-
PDF
- Split View
-
Views
-
Cite
Cite
C Montalto, S Carli, C Gargiulo, F A Russo, R Gazmawi, L Tua, M Galazzi, M Acquaro, G Guida, G Disabato, A Attanasio, R Camporotondo, S Guida, L Oltrona-Visconti, S Leonardi, Prognosis and prescriptions of glifozines in candidates patients in a prospective, multicenter, quality-improvement study of patients with acute coronary syndrome, European Heart Journal, Volume 42, Issue Supplement_1, October 2021, ehab724.1211, https://doi.org/10.1093/eurheartj/ehab724.1211
Close - Share Icon Share
Abstract
Sodium-glucose transporter 2 inhibitors (SGLT2-i) have demonstrated substantial improvement in clinical outcomes for patients with heart failure (HF) and chronic kidney disease (CKD) with or without diabetes mellitus (DM). Prescription patterns and outcome of SGLT2-i candidates in patients hospitalized for an acute coronary syndrome (ACS) are less well established.
We aimed to assess the proportion of candidates to SGLT2-i and to characterize their clinical outcome in a contemporary, prospective, multicenter, quality-improvement study of all-comers patients with ACS. We also aimed to ascertain prescriptions of SGLT2-i at discharge.
Between 2018 and 2020, subjects were enrolled in the study; baseline characteristics and medications were prospectively collected, and patients were followed-up at 1 year. Subjects were considered candidates to SGLT2-i if any of the following were: (i) known (medically treated) or new (HbA1c >6.5%) diagnosis of type 2 DM; (ii) left ventricular systolic dysfunction (LVSD; new or known left ventricular ejection fraction <40%) or clinical HF; (iii) CKD (estimated glomerular filtration rate 25–74 mL/min/m2, according to DAPA-CKD trial eligibility).
Of the 2804 consecutive ACS patients enrolled, 798 (28.5%) had new or known DM and only 10 were already on SGLT2-I at baseline. Additionally, 1,098 (39.2%) patients qualified for SGLT2-i prescription as having known or new LVSD or HF, and 803 (28.6%) as having CKD. (Fig. 1A) Overall, these 1,767 (63.1%) SGLT2-i candidates had substantially higher hazard of death as compared to no candidate (Hazard Ratio [HR] at 1-year: 6.82; 95% Confidence Interval: 4.32–10.8; p<0.001; Fig. 1B) and each indication to SGLT2-i independently predicted death at 1 year (HR: 2.30/2.11/3.06; 95% CI: 1.78–2.97/1.62–2.74/2.35–3.97; all p<0.0001; for DM, HF, CKD, respectively; Fig. 2). At discharge, only 18 (1.0% of the candidates) were prescribed with SGLT2-i and, of those with DM, having a diabetological consultation before discharged modestly but significantly increased the likelihood of being discharged with SGLT2-i (4.3% vs. 6.6%; p=0.0015).
Most (two out of three) contemporary ACS patients are candidates to SGLT2-i therapy, and they have a significant and substantial higher risk of mortality at 1-year as compared to no candidates. Current prescription rates are still extremely low (1%) and highlight opportunity for quality improvement and multidisciplinary decision-making.
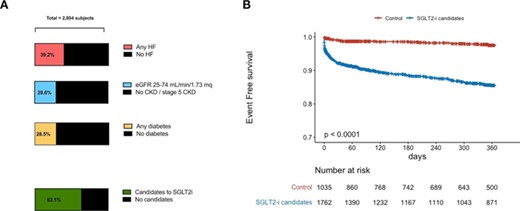
Figure 1
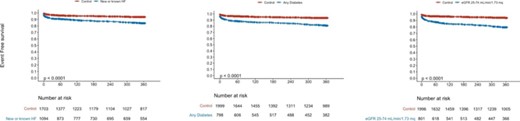
Figure 2
- acute coronary syndromes
- left ventricular ejection fraction
- pharmacotherapy
- diabetes mellitus
- consultation
- kidney failure, chronic
- heart failure
- diabetes mellitus, type 2
- decision making
- hemoglobin a, glycosylated
- inpatients
- diagnosis
- mortality
- treatment outcome
- left ventricular systolic dysfunction
- quality improvement
- glomerular filtration rate, estimated
- sodium-glucose transporter 2 inhibitors



