-
PDF
- Split View
-
Views
-
Cite
Cite
N A Mark Estes, Samir Saba, Primary prevention of sudden death with the implantable cardioverter defibrillator: bridging the evidence gap, European Heart Journal, Volume 41, Issue 36, 21 September 2020, Pages 3448–3450, https://doi.org/10.1093/eurheartj/ehaa324
Close - Share Icon Share
This editorial refers to ‘Clinical effectiveness of primary prevention implantable cardioverter-defibrillators: results of the EU-CERT-ICD controlled multicentre cohort study’†, by M. Zabel et al., on page 3437.
Multiple randomized controlled trials of primary prevention of sudden cardiac death with the implantable cardioverter defibrillator (ICD) provided robust evidence of incremental mortality benefit over guideline-based medical therapy in patients with ischaemic and non-ischaemic cardiomyopathy with reduced left ventricular ejection fraction (LVEF).1–5 Based on these trials, published between 2002 and 2012, primary prevention ICDs continue to be recommended in current international guidelines.6 , 7 However, sudden death and total mortality have decreased in heart failure patients with improved medical therapy since these legacy ICD trials.8 , 9 A recent analysis of drug trials in heart failure patients with impaired LVEF, including >40 000 patients without ICDs enrolled in 12 clinical trials of pharmacological therapy, demonstrated a 44% decline in sudden death across the trials between 1995 and 2014.8 The cumulative incidence of sudden death at 90 days after randomization was 2.4% in the earliest trial and 1.0% in the most recent trial.8 The annual rate of sudden death per 100 patient-years in the treatment limbs decreased from 5.4 to 3.0 in long-term follow-up.8 These trends were attributed to the sequential introduction of angiotensin-converting enzyme inhibitors, beta-blockers, angiotensin receptor blockers, and mineralocorticoid receptor antagonists.8 The decreased risk of sudden death in recent heart failure trials has resulted in reasonable questions regarding continued survival benefit of primary prevention ICDs in this patient population.8 The lack of improved survival among patients with non-ischaemic cardiomyopathy with high rates of guideline-recommended pharmacological treatment and cardiac resynchronization therapy in the DANISH Trial has been represented as supporting lack of benefit.8 , 9 Notably, a meta-analysis combining all available randomized controlled trials of patients with non-ischaemic cardiomyopathy including the DANISH trial demonstrates a continued reduction in all-cause mortality.10 Addressing this gap in evidence regarding contemporary benefit of primary prevention ICDs is particularly important given the limited resources of healthcare systems. It is evident that randomizing patients with contemporary drug therapy to primary prevention ICDs would be unethical given the benefit demonstrated in the legacy trials.
In this issue of the European Heart Journal, Zabel and colleagues report on the results of the EU-CERT-ICD Multicenter Cohort Study assessing the clinical effectiveness of primary prevention ICD therapy.11 The investigators enrolled 2327 patients with ischaemic or non-ischaemic cardiomyopathy on optimal medical therapy with guideline indications for prophylactic ICD implantation in a prospective controlled cohort study in 44 centres in 15 European countries. The control group consisted of 731 patients not receiving ICDs despite guideline-based indications. The primary endpoint was all-cause mortality. During follow-up of 2.4 ± 1.1 years, 342 deaths occurred (6.3%/year annualized mortality, 5.6%/year in the ICD group vs. 9.2%/year in controls). The adjusted hazard ratio (HR; 0.713, P = 0.0016) for the primary endpoint with ICD treatment provides important evidence of continued benefit of primary prevention ICDs. Subgroup analyses indicated no ICD benefit in diabetics (adjusted HR 0.945, P = 0.7797) or those aged ≥75 years (adjusted HR 1.063, P = 0.8206). The authors conclude that patients with LVEF ≤35% and narrow QRS continue to derive benefit with primary prevention ICD treatment. ICD use was associated with a 27% lower mortality, with no survival advantage in older or diabetic patients.11
This study represents an important contribution assessing benefits of primary prevention ICDs in patients treated with optimal medical therapy. As with any non-randomized controlled trial, the investigation has limitations which are inherent to the study design.10 These include the possibility of unidentified and thereby unmeasured confounding variables.10 A treatment bias favouring the ICD patients cannot be excluded.10 Despite these limitations, which are acknowledged by the authors, their conclusions are valid and provide strong evidence of continued survival benefit in patients with ischaemic and non-ischaemic cardiomyopathy with prophylactic ICDs. Subgroup analyses indicating no ICD benefit in diabetics or those aged ≥75 years are important, as these observations emphasize the need for improvement in risk prediction models that can overcome the traditional exclusive reliance on ejection fraction.
Abundant evidence supports the notion that not all patients with low LVEF included in the original legacy trials derive benefit from primary prevention implantation of an ICD.1–5 , 11–15 Selection of patients based on LVEF is recognized to have many limitations as >50% of sudden deaths occur in patients with LVEF >35%. Furthermore, many patients receiving primary prevention ICDs never receive an appropriate ICD intervention before dying of heart failure or another non-arrhythmic cause. Subgroups of patients from retrospective analyses of multiple ICD trials and registries have identified patients most likely to derive benefit from ICD treatment.12–14 Risk stratification models primarily identify subsets of patients with low LVEF with the highest ratios of sudden death to total mortality (Figure 1).12–14 The Seattle Proportional Risk Model and Seattle Heart Failure Model have recently been demonstrated to identify patients in the DANISH Trial most likely to benefit from primary prevention ICD treatment.15 Among patient-specific risk factors identified are appropriate ICD intervention when compared with the corresponding risk of death without such intervention. It is only when there is a sufficiently high risk of appropriate ICD intervention and a low risk of non-arrhythmic mortality that sudden death reduction by an ICD would be expected to impact on total mortality. It follows that the benefit of primary prevention ICDs may be limited in patients with a low risk of appropriate device intervention and with a higher risk of death without such an intervention. All risk stratification models are derived from retrospective analyses of prior trials and registries, selecting patients at highest risk of sudden death when compared with total mortality (Figure 1). However, currently one of the fundamental principals of evidence-based medicine has not been fulfilled with validation of these models in prospective randomized trials.
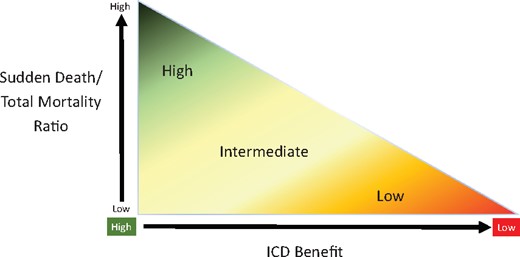
Paradigm for potential benefit of primary prevention ICD based on the ratio of sudden death to total mortality. The potential survival benefit of primary prevention ICDs can be divided into high, intermediate high, intermediate low, and low based on risk stratification models developed from retrospective analyses of primary prevention trials and registries but not prospectively validated.
By bridging the evidence gap and demonstrating contemporary mortality benefit with primary prevention ICDs in patients with decreased LVEF on optimal medical therapy, the EU-CERT-ICD Multicenter Cohort Study represents an important real-world contribution to current knowledge.11 Subgroup analyses in the study provide clinically useful insights into lack of benefit in diabetics and the elderly (>75 years).11 The incremental reduction of all-cause mortality with ICD is substantial in this study and provides support for continued patient selection based on current guidelines.6 , 7 , 11 Clinicians should remain mindful that meta-analyses provide robust evidence of continued mortality benefit with primary prevention ICDs in non-ischaemic cardiomyopathy.11 While risk stratification models have the potential to improve selection of patients with ischaemic and non-ischaemic cardiomyopathy for primary prevention ICDs, these models have not been prospectively validated. Adequately powered randomized studies are needed before implementation of changes to existing guidelines. However, guidelines guide while patients and physicians decide. In this process, clinicians should be mindful of available risk stratification models and subgroup analyses from the EU-CERT-ICD and other studies.11–15 It follows that the process of shared decision-making should include careful consideration of the patient’s wishes and values with an individualized assessment of potential benefit and risks of primary prevention ICDs placement.
Conflict of interest: N.A.M.E. reports receiving consulting fees from Medtronic, Boston Scientific, and Abbott. S.S. . reports receiving research support from Boston Scientific and Abbott.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
Footnotes
† doi:10.1093/eurheartj/ehaa226.
References



