-
PDF
- Split View
-
Views
-
Cite
Cite
M D Fridman, T Tofighi, C P S Fan, R M Hamilton, Resting ECG measurements can identify abnormalities in children with catecholaminergic polymorphic ventricular tachycardia, European Heart Journal, Volume 42, Issue Supplement_1, October 2021, ehab724.0305, https://doi.org/10.1093/eurheartj/ehab724.0305
Close - Share Icon Share
Abstract
Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT) is a rare inherited disease characterized by exercise- or emotionally-triggered life-threatening ventricular arrhythmias. The resting ECG is considered to be normal and diagnosis has depended on exercise testing that is difficult acutely post-arrest or in young children.
To identify resting ECG abnormalities in children with CPVT through assessment of measurement matrix parameters compared to a cohort of normal children.
A discovery cohort of 65 CPVT patients from the Electrophysiology program were identified. After excluding those on antiarrhythmics or in an arrhythmia at the time of their baseline ECG, 31 cases were matched 3:1 by age and sex with 93 healthy controls. Each individual had baseline ECG parameters and 180 machine-derived ECG amplitudes and durations (measurement matrix) measured. Statistical differences between ECG measures were assessed using Student's T-Test adjusted with a False Detection Rate of 1%. Significant measures were processed in a machine-learning algorithm to derive a Tree Model to differentiate individuals with and without CPVT.
No significant differences were detected between CPVT patients who had and did not have a cardiac arrest. Comparing the CPVT and control cohorts, significant repolarization differences were seen in the amplitudes of lateral (I, negative aVR, V5, V6) and anterior leads (V2, V3, V4) at the J-point, ST midpoint, ST endpoint, and T-wave. Specifically, individuals with CPVT had significantly lower mean amplitudes in all aforementioned leads except aVR where the mean amplitudes were higher. These data were then used to create a Tree Model of the discovery cohort displayed in Figure 1 with a resulting R2 of 0.74, sensitivity of 0.81, and specificity of 0.98.
Baseline differences in repolarization are detectable in the left and anterior chest leads using machine-derived measurements of baseline ECGs in patients with CPVT, which may guide clinical suspicion when evaluating the resting ECG. These results warrant further analysis including testing of the Tree Model with a validation cohort.
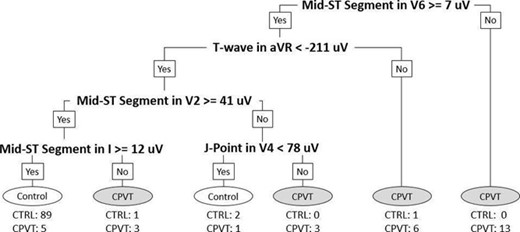
Figure 1. CPVT Tree Model
- anti-arrhythmia agents
- cardiac arrhythmia
- cardiac arrest
- electrocardiogram
- t wave feature
- exercise stress test
- exercise
- genetic disorder
- awards and prizes
- canada
- child
- electrophysiology
- trees (plant)
- diagnosis
- heart
- ventricular arrhythmia
- chest leads
- ecg abnormal
- well child
- ontario
- catecholaminergic polymorphic ventricular tachycardia
- machine learning



