-
PDF
- Split View
-
Views
-
Cite
Cite
Filippo Crea, How epidemiology can improve the understanding of cardiovascular disease: from mechanisms to treatment, European Heart Journal, Volume 42, Issue 44, 21 November 2021, Pages 4503–4507, https://doi.org/10.1093/eurheartj/ehab797
Close - Share Icon Share
 For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
Life is more than work, for dedicated cardiologists too; thus, we enjoy wine, drinks, sweets, and coffee. Are these forbidden joys or are they possibly even protective?1–3 This Focus Issue on epidemiology and prevention contains the Viewpoint article ‘Wine, chocolate, and coffee: forbidden joys?’ by Thomas Lüscher from the Royal Brompton and Harefield Hospitals in London, UK.4 Lüscher concludes that wine is truly a joy, but at best neutral when consumed in moderation. Chocolate is a joy for our cardiovascular system, if consumed in dark, bitter form. Coffee wakes us up, less so if drunk regularly, and might even be protective at a dose of up to four cups a day.
Atrial cardiomyopathy has been suggested to play an important role in the development of atrial fibrillation (AF).5,6 In a Clinical Research article entitled ‘Genome-wide association study identifies 18 novel loci associated with left atrial volume and function’, Gustav Ahlberg from the University Hospital of Copenhagen in Denmark, and colleagues7 used the UK Biobank, which is a large prospective population study with available phenotypic and genetic data, to perform genome-wide association studies on five volumetric and functional left atrial (LA) variables in 35 658 European individuals. They identified 18 novel genetic loci, mapped to genes with known roles in cardiomyopathy (e.g. MYO18B, TTN, DSP, and ANKRD1) and arrhythmia (e.g. TTN, CASQ2, MYO18B, and C9orf3) associated with the volumetric and functional LA variables. Furthermore, high genetic correlations were observed between LA volume and function and stroke, which was most pronounced for the LA passive emptying fraction. To investigate whether the genetic risk of AF was associated with LA traits that precede overt AF, Ahlberg and colleagues produced a polygenetic risk score for AF. They found that polygenetic risk for AF was associated with increased LA volume and decreased LA function in participants without AF.
The results found in this study suggest that compromised LA function may share genetic underpinning with cardiomyopathy. Furthermore, they show that the genetic risk of AF influences LA structure prior to diagnosis of AF, suggesting an intrinsic relationship. The manuscript is accompanied by an Editorial by Renate Schnabel and Stephan Camen from the University Heart and Vascular Center Hamburg in Germany.8 The authors note that the present study provides convincing evidence for a genetic component in LA morphology and function, supporting the concept of atrial cardiomyopathy as an intrinsic disease entity. However, the (clinical) definition of atrial cardiomyopathy remains vague, and more research is needed to define its genetic, morphological, and functional characteristics, ideally combining different imaging modalities and modern functional parameters. In addition, the potential prognostic impact of atrial cardiomyopathy and its treatment through risk factor modification, medication, or ablation in AF needs to be investigated.
The incidence of ST-elevation myocardial infarction (STEMI) in European countries ranges between 40 and 140/100 000/year, which equates to >500 000 patients with STEMI being admitted each year. Despite improvements in management, STEMI remains one of the leading causes of death in Europe and worldwide.9 In a Clinical Research article entitled ‘Reperfusion therapies and in-hospital outcomes for ST-elevation myocardial infarction in Europe: the ACVC-EAPCI EORP STEMI Registry of the European Society of Cardiology’, Uwe Zeymer from the Klinikum der Stadt Ludwigshafen and Institut für Herzinfarktforschung in Ludwigshafen am Rhein, Germany, and colleagues aimed to determine the contemporary use of reperfusion therapy in the European Society of Cardiology member and affiliated countries, and adherence to ESC clinical practice guidelines in patients with STEMI.10 They assessed STEMI patients with symptom onset <24 h in 196 centres across 29 countries. A total of 11 462 patients were enrolled, for whom primary percutaneous coronary intervention (total cohort frequency 72.2%; country frequency range 0–100%), fibrinolysis (18.8%; 0–100%), and no reperfusion therapy (9.0%; 0–75%) were performed. Corresponding in-hospital mortality rates from any cause were 3.1, 4.4, and 14.1%. Achievement of quality indicators was reported for 93% (region range 85–97%) for the performance of reperfusion therapy of all patients with STEMI <12 h and for 54.4% (region range 37.1–70.1%) for timely reperfusion (Figure 1).
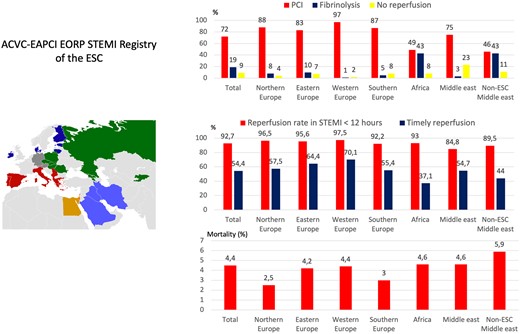
Graphical Abstract (from Zeymer U, Ludman P, Danchin N, Kala P, Laroche C, Sadeghi M, Caporale R, Shaheen SM, Legutko J, Iakobsishvili Z, Alhabib KF, Motovska Z, Studencan M, Mimoso J, Becker D, Alexopoulos D, Kereseselidze Z, Stojkovic S, Zelveian P, Goda A, Mirrakhimov E, Bajraktari G, Al-Farhan H, Śserpytis P, Raungaard B, Marandi T, Moore AM, Quinn M, Karjalainen PP, Tatu-Chitolu G, Gale CP, Maggioni AP, Weidinger F. Reperfusion therapies and in-hospital outcomes for ST-elevation myocardial infarction in Europe: the ACVC-EAPCI EORP STEMI Registry of the European Society of Cardiology. See pages 4536–4549).
Zeymer and colleagues conclude that the use of reperfusion therapy for STEMI in ESC member and affiliated countries is high. Primary PCI is the most frequently used treatment, and associated total in-hospital mortality is <5%. However, there is geographic variation in the use of primary PCI, which is associated with differences in in-hospital mortality. This manuscript is accompanied by an Editorial by Cindy Grines from the Northside Hospital Cardiovascular Institute in Atlanta, GA, USA and Sameer Mehta from the Lumen Global Foundation, Miami, FL, USA.11 Grines and Mehta conclude that further improvements in STEMI care will require strong commitment among the medical community as well as support from hospitals and regional funding agencies. It is hoped that cardiology societies can assist with efforts to navigate governmental bureaucracy and improve funding of STEMI care.
Acute coronary syndrome (ACS) is frequently accompanied by AF, which may be previously known or first-time detected.12 Previously known AF is well recognized to further aggravate the prognosis of patients with ACS; however, contemporary, unselected data on the subgroup of patients admitted with first-time detected AF are sparsely examined, and are missing in particular in a nationwide setting. In a Clinical Research article entitled ‘Incidence of ischaemic stroke and mortality in patients with acute coronary syndrome and first-time detected atrial fibrillation: a nationwide study’, Jeppe Kofoed Petersen from the Rigshospitalet in Copenhagen, Denmark, and colleagues examine contemporary data on the 1-year prognosis of patients surviving an ACS and concomitant first-time detected AF.13 Using Danish nationwide registries, the authors identified all patients surviving a first-time admission with ACS from 2000 to 2018 and grouped them into (i) those without AF prior to or during ACS; (ii) those with a history of AF; and (iii) those with first-time detected AF during admission with ACS. With 1 year of follow-up, rates of ischaemic stroke, death, and bleeding were compared between study groups using multivariable adjusted Cox proportional hazards analysis. A total of 161 266 ACS survivors were included: 135 878 (84%) without AF, 18 961 (12%) with a history of AF, and 6427 (4%) with first-time detected AF at admission with ACS. Compared with those without AF, the adjusted 1-year rates of outcomes were as follows: ischaemic stroke [hazard ratio (HR) 1.38 for patients with a history of AF and HR 1.67 for patients with first-time detected AF]; mortality (HR 1.25 for patients with a history of AF and HR 1.52 for patients with first-time detected AF); and bleeding (HR 1.22 for patients with a history of AF and HR 1.28 for patients with first-time detected AF).
The authors conclude that in patients with ACS, first-time detected AF appeared to be at least as strongly associated with the 1-year rates of ischaemic stroke, mortality, and bleeding as compared with patients with a history of AF. The contribution is accompanied by an Editorial by Jur ten Berg and Wilbert Bor from the St. Antonius Hospital, Nieuwegein, The Netherlands.14 The authors note that these findings should encourage active consideration of the combination of oral anticoagulants and antiplatelet therapy (preferably single antiplatelet therapy with clopidogrel) as the optimal antithrombotic therapy in ACS patients with newly diagnosed AF.
While greater physical activity (PA) is associated with improved health outcomes, the direct links between distinct components of PA, their changes over time, and cardiorespiratory fitness are incompletely understood. In a Clinical Research article entitled ‘Physical activity and fitness in the community: the Framingham Heart Study’, Matthew Nayor from the Boston University School of Medicine in Boston, MA, USA, and colleagues studied this further.15 Maximum effort cardiopulmonary exercise testing (CPET) and objective PA measures [sedentary time (SED), steps/day, and moderate–vigorous PA (MVPA)] via accelerometers worn for 1 week concurrent with CPET and 7.8 years prior were obtained in 2070 Framingham Heart Study participants. Increases of 17 min of MVPA/day or 4312 steps/day, or reductions of 249 min of SED per day between the two exam cycles corresponded to a 5% higher peak VO2. Individuals with high (above-mean) steps or MVPA demonstrated above-average peak VO2 values regardless of whether they had high or low SED (Figure 2).
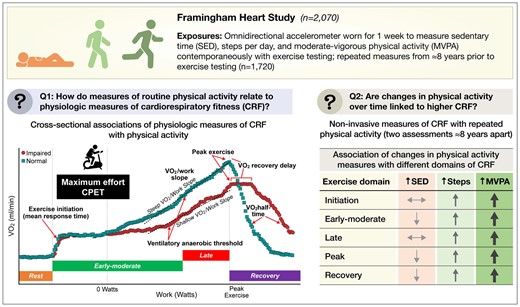
Graphical Abstract (from Nayor M, Chernofsky A, Spartano NL, Tanguay M, Blodgett JB, Murthy VL, Malhotra R, Houstis NE, Velagaleti RS, Murabito JM, Larson MG, Vasan RS, Shah RV, Lewis GD. Physical activity and fitness in the community: the Framingham Heart Study. See pages 4565–4575).
Nayor et al. conclude that their findings provide a detailed assessment of relationships of different types of PA with multidimensional cardiorespiratory fitness measures and suggest that favourable longitudinal changes in PA (and MVPA in particular) are associated with greater objective fitness. The manuscript is accompanied by an Editorial by Bjarne Nes and Jon Magne Letnes from the Norwegian University of Science and Technology, Trondheim, Norway.16 The authors note that in the end, Nayor and colleagues have some encouraging findings which should resonate with the general public as well, as their findings indicate that moderate increases in daily walking or slight increases in MVPA may compensate our increasingly sedentary lifestyle. Although the reported effect estimates may seem small, when considering the strong relationship between cardiorespiratory fitness and health outcomes, the benefit on the health of a population from a modest increase in regular activity may be substantial.
Benzbromarone is a uricosuric agent inhibiting a renal tubular transporter, URAT-1. It shows high efficacy and safety in general even for patients with chronic kidney disease, but was not approved in the USA and was withdrawn from some European countries based on several hepatotoxicity reports. However, the decision to withdraw the drug has often been questioned based on the risk estimated as <1:17 000. Currently, it is still actively used to treat gout in Asia including South Korea, some countries of Europe, and South America. The 2016 EULAR guideline for gout management recommends using benzbromarone alone or in combination with allopurinol when the initial treatment with allopurinol is not effective enough to lower serum urate levels. In a Clinical Research article entitled ‘Cardiovascular risk associated with allopurinol vs. benzbromarone in patients with gout’, Eun Ha Kang from Seoul National University Bundang Hospital, and colleagues compared cardiovascular risk among patients with gout who initiated allopurinol vs. benzbromarone.17 Using the Korean National Health Insurance claims data (2002–2017), they conducted a cohort study of 124 434 gout patients who initiated either allopurinol (n = 103 695) or benzbromarone (n = 20 739), matched on propensity score at a 5:1 ratio. The primary outcome was a composite cardiovascular endpoint of myocardial infarction, stroke/transient ischaemic attack, or coronary revascularization. Over a mean follow-up of 1.16 years, 2258 patients developed a composite cardiovascular event. The incidence rate of the composite cardiovascular event was higher for allopurinol (1.81 per 100 person-years) than for benzbromarone (1.61 per 100 person-years) with a HR of 1.22. The HR for all-cause mortality was 1.66 among allopurinol initiators compared with benzbromarone.
The authors conclude that in this large population-based cohort of gout patients, allopurinol is associated with an increased risk of composite cardiovascular events and all-cause mortality compared with benzbromarone. The contribution is accompanied by an Editorial by Giulia Fiorini and Claudio Borghi from the University of Bologna in Italy.18 The authors note that the effective treatment of gout is a primary therapeutic need that should involve the correct identification of the patients and the prevention of both articular and cardiovascular diseases. Xanthine oxidoreductase inhibitors and uricosuric agents are the pillars of treatment, with some differences in their utilization across the world. They intercept the two most important mechanisms involved in hyperuricaemia, i.e. overproduction and/or underexcretion of urate. Post-hoc analysis of adjusted real-life data may provide an outstanding example of how to generate a ‘working hypothesis’ that should be carefully tested in perspective.
Angina pectoris has been considered to be mainly caused by atherosclerotic obstructive coronary artery disease (CAD). However, up to 50% of patients undergoing diagnostic coronary angiography for typical chest pain have angiographically normal coronary arteries or non-obstructive CAD. In such cases, coronary functional abnormalities are implicated, including epicardial coronary artery spasm and coronary microvascular dysfunction. The latter is typically defined as increased susceptibility to vasoconstrictor stimuli resulting in microvascular spasm and/or impaired dilatation of coronary microvessels, with a resultant inadequate increase in blood flow in response to stress.19–22 In a Clinical Research article entitled ‘Clinical characteristics and prognosis of patients with microvascular angina: an international and prospective cohort study by the Coronary Vasomotor Disorders International Study (COVADIS) Group’, Hiroaki Shimokawa from the Tohoku University Graduate School of Medicine in Sendai, Japan, and colleagues sought to provide multinational, multiethnic data on the clinical characteristics and prognosis of patients with microvascular angina (MVA).23 The Coronary Vasomotor Disorders International Study Group recently proposed the diagnostic criteria for MVA. Shimokawa et al. prospectively evaluated the clinical characteristics of patients according to these criteria and their prognosis. The primary endpoint was the composite of major cardiovascular events (MACE), verified by institutional investigators, which included cardiovascular death, non-fatal myocardial infarction, non-fatal stroke, and hospitalization due to heart failure or unstable angina. During the period from 1 July 2015 to 31 December 2018, a total of 686 patients with MVA were registered from 14 institutes in seven countries across four continents. Among them, 64% were female and the main ethnic groups were Caucasians (61%) and Asians (29%). During follow-up of a median of 398 days, 78 MACE occurred (6.4% in men vs. 8.6% in women, P = 0.19). Multivariable Cox proportional hazard analysis disclosed that hypertension and previous history of CAD, including ACS and stable angina pectoris, were independent predictors of MACE. There was no sex or ethnic difference in prognosis, although women had lower Seattle Angina Questionnaire scores than men (P < 0.05).
The authors conclude that this first international study provides novel evidence that MVA is an important health problem regardless of sex or ethnicity, that a diagnosis of MVA portends a substantial risk of MACE associated with hypertension and previous history of CAD, and that women have a lower quality of life than men despite the comparable prognosis. The article is accompanied by an Editorial by Kevin Cheng and Ranil de Silva from the Imperial College London in the UK.24 The authors conclude that the results of the current study in combination with the outcomes of a pragmatic trial evaluating conventional antianginal drugs (WARRIOR, NCT03417388) and a randomized placebo-controlled trial of the endothelin antagonist zibotentan (PRIZE, NCT04097314) have the potential to offer significant improvements in current management. Rigorous application of guideline-directed management of conventional cardiovascular risk factors is essential for patients with MVA. These systematic evaluations will hopefully go a significant way towards addressing the unmet clinical needs and adverse prognosis of patients with MVA.
The editors hope that readers of this issue of the European Heart Journal will find it of interest.
With thanks to Amelia Meier-Batschelet, Johanna Huggler, and Martin Meyer for help with compilation of this article.




