-
Views
-
Cite
Cite
M Mehr, M Taramasso, T Ourrak, P Lurz, R S Von Bardeleben, N Fam, E Lubos, P Boekstegers, W Schillinger, B Plicht, H Eggebrecht, S Baldus, J Senges, F Maisano, J Hausleiter, 1385
Combined tricuspid and mitral vs. isolated mitral valve repair for severe mitral and tricuspid regurgitation: An analysis from TriValve and TRAMI registries, European Heart Journal, Volume 40, Issue Supplement_1, October 2019, ehz748.0052, https://doi.org/10.1093/eurheartj/ehz748.0052Close - Share Icon Share
Abstract
Edge-to-edge repair has been shown to be a successful therapeutic option for patients with severe mitral regurgitation (MR). Lately, it has also been emerging as a treatment perspective for severe tricuspid regurgitation (TR) in patients at high-risk for cardiac surgery. In patients, with both severe MR and TR the best treatment strategy for patients at high risk for surgery is unknown.
We retrospectively analyzed data from the international multicentre TriValve (Transcatheter Tricuspid Valve Therapies) registry and from the German multicentre TRAMI (Transcatheter Mitral Valve Interventions) registry. All patients included into the analysis had both severe MR and TR. Patients from the TRAMI registry (n=106) were treated with edge-to-edge repair in mitral position only. In patients from the TriValve registry (n=122), both valves were treated concomitantly in compassionate and/or off-label use. We sought to compare baseline characteristics, procedural data and 1-year mortality in both treatment groups.
228 patients (77±8 years; 44.3% female) were included into the analysis. All patients showed significant dyspnea on exposure (NYHA III or IV 93.9%). Kidney function (eGFR 42 ml/min/1,72m2) and the proportion of patients with significant pulmonary hypertension (59.0%) and COPD (23.7%) did not differ between the groups, but the proportion of patients with LV-EF <30% (34.9% vs. 18.0%, p<0.001) were higher in the TRAMI cohort.
At discharge, MR was comparably reduced in both groups (MR ≤ I° 75.9% vs. 77.3%, p=0.67). While all patients in both registries had significant TR at baseline, the percentage of patients with TR≥3+ at discharge was reduced to 18.6% in TriValve by the placement of 2±1 tricuspid clips/patient. The rate of in-hospital adverse events and the time of hospitalization did not differ in both cohorts. At 1-year, overall all-cause mortality was 34.0% in the TRAMI cohort and 16.4% in the TriValve cohort (p=0.0002, see figure; after adjustment for LVEF <30%: p=0.049). The rate of patients with NYHA ≤ II at 1 year did not differ between both cohorts (69.4% vs. 67.0%, p=0.54).
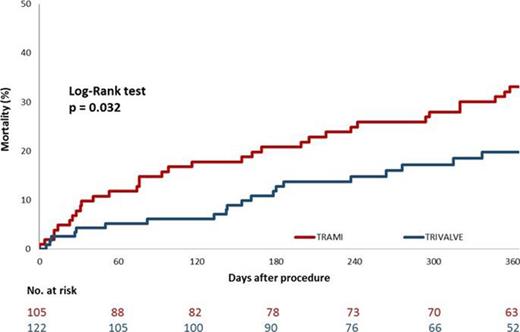
1-year mortality TriValve vs. TRAMI
Transcatheter mitral and tricuspid valve repair can result in a significant clinical improvement at 1 year. The concomitant treatment of both valve regurgitations may result in an improved survival, which needs to be confirmed in dedicated prospective trials.
- left ventricular ejection fraction
- mitral valve insufficiency
- tricuspid valve insufficiency
- mitral valve repair
- chronic obstructive airway disease
- cardiac surgery procedures
- repair of tricuspid valve
- mitral valve
- dyspnea
- tricuspid valve
- renal function
- heart valve diseases
- pulmonary hypertension
- surgical procedures, operative
- mortality
- surgery specialty
- off-label use
- mitral valve repair, edge-to-edge
- new york heart association classification
- adverse event





