-
PDF
- Split View
-
Views
-
Cite
Cite
T Satou, H Kitahara, K Ishikawa, T Nakayama, Y Fujimoto, K Sano, Y Kobayashi, Short-term risk stratification using CADILLAC risk score in patients with ST elevation myocardial infarction, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.1352, https://doi.org/10.1093/ehjci/ehaa946.1352
Close - Share Icon Share
Abstract
The recent reperfusion therapy for ST-elevation myocardial infarction (STEMI) has made the length of hospital stay shorter without adverse events. CADILLAC risk score is reportedly one of the risk scores predicting the long-term prognosis in STEMI patients.
To invenstigate the usefulness of CADILLAC risk score for predicting short-term outcomes in STEMI patients.
Consecutive patients admitted to our university hospital and our medical center with STEMI (excluding shock, arrest case) who underwent primary PCI between January 2012 and April 2018 (n=387) were enrolled in this study. The patients were classified into 3 groups according to the CADILLAC risk score: low risk (n=176), intermediate risk (n=87), and high risk (n=124). Data on adverse events within 30 days after hospitalization, including in-hospital death, sustained ventricular arrhythmia, recurrent myocardial infarction, heart failure requiring intravenous treatment, stroke, or clinical hemorrhage, were collected.
In the low risk group, adverse events within 30 days were significantly less observed, compared to the intermediate and high risk groups (n=13, 7.4% vs. n=13, 14.9% vs. n=58, 46.8%, p<0.001). In particular, all adverse events occurred within 3 days in the low risk group, although adverse events, such as heart failure (n=4), recurrent myocardial infarction (n=1), stroke (n=1), and gastrointestinal bleeding (n=1), were substantially observed after day 4 of hospitalization in the intermediate and high risk groups.
In STEMI patients with low CADILLAC risk score, better short-term prognosis was observed compared to the intermediate and high risk groups, and all adverse events occurred within 3 days of hospitalization, suggesting that discharge at day 4 might be safe in this study population. CADILLAC risk score may help stratify patient risk for short-term prognosis and adjust management of STEMI patients.
Comparison of adverse events between low risk and intermediate-high risk groups
| . | Low risk (n=176) . | Intermediate-high risk (n=211) . | P-value . |
|---|---|---|---|
| Adverse event during hospitalization | 13 (7.4%) | 71 (33.6%) | <0.001 |
| In-hospital death | 1 (0.6%) | 7 (3.3%) | 0.125 |
| Sustained VT/VF | 4 (2.3%) | 3 (1.4%) | 0.808 |
| recurrment MI | 1 (0.6%) | 1 (0.5%) | 1.000 |
| HF requiring i.v. treatment | 9 (5.1%) | 61 (28.9%) | <0.001 |
| Stroke | 0 (0%) | 1 (0.5%) | 1.000 |
| Clinical hemorrhage | 0 (0%) | 5 (2.4%) | 0.109 |
| Others | 2 (1.1%) | 5 (2.4%) | 0.601 |
| . | Low risk (n=176) . | Intermediate-high risk (n=211) . | P-value . |
|---|---|---|---|
| Adverse event during hospitalization | 13 (7.4%) | 71 (33.6%) | <0.001 |
| In-hospital death | 1 (0.6%) | 7 (3.3%) | 0.125 |
| Sustained VT/VF | 4 (2.3%) | 3 (1.4%) | 0.808 |
| recurrment MI | 1 (0.6%) | 1 (0.5%) | 1.000 |
| HF requiring i.v. treatment | 9 (5.1%) | 61 (28.9%) | <0.001 |
| Stroke | 0 (0%) | 1 (0.5%) | 1.000 |
| Clinical hemorrhage | 0 (0%) | 5 (2.4%) | 0.109 |
| Others | 2 (1.1%) | 5 (2.4%) | 0.601 |
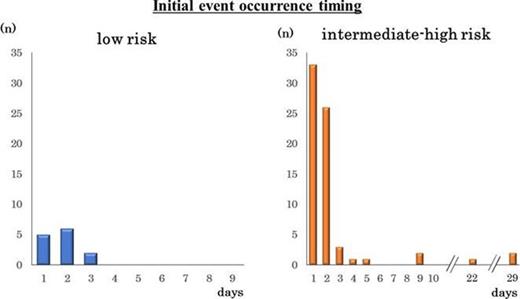
Initial event occurrence timing
Type of funding source: None
- myocardial infarction
- st segment elevation myocardial infarction
- coronary arteriosclerosis
- sustained ventricular tachycardia
- hemorrhage
- cerebrovascular accident
- ischemic stroke
- heart failure
- reperfusion therapy
- epidemiology
- gastrointestinal bleeding
- hospital mortality
- hospitals, university
- length of stay
- shock
- ventricular arrhythmia
- stratification
- adverse event



