-
PDF
- Split View
-
Views
-
Cite
Cite
Filippo Crea, Challenges in risk stratification of symptomatic and asymptomatic valvular heart disease: lessons from large observational studies, European Heart Journal, Volume 41, Issue 45, 1 December 2020, Pages 4289–4292, https://doi.org/10.1093/eurheartj/ehaa951
Close - Share Icon Share
 For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
This is a Focus Issue on valvular heart disease (VHD), which is progressively occupying the centre stage of cardiovascular medicine. Changing societal demographics and an ageing population (with increasing prevalence of degenerative disease), advances in imaging, and the explosion of interest in transcatheter interventional techniques (supported by a series of landmark clinical trials) have attracted clinicians, researchers, engineers, device manufacturers, and investors, and transformed the landscape of clinical management.1–4
The first contribution is a clinical research article entitled ‘Isolated tricuspid valve surgery: impact of aetiology and clinical presentation on outcomes’, by Julien Dreyfus from the Centre Cardiologique du Nord in Saint-Denis, France, and colleagues. The authors sought to identify determinants of in-hospital and mid-term outcomes after isolated tricuspid valve surgery as little is known regarding the impact of tricuspid regurgitation (TR), its mechanism, and clinical presentation.5 Among ∼5600 consecutive adult patients who underwent tricuspid valve surgery at 12 French tertiary centres in 2007–2017 collected from a mandatory administrative database, the authors identified 466 patients who underwent an isolated tricuspid valve surgery. Most patients presented with advanced disease [47% in New York Heart Association (NYHA) class III/IV, 57% with right-sided heart failure signs]. TR was functional in 49% (22% with prior left-sided heart valve surgery and 27% isolated) and organic in 51% (infective endocarditis in 31% and other causes in 20%). In-hospital mortality and major complication rates were 10% and 31%, respectively. Rates of survival and survival free of heart failure readmission were 75% and 62% at 5 years. Independent determinants of outcomes were NYHA class III/IV [odds ratio (OR) 2.7], moderate/severe right ventricular dysfunction (OR 2.6), and lower prothrombin time (OR 0.9), while the mechanism of TR was not associated with the outcomes.
The authors conclude that isolated tricuspid valve surgery is associated with high mortality and morbidity, both in hospital and during follow-up, predicted by the severity of the presentation but not by the mechanism of TR. The results suggest that tricuspid valve interventions should be performed earlier in the course of the disease. The manuscript is accompanied by an Editorial by Victoria Delgado from the Leiden University Medical Center in the Netherlands and colleagues.6 The authors note that while data on the efficacy and durability of current transcatheter therapies are awaited, granular data such as those reported in the present article by Dreyfus et al.5 are important to highlight the need for early referral for isolated tricuspid valve intervention in patients with severe TR.
Mitral annular calcification (MAC) is a common degenerative mitral valve disease characterized by calcification at the level of the mitral annulus that can be associated with significant mitral valve dysfunction including both stenosis and regurgitation. MAC is associated with female sex, advanced age, chronic kidney disease, and multiple cardiovascular risk factors, and prevalence ranges from 8% to 15% in the general population and reaches as high as 40% among the elderly. In a clinical research manuscript entitled ‘Prognostic importance of the transmitral pressure gradient in mitral annular calcification with associated mitral valve dysfunction’, Philippe Bertrand from the Massachusetts General Hospital in Massachusetts, USA, and colleagues sought to define the natural history of patients with MAC-related mitral valve dysfunction and to assess the prognostic importance of mean transmitral pressure gradient and impact of concomitant mitral regurgitation (MR).7 The institutional echocardiography database was examined for the period 2001–2019 for all patients with MAC and mean gradient (MG) ≥3 mmHg. About 5700 patients were stratified by MG into low (3–5 mmHg), mid (5–10 mmHg), and high (≥10 mmHg) gradient. Primary outcome was all-cause mortality, and outcome models were adjusted for age, sex, and MAC-related risk factors (hypertension, diabetes, coronary artery disease, and chronic kidney disease). Mean transmitral pressure gradient was independently associated with mortality [adjusted hazard ratio (HR) 1.064 per 1 mmHg increase). MR severity was associated with mortality at low gradients but not at higher gradients.
Bertrand and colleagues conclude that in MAC-related mitral valve dysfunction, mean transmitral gradient is associated with increased mortality after adjustment for age, sex, and MAC-related risk factors. Concomitant MR is associated with excess mortality in low gradient ranges but gradually loses prognostic importance at higher gradients, indicating prognostic utility of the transmitral gradient in MAC regardless of MR severity. The manuscript is accompanied by an Editorial by Rebecca Hahn from Columbia University in New York, USA.8 who notes that any echocardiographic evidence for annular calcification may be an indication to use advanced multimodality imaging and novel biomarkers since these new tools may be the key to unlocking the mystery of intracardiac calcification and allow early detection and disease prevention.
Cardiac myxomas usually develop in the atria and consist of an acid mucopolysaccharide-rich myxoid matrix with polygonal stromal cells scattered throughout. These human benign tumours are a valuable research model because of the rarity of cardiac tumours, their clinical presentation, and uncertain origin. In a Translational Research article entitled ‘Atrial myxomas arise from multipotent cardiac stem cells’, Mariangela Scalise from the Magna Graecia University in Catanzaro, Italy, and colleagues assessed whether human adult cardiac stem cells give rise to myxoma stromal cells.9 The authors collected and analysed 23 myxomas for the presence of multipotent cardiac stem cells. They detected myxoma cells positive for c-kit. Most of the c-kit-positive cells were blood lineage-committed cells. However, blood lineage-uncommitted c-kit-positive cardiac myxoma cells expressed stemness and cardiac progenitor cell transcription factors. Approximately 10% of the blood lineage-uncommitted c-kit-positive cardiac myxoma cells expressed calretinin, a characteristic of myxoma stromal cells. In vitro, blood lineage-uncommitted c-kit-positive cardiac myxoma cells secreted chondroitin-6-sulfate and hyaluronic acid, which are the main components of the gelatinous myxoma matrix in vivo, and showed clonogenic, self-renewing, and sphere-forming properties (Figure 1).

The main findings of the study showing that cardiac myxomas arise from multipotent c-kitpos/CD45neg/CD31neg myxoma tumour initiating cells and the working hypothesis of their direct derivation from normal c-kitpos/CD45neg/CD31neg cardiac stem/progenitor cells transformed by specific miRNA modulation (from Scalise M, Torella M, Marino F, Ravo M, Giurato G, Vicinanza C, Cianflone E, Mancuso T, Aquila I, Salerno L, Nassa G, Agosti V, De Angelis A, Urbanek K, Berrino L, Veltri P, Paolino D, Mastroroberto P, De Feo M, Viglietto G, Weisz A, Nadal-Ginard B, Ellison-Hughes GM, Torella D. Atrial myxomas arise from multipotent cardiac stem cells. See pages 4332–4345).
The authors conclude that human myxoma is the first described cardiac stem cell-related human cardiac disease. This manuscript is accompanied by an Editorial by Mark Alan Sussman from the San Diego State University in California, USA10 who notes that Scalise et al. reveal the fundamental contribution of cardiac stem cells to atrial myxomas, offering provocative and tantalizing new insights for myocardial biology as well as strategic approaches to translational applications.
Management of VHD has dramatically changed over the last few decades. The primary goal has moved away from relieving symptoms once they occur to optimizing long-term morbidity and mortality, which requires timely intervention. Early symptoms (the start of a decline in exercise capacity/exertional shortness of breath) are a clear trigger for intervention, but even asymptomatic patients may be at risk when followed conservatively.11,12 The issue contains a State of the Art review article entitled ‘Timing of intervention in asymptomatic patients with valvular heart disease’ by Helmut Baumgartner from the University Hospital Muenster in Germany, and colleagues. The authors note that recommendations for treatment of patients with symptoms due to severe valvular disease are based on a foundation of solid evidence.4 However, when to intervene in asymptomatic patients remains controversial, and decision requires careful individual weighing of the potential benefits against the risk of intervention and its long-term consequences. The primary rationale for earlier intervention is prevention of irreversible left ventricular (LV) myocardial changes that might result in later clinical symptoms and adverse cardiac events. Various outcome predictors have been identified that facilitate decision-making. This review summarizes current recommendations and discusses recently published data that challenge them suggesting even earlier intervention. In adults with asymptomatic aortic stenosis, emerging risk markers include very severe valve obstruction, elevated serum natriuretic peptide levels, and imaging evidence of myocardial fibrosis or increased extracellular myocardial volume. Currently, transcatheter aortic valve implantation (TAVI) is not recommended for treatment of asymptomatic severe aortic stenosis although this may change in the future. In patients with aortic regurgitation, the potential benefit of early intervention in preventing LV dilation and dysfunction must be balanced against the long-term risk of a prosthetic valve, a particular concern because severe aortic regurgitation often occurs in younger patients with a congenital bicuspid valve. In patients with mitral stenosis, the option of transcatheter mitral balloon valvotomy tilts the balance towards earlier intervention to prevent atrial fibrillation, embolic events, and pulmonary hypertension. When chronic severe MR is due to mitral valve prolapse, anatomic features consistent with a high likelihood of a successful and durable valve repair favour early intervention. The authors conclude that optimal timing of intervention in adults with VHD is a constantly changing threshold that depends not only on the severity of valve disease but on the safety, efficacy, and long-term durability of our treatment options (Figure 2).
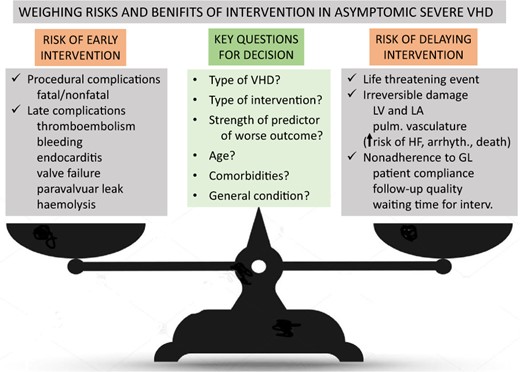
Weighing of risks and benefits of intervention in asymptomatic valvular heart disease. Aspects that need to be considered and key questions for decision-making. Arrhyth., arrhythmias; GL, guidelines; HF, heart failure; interv., intervention; LA, left atrium; LV, left ventricle; pulm., pulmonary; VHD, valvular heat disease (from Baumgartner H, Iung B, Otto CM. Timing of intervention in asymptomatic patients with valvular heart disease. See pages 4349–4356).
The issue is also complemented by Discussion Forum contributions. In a contribution entitled ‘Is the national readmission database the right database to identify valve-in-valve transcatheter aortic valve replacement patients?’, Salik Nazir from the University of Toledo in Toledo, Ohio, USA comment on the recent publication ‘Comparison of in-hospital outcomes and readmissions for valve-in-valve transcatheter aortic valve replacement vs. reoperative surgical aortic valve replacement: a contemporary assessment of real-world outcomes’ by Sameer A Hirji from Harvard Medical School in Boston, Massachusetts, USA, and colleagues.13,14 Hirji et al. respond in a separate comment.15
In a contribution entitled ‘Variable rate of stroke after transcatheter aortic valve replacement with self-expandable valves: more doubts than certainties’, Marco Ferlini from the Policlinico San Matteo in Pavia, Italy comment on the recent article ‘Comparison of newer generation self-expandable vs. balloon-expandable valves in transcatheter aortic valve implantation: the randomized SOLVE-TAVI trial’.16,17 Thiele et al. respond in a separate comment.18
The editors hope that this issue of the European Heart Journal will be of interest to its readers.
With thanks to Amelia Meier-Batschelet, Johanna Huggler, and Martin Meyer for help with compilation of this article.
References
Bertrand, PB, Churchill, TW, Yucel, E, Namasivayam, M, Bernard, S, Nagata, Y, He, W, Andrews, CT, Picard, MH, Weyman, AE, Levine, RA and Hung, J.




