-
PDF
- Split View
-
Views
-
Cite
Cite
Kristian Thygesen, Allan S Jaffe, Revisiting the definition of perioperative myocardial infarction after coronary artery bypass grafting, European Heart Journal, Volume 43, Issue 25, 1 July 2022, Pages 2418–2420, https://doi.org/10.1093/eurheartj/ehac147
Close - Share Icon Share
This editorial refers to ‘Impact of myocardial injury after coronary artery bypass grafting on long-term prognosis’, by L. Pölzl et al., https://doi.org/10.1093/eurheartj/ehac054.
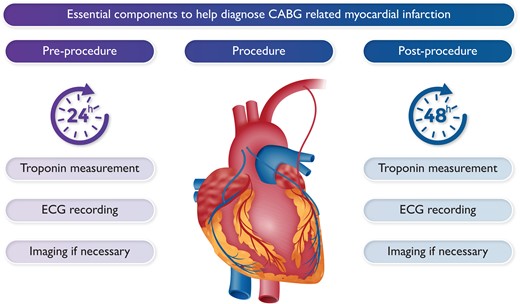
Essential components to help diagnose CABG-related myocardial infarction.
The concept of procedural-related myocardial infarction (MI) was coined in 2000 in the consensus document on the redefinition of MI.1 However, this document, later referred to as the first universal definition of MI (UDMI), dealt only with percutaneous coronary intervention (PCI). The Task Force of the first UDMI was well aware that myocardial injury was unavoidable with cardiac surgery but argued that no biomarker was capable of distinguishing injury due to an acute MI from the myocardial cell injury associated with the procedure itself.1 This is still the case, even though the authors of their articulation in the present issue of the European Heart Journal in their Introduction suggest the myocardial injury intrinsic to the operative procedure is ischaemically mediated.2 It may, or more importantly, may not be.
The matter of the lack of diagnostic criteria for the definition of an MI related to coronary artery bypass grafting (CABG) was eagerly discussed when developing the second UDMI document in 2007.3 It was recognized at this stage that only scant literature existed concerning the diagnostic application of biomarkers for defining MI in the setting of CABG. On the other hand, it had been documented in studies employing cardiac biomarkers in conjunction with CABG that substantial elevations of measured values were associated with a worsened prognosis. This prompted the Task Force to suggest, by arbitrary convention, that the following should be considered as diagnostic of a CABG-related MI (called type 5 MI): (i) biomarker values more than five times the 99th percentile of the upper reference limit following CABG when associated with the appearance of new pathological Q waves or new left bundle branch block; (ii) angiographically documented new graft or native coronary artery occlusion; or (iii) imaging evidence of new loss of viable myocardium.3 However, it was unclear how to distinguish between the injury that was associated with the procedure itself due to cardioplegia and cardiac arrest time, and a vascular event, be it in a native coronary artery or in a bypass graft. Thus, whether in hindsight it was correct to endorse criteria for MI based on the impact of biomarkers on prognosis is unclear. Nonetheless, this concept of capturing MI related to CABG has largely remained unchanged, although with minor modifications of the biomarker cut-off points and of the ancillary criteria through additional iterations of the UDMI documents in 2012 and 2018.4
Initially, the fundamental definitional principles were developed from a diagnostic point of view without regard for prognostic reflections. Even so, there has been an appropriate and increasing interest in examining the outcomes of components of the procedure-related MI definitions with a balanced consideration of diagnostic accuracy and clinical relevance. In this context, cohort analyses have shown substantial differences in the rates and clinical significance of periprocedural MI depending on the criteria applied and the nature of the biomarkers and the assays used to measure them. Various diagnostic cut-offs, with or without ancillary criteria, can provide very different rates of MI after stenting or CABG.5,6
These disputed areas are targeted by Pölzl et al. in this issue of the journal, in which the incidence and prognostic impact of CABG-elated MI was assessed according to the definitions of the 4th UDMI, the Society for Cardiovascular Angiography and Intervention (SCAI), and the Academic Research Consortium (ARC).2 The study showed a significant difference in the occurrence of procedural-related MI (49.5% SCAI vs. 2.9% 4UDMI vs. 2.6% ARC). Furthermore, it showed that the 4UDMI and ARC criteria remained strong independent predictors for all-cause mortality in both the short term (30 days) and the long term (5 years). Both the 4UDMI and ARC definitions augmented the biomarker assessment with ancillary criteria, and this appears to be key to their more robust ability to identify those at risk. In contrast, no significant association was observed between CABG-related MI with the SCAI definition and all-cause mortality.2 It clearly reveals that it does matter how procedure-related MI is defined in a ‘real-life’ setting. It also weakens the elementary significance of the expression ‘clinically relevant MI’ which SCAI has wished to apply equally to CABG and PCI.7
Both cardiac troponins (cTn I and cTnT) and creatine kinase myocardial band (CK-MB) were sampled in the patients. cTn levels were available in 98.1% of patients before surgery and in 99.9% after surgery, whereas CK-MB measurements were available in only 9.8% of patients before surgery and in 95.6% after surgery.2 The sparse measurements of pre-procedural CK-MB might have hampered determination of CABG-related MI according to the SCAI criteria that emphasize baseline measurements but, in the absence of CK-MB determinations, use an increase in cTn concentrations to a very high pre-defined threshold (a 70-fold increase).2 What is important to note and a notable omission was the impact of an increased baseline value on post-procedure values. From prior data with PCI, it appears that an increased cTn baseline value is usually associated with increased post-procedural values probably due to the clinical and anatomical substrate of that subset of patients. That is not the case with CK-MB,8 which, due to its lesser sensitivity and issues of specificity, does not provide that information. In addition, it is no longer endorsed for clinical use.9 These relationships are similar for CABG. There is, for example, a relationship between an increased value of high-sensitivity cTn and the extent and complexity of the underlying coronary artery disease.10 One might wonder whether the increased cTn signal at baseline was due to a possible acute event or the severity of the underlying coronary disease, and might, as with PCI, have presaged the adverse post-CABG effects.
It is noteworthy that the patients in this study were a fairly homogeneous group treated with a standard protocol, i.e. all had on-pump surgery with similar anaesthesia and cardioplegia regimens.2 If a more heterogenous group had been studied, such as those with off-pump surgery or concomitant valve replacement, the results would probably have been different. This is important as it means that these criteria are unique to the procedure studied and the specific assays used to evaluate them.11
It appeared that new occurrence of perioperative ECG changes characteristic for myocardial ischaemia was an important predictive factor.2 Signs of new ischaemia in the ECG including new Q waves and reduced R wave progression within the first 48 h after surgery were observed in 9.9% of the patients and were associated with increases in the rate of events (composite of MI, all-cause mortality, and repeated revascularization) and the rate of death.2 This impact of the ECG has also been shown in other studies.12,13 Was that a function of the likelihood that these patients were those with acute presentations which might be associated with increased baseline concentrations of cTn or individuals with more adverse coronary anatomy as is the case with pre-CABG increases in stable patients?10 Nonetheless, these findings reinforce the clinical applicability of the 4UDMI criteria for CABG-related MI by stressing the development of new pathological Q waves together with cTn release, but also by emphasizing that even an isolated development of new pathological Q waves has important significance.4
The significance of perioperative ECG changes indicative of myocardial ischaemia calls attention to the importance of routinely recording ECGs both before and after coronary surgery. This undertaking not only would be of relevance for the assessment of the prognosis but also would have clinical significance in the event of a new ischaemic pattern that might require rapid action with potential consequences for the outcome.2 Perhaps, in contrast to being a reflection of substrate as suggested above, these findings are indicative of a primary vascular event rather than increased biomarker release due to the procedure itself. That would be of major importance. In fact, higher values of cTn in the past have been correlated with magnetic resonance imaging findings of more extensive confluent and often transmural injury.14 Rather than a biomarker, has the ECG emerged as a key to making this critical distinction? If so, it may permit interventions that will improve prognosis. Time will tell, but it is a clear signal that we should not ignore.
These data help to move the field forward. They provide a critical concept that no biomarker has sufficient sensitivity and, more importantly, sufficient specificity to be used in isolation in the evaluation of patients post-CABG. The data substantiate that the relationship of the definitions to prognosis does matter and that the SCAI definition based on CK-MB and cTn, when CK-MB is not available, is not nearly as useful as the UDMI and the ARC definitions. Of interest, the ECG, especially with the sophisticated processing associated with artificial intelligence, is beginning to re-emerge as a crucial tool.15 Perhaps it is time to re-evaluate and separate the role of biomarkers to derive our definitions and their very different role in helping to define prognosis.
Conflict of interest: K.T. has no conflicts of interest. A.S.J. has consulted or presently consults outside the submitted work for most of the major diagnostic companies, including the companies that make the assays used in this evaluation.
References
Author notes
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.



