-
PDF
- Split View
-
Views
-
Cite
Cite
Thomas F Lüscher, From TAVI to tricuspid cliping: fine-tuning the management of valvular heart disease, European Heart Journal, Volume 41, Issue 20, 21 May 2020, Pages 1863–1866, https://doi.org/10.1093/eurheartj/ehaa459
Close - Share Icon Share
 ensp;For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
ensp;For the podcast associated with this article, please visit https://dbpia.nl.go.kr/eurheartj/pages/Podcasts.
The management of valvular heart disease has undergone impressive developments during the last two decades.1 While the management of these conditions was primarily a surgical domain, today more patients are treated with catheter-based techniques for the aortic,2,3 mitral,4 pulmonary,5 and now also the tricuspid valve,6 with ever increasing success. While initially reserved for inoperable high-risk patients, transcatheter valve implantation (TAVI) in particular is now also considered for low-risk patients.7 However, the long-term performance of TAVI valves is still under debate. Furthermore, most valves and devices have only been tested with a product of a single manufacturer, and a comparison of self-expanding and balloon-expandable TAVI valves has only been done in a meta-analysis,8 but not in a randomized fashion. These problems are now addressed in this Focus Issue on valvular heart disease, starting with an article entitled ‘Long-term clinical outcome and performance of transcatheter aortic valve replacement with a self-expandable bioprosthesis’ by Luca Testa and colleagues from the Istituto Clinico S. Ambrogio in Milan, Italy.9 The authors note that in the last decade, TAVI has led to a paradigm shift in the treatment of patients with severe symptomatic aortic stenosis. Data on the long-term performance of TAVI valves are still limited. The authors evaluated the clinical and haemodynamic outcomes of the CoreValve self-expandable valve up to 8-year follow-up.
A total of 990 inoperable or high-risk patients were treated with the CoreValve transcatheter aortic valve. A significant functional improvement was observed in the majority and maintained over time, with 79% of survivors classified as NYHA class ≤II at 8 years (Figure 1). A total of 728 died within 8 years follow-up, leading to a 78.3% mortality. The transprosthetic gradient remained unchanged. The rate of grade 0/1 paravalvular leak (PVL) was consistent during follow-up, with no significant change from post-procedure to follow-up ≥5 years in paired analysis. At 8 years, moderate and severe structural valve deterioration was 3.0% and 1.6%, respectively, while late bioprosthetic valve failure was 2.5%. Thus, while the long-term performance and durability of TAVI valves is still questioned, the present study provides reassuring 8-year evidence on the CoreValve first-generation self-expandable bioprosthesis. These clinically important results are further discussed in an Editorial by Lars Sondergaard from the Rigshospitalet in Copenhagen, Denmark.10
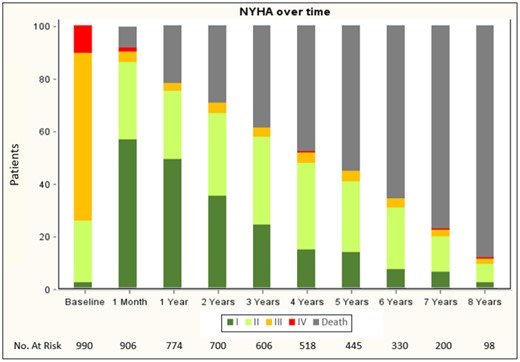
New York Heart Association class changes over time (from Testa L, Latib A, Brambilla N, De Marco F, Fiorina C, Adamo M, Giannini C, Angelillis M, Barbanti M, Sgroi C, Poli A, Ferrara E, Bruschi G, Russo CF, Matteo M, De Felice F, Musto C, Curello S, Colombo A, Tamburino C, Petronio AS, Bedogni F. Long-term clinical outcome and performance of transcatheter aortic valve replacement with a self-expandable bioprosthesis. See pages 1876–1886).
TAVI has now emerged as an established treatment option in patients with symptomatic aortic stenosis. However, the choice of the optimal valve is still a matter of debate. To address this question, Holger Thiele and colleagues from the University of Leipzig – Heart Center in Germany report in their article ‘Comparison of newer generation self-expandable vs. balloon-expandable valves in transcatheter aortic valve implantation’ the results of their randomized SOLVE-TAVI trial, a multicentre, open-label, 2 × 2 factorial, randomized trial of 447 patients with aortic stenosis.11 The primary endpoint of all-cause mortality, stroke, moderate or severe prosthetic valve regurgitation, and permanent pacemaker implantation occurred in 28.4% of patients receiving a CoreValve and in 26.1% of those with the balloon-expandable Edwards valve. Thus, in patients with aortic stenosis undergoing trans femoral TAVI, newer generation self-expandable and balloon-expandable valves are equivalent. These findings support their safe application in the majority of patients with some specific preferences based on individual valve anatomy. These important results are put into context in a thought-provoking Editorial by the pioneer of TAVI, John Webb, and colleagues from the St. Paul’s Hospital in Vancouver, Canada.12
Myocardial fibrosis might represent a key player in heart failure of patients with aortic stenosis. In their article ‘Impact of myocardial fibrosis on left ventricular remodelling, recovery, and outcome after transcatheter aortic valve implantation in different haemodynamic subtypes of severe aortic stenosis’ Miriam Puls and colleagues from the University Medical Centre Göttingen in Germany assessed its impact on left ventricular (LV) remodelling, recovery, and mortality after TAVI.13 Myocardial fibrosis differed significantly between aortic stenosis subtypes, with the highest levels of 30% in low LV ejection fraction (LVEF), low pressure gradient aortic stenosis, and the lowest levels of 14% in those with normal LVEF, high gradient aortic stenosis. In the entire cohort, high myocardial fibrosis was associated with poorer LV function, greater extent of LV remodelling, and more pronounced heart failure at baseline. After TAVI, high myocardial fibrosis was associated with a delay in normalization of LV geometry and function, but not per se with absence of reverse remodelling and clinical improvement. Multivariate analysis identified high myocardial fibrosis as an independent predictor of cardiovascular mortality with a hazard ratio of 27. Thus, histological myocardial fibrosis in aortic stenosis is associated with LV remodelling and cardiovascular mortality after TAVI. The clinical importance of these novel data is assessed in a well written Editorial by William Kong from the National University Heart Centre Singapore.14
Tricuspid valve regurgitation is the new frontier: long the Cinderella of valve disease, it has attracted increasing interest as it may affect outcome and is now amenable to catheter-based repair. 6,15,16 These new possibilities in the management of such patients is most important as their outcome is grim, as outlined in the article ‘Functional tricuspid regurgitation of degenerative mitral valve disease: a crucial determinant of survival’ by Maurice Enriquez-Sarano and colleagues from the Mayo Clinic in Rochester, Minnesota, USA.17 They assessed the functional tricuspid regurgitation determinants, consequences, and independent impact on outcome in degenerative mitral regurgitation in 5083 patients with normal LVEF. Functional tricuspid regurgitation was graded as trivial in 45%, mild in 37%, moderate in 15%, and severe in 3%. While systolic pulmonary pressure ≥50 mmHg was the most powerful predictor, other determinants were functional tricuspid regurgitation severity, older age, female sex, lower LVEF, degenerative mitral regurgitation, and particularly atrial fibrillation. Moderate or severe functional tricuspid regurgitation was independently linked to more severe clinical presentation, more oedema, lower stroke volume, and impaired renal function. Survival throughout follow-up was strongly associated with functional tricuspid regurgitation severity. Within 5 years of diagnosis, valve surgery was performed in 73% and 15% of severe and moderate degenerative mitral regurgitation, respectively and in only 26% and 6% of severe and moderate functional tricuspid regurgitation. Valvular surgery improved outcome without alleviating completely the higher mortality associated with functional tricuspid regurgitation. Thus, functional tricuspid regurgitation is frequent and causally not only linked to pulmonary hypertension, but also to atrial fibrillation. Severe tricuspid regurgitation is associated at diagnosis with more severe clinical presentation and eventually worse mortality, but remains profoundly undertreated. Thus, careful assessment, consideration for tricuspid surgery, and testing of new transcatheter therapy is warranted, as outlined by Georg Nickenig from the Universität Bonn in Germany in his balanced Editorial.18
This new frontier is further discussed in an interesting and balanced review entitled ‘Uncertainties and challenges in surgical and transcatheter tricuspid valve therapy: a state-of-the-art expert review’ by Osama Ibrahim Soliman and colleagues from the Thoraxcenter, Erasmus Medical Center Rotterdam in the Netherlands.4 They remind us that tricuspid regurgitation was historically often disregarded and undertreated, as thoroughly documented by the Mayo Clinic.17 Surgery with annuloplasty, leaflet repair, or valve replacement is currently the only Class I guideline-recommended therapy for tricuspid regurgitation. Many dedicated transcatheter tricuspid repair or replacement devices, which mimic well-established surgical techniques, are currently under development. Nevertheless, many aspects of tricuspid regurgitation are poorly understood, but Maurice Enriquez-Sarano and colleagues fortunately provided important insight into disease progression in their study this issue.17 Nevertheless, surgical or interventional risk stratification and predictors of successful therapy need to be developed. The optimal treatment timing and the choice of proper surgical or interventional technique for significant tricuspid regurgitation remain to be elucidated and should be thoroughly discussed in an experienced HeartTeam (Figure 2).
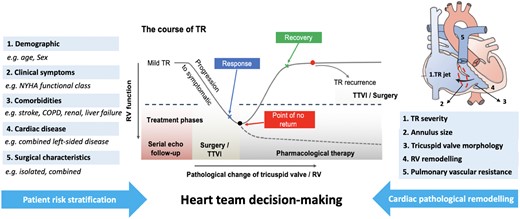
Heart team decision-making for treatment of tricuspid regurgitation. COPD, chronic obstructive pulmonary disease; NYHA, New York Heart Association; RV, right ventricle; TR, tricuspid regurgitation, TTVI, transcatheter tricuspid valve intervention (from Chang CC, Veen KM, Hahn RT, Bogers AJJC, Latib A, Oei FBS, Abdelghani M, Modolo R, Ho SY, Abdel-Wahab M, Fattouch K, Bosmans J, Caliskan K, Taramasso M, Serruys PW, Bax JJ, van Mieghem NMDA, Takkenberg JJM, Lurz P, Modine T, Soliman O. Uncertainties and challenges in surgical and transcatheter tricuspid valve therapy: a state-of-the-art expert review. See pages 1932–1940).
The issue is complemented by various Discussion Forum contributions. In a contribution entitled ‘High low-density lipoprotein levels and high risk of aortic stenosis’, Anders Greve from the Rigshospitalet in Copenhagen, Denmark comment on the recent contribution ‘Plasma lipids and risk of aortic valve stenosis: a Mendelian randomization study’ by Kazem Rahimi and colleagues from the University of Oxford in the UK.19,20 Rahimi et al. respond in a separate contribution. 21
The editors hope that the articles published in this issue of the European Heart Journal will be of interest to its readers.
With thanks to Amelia Meier-Batschelet for help with compilation of this article.
References




