-
PDF
- Split View
-
Views
-
Cite
Cite
Yaling Han, Yang Li, Adherence to P2Y12 inhibitors in acute coronary syndrome after a percutaneous coronary intervention: what can we improve?, European Heart Journal, Volume 43, Issue 24, 21 June 2022, Pages 2314–2316, https://doi.org/10.1093/eurheartj/ehac101
Close - Share Icon Share
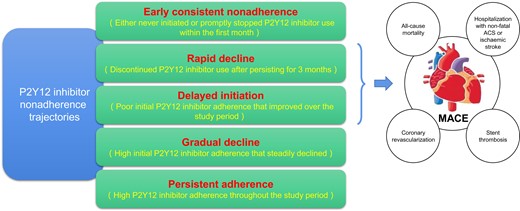
The trajectories of adherence to P2Y12 inhibitors and the association with MACE.
This editorial refers to ‘P2Y12 inhibitor adherence trajectories in patients with acute coronary syndrome undergoing percutaneous coronary intervention: prognostic implications’, by R.D. Turgeon et al., https://doi.org/10.1093/eurheartj/ehac116.
Acute coronary syndrome (ACS), which accounts for nearly half of all deaths due to coronary heart disease, is a major healthcare and economic burden in the world.1 The goals of treatment for patients with ACS focus on symptom relief and preventing complications such as recurrent myocardial infarction (MI) or death.2 Dual antiplatelet therapy (DAPT) with a P2Y12 inhibitor (clopidogrel, prasugrel, or ticagrelor) added to aspirin is considered the standard of care for patients presenting with ACS undergoing percutaneous coronary intervention (PCI). Patients who receive DAPT have demonstrated a reduction in recurrent ischaemic events. Therefore, current guidelines recommend the use of DAPT for 1 year in all patients with ACS, and the PRECISE DAPT score is a tool to support decision-making in deciding the duration of DAPT.3–5
Importantly, medication adherence to DAPT after PCI is important to optimize clinical outcomes. Premature DAPT cessation is associated with an increased risk for stent thrombosis, MI, or even death. The prospective, international, multicentre PARIS (Patterns of Non-Adherence to Anti-Platelet Regimens In Stented Patients) registry suggested that the reason for DAPT cessation influences the risk for major adverse cardiovascular events (MACE), with those stopping therapy due to ‘disruption’ (non-adherence or bleeding) having the highest risk [hazard ratio (HR) 1.50, 95% confidence interval (CI) 1.14–1.97), whereas those discontinuing (physician-guided) have a lower risk (HR 0.63, 95% CI 0.46–0.86).6 In this registry, DAPT cessation was more frequent in elderly and high bleeding risk patients.7,8 Additionally, the OPT-CAD (Optimal antiPlatelet Therapy for Chinese patients with Coronary Artery Disease) registry which enrolled 14 032 consecutive patients (including 7049 patients with ACS undergoing PCI) was designed to develop a predictive model and guide the management for antiplatelet therapy.9 Rates of DAPT adherence were 85.3, 76.6, 73.4, 71.0, and 55.6% at discharge, 3, 6, 9, and 12 months, respectively. Consequently, premature DAPT discontinuation before 12 months was associated with increased risk of ischaemic events.10,11 A meta-analysis of 34 studies with description of DAPT adherence and 11 studies with description of factors associated with non-adherence demonstrated that rates of DAPT adherence after drug-eluting stent (DES) placement are generally high (85.6–98.3%) at 1 month, begin to decline (70.3–98.8%) by 6 months, and are lower (42.8–96.2%) at 12 months.12 Furthermore, factors associated with non-adherence included bleeding, lower education level, immigrant status, and lack of knowledge regarding DAPT.12
In this issue of the European Heart Journal, Ricky D. Turgeon et al.13 report the results of a population-based cohort study of all patients older than 18 years of age in the province of Alberta, Canada who underwent PCI for ACS from 1 April 2012 to 31 March 2016. Prevalent P2Y12 inhibitor users (defined as individuals with a prescription for clopidogrel, prasugrel, or ticagrelor within 120 days prior to the index ACS admission), patients whose first P2Y12 inhibitor fill was for prasugrel (due to the limited use of this agent during the study time frame), and patients who died during index ACS hospitalization or on the date of discharge were excluded. The aim of the study was to evaluate P2Y12 inhibitor adherence trajectories among ACS patients treated with PCI, their frequency, and association with 12-month MACE defined based on a composite of all-cause mortality, hospitalization with non-fatal ACS or ischaemic stroke, coronary revascularization excluding staged PCI procedures, and stent thrombosis. Group-based trajectory modelling (GBTM) to identify adherence trajectories to P2Y12 inhibitors was firstly used in the research field of antiplatelet therapy.13 Although GBTM does not solve the problem of balancing comprehensibility and complexity, it is a method used to identify latent groups of individuals following a similar longitudinal trajectory, and subsequently allows for the evaluation of the frequency of each trajectory group, as well as associations with risk factors and subsequent outcomes.14 A total of 12 844 patients were included in this study. The mean age was 62.4 years, 24.6% were female, 45.6% presented with ST-segment elevation MI (STEMI), and 62.1% were treated with a second-generation DES.
The present study identified five distinct trajectories of P2Y12 inhibitor adherence in the year after undergoing PCI for ACS: 1414 (11.0%) patients either never initiated or promptly stopped P2Y12 inhibitor use within the first month (early consistent non-adherence), 983 (7.7%) discontinued P2Y12 inhibitor use after persisting for 3 months (rapid decline), 768 (6.0%) had poor initial P2Y12 inhibitor adherence that improved over the study period (delayed initiation), 2535 (20.5%) had high initial P2Y12 inhibitor adherence that steadily declined (gradual decline), and 7144 (54.8%) had high P2Y12 inhibitor adherence throughout the study period (persistent adherence). The five trajectories identified in this analysis provide an intuitive, clinically meaningful classification of P2Y12 inhibitor adherence trajectories that are consistent with a conceptual framework. Moreover, classifying patient adherence based on their trajectory may facilitate the implementation of targeted adherence interventions. Overall, the authors found that more than half (54.8%) of this cohort had persistent adherence to their P2Y12 inhibitor, whereas the remaining patients had one of four distinct suboptimal adherence trajectories. These same five trajectories emerged in both males and females, with similar distribution across groups. Several factors, such as worse socioeconomic status, smoking, prior PCI, stent type, and lower concomitant use of other preventive medications were associated with non-adherence and shared across two or more non-adherence trajectories. In addition, compared with persistent adherence, rapid decline (HR 1.23, 95% CI 1.01–1.49) and delayed initiation (HR 1.41, 95% CI 1.12–1.78) were both associated with a higher risk of MACE, whereas early consistent non-adherence was significantly associated with MACE in the DES subgroup (Graphical Abstract). A gradual decline in adherence was not associated with significantly higher risk of MACE. The post-hoc sensitivity analysis showed that early consistent non-adherence (HR 1.50, 95% CI 1.12–2.02) and rapid decline (HR 1.40, 95% CI 1.09–1.79) were associated with a higher risk of major bleeding compared with persistent adherence, particularly during the period of relatively higher adherence, whereas delayed initiation and gradual decline were not associated with increased major bleeding. Interestingly, patients in the rapid decline group may have both high bleeding and high ischaemic risk, who discontinued P2Y12 inhibitors because of bleeding and consequently were associated with higher MACE after P2Y12 non-adherence.
These data published in the article will be helpful to evaluate the trajectories of adherence to P2Y12 inhibitors among patients with ACS treated with PCI and the association with MACE,13 but the lack of detailed information on patients (high bleeding risk, high ischaemic risk, or both high bleeding and high ischaemic risk), the individualized time of P2Y12 inhibitor discontinuation, the causal relationship between bleeding and non-adherence, as well as types of P2Y12 inhibitors and DES, still call for additional large-scale registries specifically examining these points. Performing similar studies in different geographic areas may also be useful to evaluate the impact of socioeconomic factors on P2Y12 inhibitor adherence trajectories. Despite these unknowns, the present study represents a valuable contribution to the identification of five distinct trajectories of P2Y12 inhibitor adherence, risk factors for P2Y12 inhibitor non-adherence trajectories, and the association of P2Y12 inhibitor trajectory with MACE and major bleeding.
Conflict of interest: none declared.
References
Author notes
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.



