-
PDF
- Split View
-
Views
-
Cite
Cite
M Tesic, Q Ciampi, A Djordjevic-Dikic, B Beleslin, L Cortigiani, A Palinkas, E Palinkas, A Nemes, F Rigo, C Borguezan-Daros, A Varga, G Agoston, B Villari, C Carpeggiani, E Picano, Stress Echo 2020 study group of the Italian Society of Cardiovascular Echography and Cardiovascular Imaging , Prognostic role of coronary flow velocity reserve in hypertrophic cardiomyopathy, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.0009, https://doi.org/10.1093/ehjci/ehaa946.0009
Close - Share Icon Share
Abstract
A reduction in coronary flow velocity reserve (CFVR) related to coronary microvascular dysfunction is a major mechanism for ischemia in hypertrophic cardiomyopathy (HCM).
To assess the functional correlates and prognostic value of CFVR during stress echocardiography (SE) in HCM.
We enrolled 201 HCM patients (age 51±14 years, 105 male, 52%; maximal wall thickness: 18±3 mm) studied with CFVR during exercise (n=33, 16.4%), dipyridamole (n=89, 44.3%) or adenosine (n=79, 39.3%) SE in 6 certified centers. CFVR was assessed using pulsed wave Doppler sampling in left anterior descending coronary artery. All patients completed the clinical follow-up.
During SE mean value of CFVR was 2.11±0.46. No patients showed regional wall motion abnormalities during stress. LV outflow tract obstruction (LVOTO) was present in 34 (16.9%) patients at rest and in 47 (23.4%) at peak stress. CFVR was inversely related to age (r=−0.229, p=0.001) and maximal wall thickness (r=−0.197, p=0.031). During a median follow-up of 26 months (IQ range: 12–48 months), 75 events in 63 patients occurred: 10 deaths, 33 new hospital admission for acute heart failure, 8 sustained ventricular tachycardias and 24 atrial fibrillations. Patients in the lowest tertile (≤1.88) showed the worse prognosis with higher incidence of follow-up events compared to median tertile (1.89–2.29) and highest tertile (≥2.30) (see figure). At multivariable analysis, NYHA functional class (HR: 2.234, 95% CI: 1.398–3.517, p=0.001), presence of LVOTO at rest (HR: 2.958, 95% CI: 1.074–3.570, p=0.028) and lowest tertile of CFVR (HR: 2.144, 95% CI: 1.126–4.081, p=0.011) were the independent predictors of follow-up events.
In HCM patients, reduction in CFVR is associated to a clearly worse outcome. The spectrum of prognostic stratification is expanded if the response is titrated according to a continuous scale.
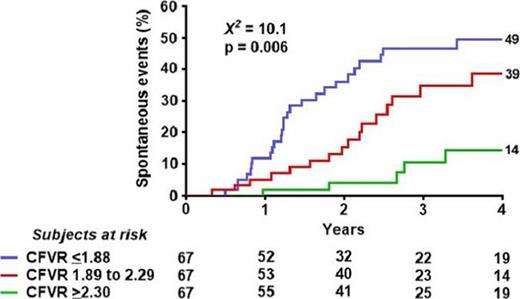
Figure 1
Type of funding source: None
- heart failure, acute
- adenosine
- atrial fibrillation
- hypertrophic cardiomyopathy
- dipyridamole
- ischemia
- left ventricular outflow obstruction
- microvascular angina
- tachycardia, ventricular
- doppler pulsed
- left ventricular wall motion
- anterior descending branch of left coronary artery
- stress echocardiography
- exercise
- follow-up
- patient prognosis
- stress
- stratification
- hospital admission
- new york heart association classification
- fluid flow



