to enter its third year, we are faced with a new disease that is often referred to as ‘long COVID’ or the post-acute sequelae of severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) infection (PASC). With over a quarter billion cases of SARS-CoV-2 infection worldwide, it has become clear that some of the patients who survive the acute sequelae of the infection continue to experience chronic symptoms afterwards including, in some patients, shortness of breath and chest pain. It is currently unclear what cardiovascular pathological changes may be contributing to these symptoms. In the USA, the National Institutes of Health has launched a large multi-centre study known as Researching COVID to Enhance Recovery (RECOVER) to elucidate the pathophysiology of PASC. One of the three key patient cohorts in the RECOVER study is in fact a multi-centre autopsy cohort, recognizing that autopsies are essential for understanding the pathological processes of new diseases.
Challenges for the continued role of autopsy
While autopsies can play many important and helpful roles in understanding cardiac diseases, the field of autopsy is facing many challenges. In some countries such as the USA, there is little to no governmental funding to support hospital-based autopsies and no requirement that hospitals perform autopsies. Thus, autopsy numbers have been dropping significantly. Some hospitals will not even perform autopsies if the family requests one. Medical examiners primarily perform autopsies in the setting of a suspicion of a non-natural death, and often turn down families requesting autopsies to clarify issues regarding natural deaths. This has lead to a type of post-mortem healthcare access inequality, where families of decedents from relatively more affluent hospitals may be able to obtain an autopsy on their family member, while the families of decedents who were cared for in more economically disadvantaged facilities may not be able to do so.
There has also been an erosion of the teaching of autopsy practice to medical students and pathology residents in many centres.1,60 As a result, medical students can remain poorly educated about the autopsy and there is the risk that some students are arriving at the end of their medical studies without ever having attended one. It is obvious that for them the autopsy will not be a relevant procedure to obtain, if one of their patients dies. Recently the American Board of Medical Examiners reduced the required number of autopsies for US Pathology residents from 50 to 30. In some centres, this is being accompanied by less training in autopsy. If these trends continue, it is likely there will be fewer and fewer pathologists adequately trained to perform detailed hospital-based autopsies. If we are to ensure that the autopsy system is intact and able to accomplish the tasks described above, it is important that we start addressing the erosion in the field through adequate government funding and the essential education of trainees.
We would like to remind what Dr Jesse E. Edwards, a leading cardiovascular pathologist and 1967–68 President of the American Heart Association, wrote in 1999: ‘… Now, persons in the diagnostic fields are being educated and trained in a period not only of declining incidence of autopsy, but, worse than that, absence of the clinician from the few autopsies that are being performed. Unless that trend reverses itself, it is my prediction that the day will come when current and future teachers will miss the fundamental instruction on which the practice of medicine has been built. To overcome the deficiency, there will need to be a return to the autopsy with a promise for future developments in the field of diagnostic testing’.61
Funding
C.B. is supported by the Registry for Cardio-cerebro-vascular pathology, Veneto region, Venice Italy; and CARIPARO Foundation, Padua, Italy.
Conflict of interest: none declared.



