-
PDF
- Split View
-
Views
-
Cite
Cite
Filippo Crea, Percutaneous coronary intervention vs. coronary artery bypass graft: the saga continues, European Heart Journal, Volume 43, Issue 13, 1 April 2022, Pages 1273–1276, https://doi.org/10.1093/eurheartj/ehac118
Close - Share Icon Share
With thanks to Amelia Meier-Batschelet, Johanna Hugger, and Martin Meyer for help with compilation of this article.
 For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
This issue opens with the ‘The year in cardiovascular medicine 2021: imaging’ contribution from Chiara Bucciarelli-Ducci from the Royal Brompton and Harefield NHS Trust: Royal Brompton and Harefield NHS Foundation Trust in London, UK, and colleagues.1 The authors point out that cardiovascular imaging continues to play an important role in improving risk stratification and management in patients with cardiovascular disease. In 2021, COVID-19 continued to impact the healthcare landscape, resulting in reduced access to hospital-based cardiovascular care for acute presentations, including reduced routine diagnostic cardiovascular testing. Imaging played a key role in the understanding of the presence and extent of myocardial damage caused by the coronavirus infection. What has dominated the imaging literature beyond the pandemic is novel data on valvular heart disease, the increasing use of artificial intelligence applied to imaging, and the use of advanced imaging modalities in both ischaemic heart disease and cardiac amyloidosis
The increasing volume and richness of healthcare data collected during routine clinical practice have not yet translated into significant numbers of actionable insights that have systematically improved patient outcomes. An evidence–practice gap continues to exist in healthcare. In a Special Article entitled ‘Nudging within learning health systems: next generation decision support to improve cardiovascular care’, Yang Chen from the University College London in the UK, and colleagues contest that this gap can be reduced by assessing the use of nudge theory as part of clinical decision support systems (CDSS).2 Deploying nudges to modify clinician behaviour and improve adherence to guideline-directed therapy represents an underused tool in bridging the evidence–practice gap. In conjunction with electronic health records and newer devices including artificial intelligence algorithms that are increasingly integrated within learning health systems, nudges such as CDSS alerts should be iteratively tested for all stakeholders involved in health decision-making: clinicians, researchers, and patients alike. Not only could they improve the implementation of known evidence, but the true value of nudging could lie in areas where traditional randomized controlled trials are lacking, and where clinical equipoise and variation dominate. The opportunity to test CDSS nudge alerts and their ability to standardize behaviour in the face of uncertainty may generate novel insights and improve patient outcomes in areas of clinical practice currently without a robust evidence base. Thus, a learning health system with nudge, CDSS, and artificial intelligence-powered analyses can form core parts of the learning cycle.3–5 Nudges within the CDSS can be used to either promote better adherence to guideline-directed therapy or test new hypotheses whenever there is clinical equipoise, identified through variation in clinical practice owing to the lack of robust evidence in that context.
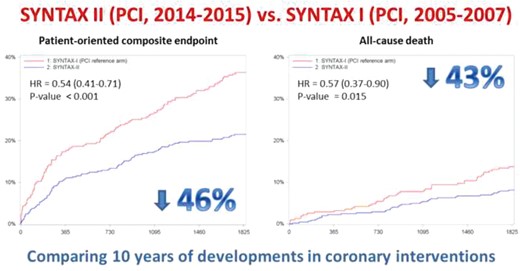
Comparison of outcomes after PCI using either the Syntax or Syntax II strategies.11
This Issue then continues with a focus on interventional cardiology. Percutaneous coronary intervention (PCI) is regarded as the standard of care for patients with non-complex single-vessel coronary artery disease who remain symptomatic despite optimal medical therapy. Conversely, in patients with medium or high anatomical complexity, which involves all three vessels, coronary artery bypass graft (CABG) surgery continues to be the recommended modality of revascularization.5–10 The SYNTAX II study evaluated the impact of advances in PCI, integrated into a single revascularization strategy, on outcomes of patients with de novo three-vessel disease (3VD). In a Fast Track clinical research article entitled ‘Five-year outcomes after state-of-the-art percutaneous coronary revascularization in patients with de novo three-vessel disease: final results of the SYNTAX II study’, Adrian Banning from the John Radcliffe Hospital in Oxford, UK, and colleagues employed decision-making utilizing the SYNTAX score II, use of coronary physiology, thin-strut biodegradable polymer drug-eluting stents, intravascular ultrasound, enhanced treatments of chronic total occlusions, and optimized medical therapy.11 Patients treated with this approach were compared with pre-defined patients from the SYNTAX I trial. SYNTAX II was a multicentre, single-arm, open-label study of patients requiring revascularization who demonstrated clinical equipoise for treatment with either CABG or PCI, predicted by the SYNTAX score II. The primary endpoint was major adverse cardiac and cerebrovascular events (MACCE), which included any revascularization. The comparators were a matched PCI cohort trial and a matched CABG cohort, both from the SYNTAX I trial. At 5 years, the MACCE rate in SYNTAX II was significantly lower than in the SYNTAX I PCI cohort (21% vs. 36%, P < 0.001). All-cause mortality was lower in SYNTAX II (8.1% vs. 13.8%, P = 0.013), reflecting a lower rate of cardiac death (2.8% vs. 8.4%, P < 0.001). MACCE in SYNTAX II and pre-defined patients in the SYNTAX I CABG cohort were similar (21.5% vs. 24.6%, P = 0.35) (Figure 1).
The authors conclude that use of the SYNTAX II PCI strategy in patients with de novo 3VD led to improved and durable clinical results when compared with pre-defined patients treated with PCI in the original SYNTAX I trial. A pre-defined exploratory analysis found no significant difference in MACCE between SYNTAX II PCI and matched SYNTAX I CABG patients at 5-year follow-up. The contribution is accompanied by an Editorial by Zaid Almarzooq and Robert Yeh from the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology at Beth Israel Deaconess Medical Center in Boston, MA, USA.12 The authors point out that overall, the SYNTAX II study confirms how developments in PCI technology and techniques have translated into better outcomes since the SYNTAX I trial. The results of the exploratory analysis comparing ‘State of the Art’ PCI with historical CABG emphasize the need for a more contemporary randomized trial that accounts for the recent advancements in both PCI and CABG. More importantly, for patients to realize the benefits of a decade's worth of advancement in the science of PCI, interventional cardiologists need to firmly commit themselves to incorporating the contemporary best practices that their patients deserve.
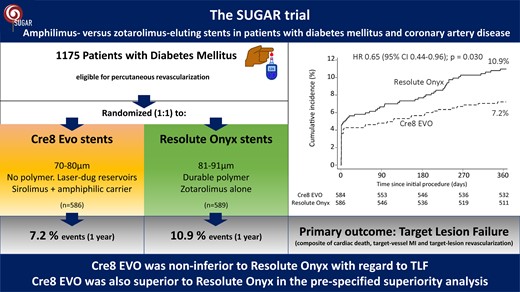
In the SUGAR trial, 1175 patients with diabetes mellitus and coronary artery disease were randomly assigned to receive Cre8 EVO or Resolute Onyx stents. Patients allocated to Cre8 EVO stents had a reduced risk of target lesion failure at 1-year follow-up.20
It is well recognized that patients with diabetes mellitus represent a high-risk subset.13–19 In particular, they are at high risk of adverse events after PCI, with no differences in outcomes between most contemporary drug-eluting stents. The Cre8 EVO stent releases a formulation of sirolimus with an amphiphilic carrier from laser-dug wells, and has shown clinical benefits in diabetes. In a second Fast Track clinical research article entitled ‘Amphilimus- vs. zotarolimus-eluting stents in patients with diabetes mellitus and coronary artery disease: the SUGAR trial’, Rafael Romaguera from the University of Barcelona in Spain, and colleagues aimed to compare Cre8 EVO stents with Resolute Onyx stents (a contemporary polymer-based zotarolimus-eluting stent) in patients with diabetes.20 This investigator-initiated, randomized, controlled, assessor-blinded trial at 23 sites in Spain enrolled eligible diabetic patients requiring PCI. A total of 1175 patients were randomly assigned (1:1) to receive Cre8 EVO or Resolute Onyx stents. The primary endpoint was target lesion failure, defined as a composite of cardiac death, target vessel myocardial infarction, and clinically indicated target lesion revascularization at 1-year follow-up. The trial had a non-inferiority design with a 4% margin for the primary endpoint. A superiority analysis was planned if non-inferiority was confirmed. There were 106 primary events, 42 (7.2%) in the Cre8 EVO group and 64 (10.9%) in the Resolute Onyx group [hazard ratio (HR) 0.65; Pnon-inferiority < 0.001; Psuperiority = 0.030] (Figure 2). Probable or definite stent thrombosis and all-cause death were not significantly different between groups.
The authors conclude that in patients with diabetes, Cre8 EVO stents were non-inferior to Resolute Onyx stents regarding the target lesion failure composite outcome. An exploratory analysis for superiority at 1 year suggests that the Cre8 EVO stents might be superior to Resolute Onyx stents regarding the same outcome. This manuscript is accompanied by an Editorial by Robert A. Byrne, Himanshu Rai, and Róisín Colleran from the Department of Cardiology and Cardiovascular Research Institute (CVRI) Dublin in Ireland.21 The authors conclude that in spite of some limitations, the results of the trial are difficult to dismiss. While further replication in additional patient cohorts would be important, the findings appear robust enough to stand on their own for now. Stent design modifications are often hypothesized to confer incremental advantages in clinical performance; not infrequently, however, the promise fails to deliver when put to the test in an objective clinical investigation. In the case of the SUGAR trial, the combination of unmet clinical need, iterative development of stent technology, and positive data from an independently conducted study produces a compelling narrative that will challenge clinicians to confront the topic of stent choice in patients with diabetes.
The choice between single or multiple arterial bypass graft surgery is still debated.22,23 In a Clinical Research article entitled ‘Single or multiple arterial bypass graft surgery vs. percutaneous coronary intervention in patients with three-vessel or left main coronary artery disease’, Piroze Davierwala from the Toronto General Hospital in Canada, and colleagues sought to compare long-term all-cause mortality between patients receiving PCI and CABG using multiple (MAG) or single arterial grafting (SAG).7 The current study is a post-hoc analysis of the SYNTAX Extended Survival Study, which compared PCI with CABG in patients with 3VD and/or left main coronary artery disease (LMCAD), and evaluated survival with ≥10 years of follow-up. The primary endpoint was all-cause mortality at maximum follow-up (median 11.9 years) assessed in the as-treated population. Of the 1743 patients, 901 (52%) underwent PCI, 532 (30%) received SAG, and 310 (18%) had MAG. All-cause death occurred in 34, 33, and 23% of patients in the PCI, SAG, and MAG groups, respectively (P < 0.001). MAG (adjusted HR 0.66), but not SAG (adjusted HR 0.83), was associated with significantly lower all-cause mortality compared with PCI. In patients with revascularization of all three major myocardial territories, a positive correlation was observed between the number of myocardial territories receiving arterial grafts and survival (Ptrend = 0.003).
The authors indicate that their findings suggest that MAG might be the more desirable configuration for CABG to achieve lower long-term all-cause mortality than PCI in patients with 3VD and/or LMCAD. The contribution is accompanied by an Editorial by Joanna Chikwe from Cedars-Sinai Medical Center in Los Angeles, CA, USA and Ottavio Alfieri from the S. Raffaele University Hospital in Milan, Italy.24 Chikwe and Alfieri conclude that major methodological limitations largely explain the discordance between the authors’ findings and those of four landmark randomized trials that consistently show significant and substantial event-free survival benefits with CABG compared with PCI in patients with multivessel disease, left main stem disease, and diabetes. A large, randomized trial incorporating newer generation drug-eluting stents and antiplatelet therapy, advances in intravascular imaging, and more complete revascularization could answer the very valid question concerning the long-term superiority of multi-arterial revascularization over PCI that this post-hoc analysis of SYNTAX cannot adequately address.
In a Clinical Research article entitled ‘Cost-effectiveness analysis of left atrial appendage occlusion in patients with atrial fibrillation and contraindication to oral anticoagulation’, Frida Labori from the University of Gothenburg, Sweden, and colleagues sought to estimate the cost-effectiveness of percutaneous left atrial appendage occlusion (LAAO) compared with standard stroke prevention care for patients with atrial fibrillation and contraindication to oral anticoagulation (OAC) in a Swedish healthcare and public sector perspective.25 Labori and colleagues used a combined decision tree and cohort Markov model to estimate costs and quality-adjusted life-years (QALYs) over a lifetime horizon with LAAO compared with standard of care where the treatment effect is based on a recent meta-analysis. According to their analysis, LAAO gives more QALYs than standard of care (7.11 vs. 6.12). Furthermore, LAAO treatment is related to the first-year cost of €14 984 and higher average healthcare costs over the lifetime by about €4010, which gives an incremental cost-effectiveness ratio of LAAO vs. standard of care at €4047 per gained QALY. From a public sector perspective, LAAO reduces average costs due to substantial reductions in long-term care, and thus implies that LAAO is dominant from a public sector perspective (lower average costs and better health outcomes).
The authors conclude that LAAO can be considered cost-effective compared with standard of care for individuals with AF and contraindication to OAC. However, these results must be confirmed in health economic evaluations alongside the ongoing randomized clinical trials. The manuscript is accompanied by an Editorial by Amneet Sandhu and Paul Varosy from the University of Colorado in Aurora, CO, USA.26 The authors conclude that with significant growth in the use of LAAO worldwide, additional cost-effectiveness analyses in other countries and with different model inputs will be important to determine whether LAAO is similarly cost-effective elsewhere in validation—or refutation—of the findings of Labori and colleagues.
The issue is also complemented by a Discussion Forum contribution. In a commentary entitled ‘Ten-year survival is not survivors at 10 years’, Kareem Bedeir from Cardiothoracic and Vascular Surgery Associates in Mobile, AL, USA comments on the recent publication ‘Ten-year all-cause death after percutaneous or surgical revascularization in diabetic patients with complex coronary artery disease’ by Rutao Wang from the National University of Ireland and colleagues.27,28 Our Weekly Journal Scan Editors have also discussed this paper in a recent contribution.29
The editors hope that this issue of the European Heart Journal will be of interest to its readers.




