-
PDF
- Split View
-
Views
-
Cite
Cite
P Lindqvist, E Tossavainen, M.Y Henein, Left atrial deformation in estimating left atrial pressure, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.0105, https://doi.org/10.1093/ehjci/ehaa946.0105
Close - Share Icon Share
Abstract
In the absence of mitral valve disease, elevated left atrial (LA) pressure reflects reduced left ventricular (LV) compliance and raised diastolic pressures, hence an important explanation for exertional breathlessness.
We studied 145 symptomatic patients, age 63±14 years, 55 males, using conventional transthoracic echocardiography guidelines protocol, including LA and LV myocardial deformation investigations along with simultaneous right heart catheterization using conventional techniques. From invasive measurements, pulmonary artery pressure (PAP), pulmonary capillary wedge pressure (PCWP) were measured and pulmonary vascular resistance (PVR) calculated. No patient had more than mild mitral or aortic valve disease.
LA strain rate during atrial systole (LASRa) was the strongest correlate with PCWP (r2=−0.39, p<0.001), over and above LASR during LV systole (LASRs) and peak LA longitudinal strain (PALS) (r2=−0.21 and −0.19, respectively, p<0.001 for both). Both LASRa and PALS predicted elevated PCWP >15 mmHg but only modestly (AUC= 0.55 and 0.52). The relationship between LASRa and PCWP was stronger in patients with post-capillary pulmonary hypertension compared to those with pre-capillary pulmonary hypertension (r2=0.21 vs. r2=0.02). However, the strongest relationship between LASRa and PCWP was in patients with LA volume >34 ml/m2 (r2=0.59, p<0.001, see figure) but other strain relationships did not improve after only including patients with increased LA volume. Finally, LASRa correlated modestly with the respective LVSRa (r=0.53, P<0.01), and to lesser extent with other cavity interaction correlations (r=0.26–0.48, p<0.01).
Despite being somehow related to ventricular function, left atrial strain rate during atrial contraction is the closest correlate to PCWP, particularly in patients with dilated LA cavity. These data should be of significant clinical value in daily management of symptomatic patients.
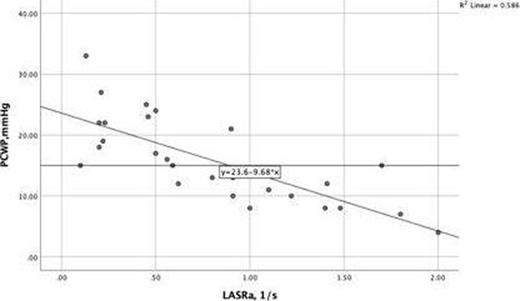
LASRaecho and PCWPrhc in patients with d
Type of funding source: None
- myocardium
- catheterization of right heart
- left atrium
- tissue doppler
- ventricular function
- dyspnea
- atrium
- left ventricle
- mitral valve disorders
- pulmonary wedge pressure
- systole
- diagnostic imaging
- guidelines
- pulmonary artery line
- echocardiography, transthoracic
- aortic valve disorders
- diastolic blood pressure
- pulmonary artery pressure
- systole, atrial
- pulmonary vascular resistance
- post-capillary pulmonary hypertension
- two-dimensional speckle tracking
- strain rate
- longitudinal strain
- left atrial pressure
- precapillary pulmonary hypertension



