-
PDF
- Split View
-
Views
-
Cite
Cite
Frazer Kirk, Kelsie Crathern, Andrie Stroebel, Video-assisted thoracoscopic sympathectomy for Harlequin syndrome, European Journal of Cardio-Thoracic Surgery, Volume 63, Issue 2, February 2023, ezac577, https://doi.org/10.1093/ejcts/ezac577
Close - Share Icon Share
Abstract
Harlequin syndrome is an exceedingly rare condition, characterized by unilateral facial flushing and hyperhidrosis. Postulated to be dysregulated sympathetic nervous system stimulation of the dermal vasculature and blood vessels of the face. There is no clear unifying pathological cause. Due to its heterogeneity and rarity, very little is known about the treatment of it. Hereafter, we describe our experience in successfully curing right-sided Harlequin syndrome through video-assisted thoracoscopic sympathectomy.
INTRODUCTION
First described in May of 1988, Harlequin syndrome was named after the English Folklore character ‘the harlequin’, for the similar appearance. It is characterized by unilateral facial flushing and hyperhidrosis with contralateral anhidrosis (Fig. 1), induced by exercises, stress or temperature change [1]. It has been observed as a benign physiology of neonates, or it may occur secondarily to immunological, cerebrovascular or neoplastic diseases (spinal cord tumours, apical lung cancers or goitre) and idiopathic cases have been described [2]. Equally, it has been documented as a temporary complication following paravertebral or thoracic epidural anaesthetics [3].

Preoperative photo demonstrating symptomatic Harlequin syndrome.
The leading pathophysiological theory is dysregulated/excessive sympathetic nervous system stimulation of the dermal vasculature and sweat glands on the affected side of the face. The sympathetic nervous system outflow to the face moves ipsilaterally from the thalamus, down the brainstem and spinal cord before moving laterally into the sympathetic chain, at the level of T1–T3. From the sympathetic chain, the sympathetic nerve fibres mix in the superior cervical ganglion and stellate ganglion before ascending along the carotid and its tributaries to the face. A lesion in any point of this outflow tract can produce harlequin syndrome [1] (Fig. 2).
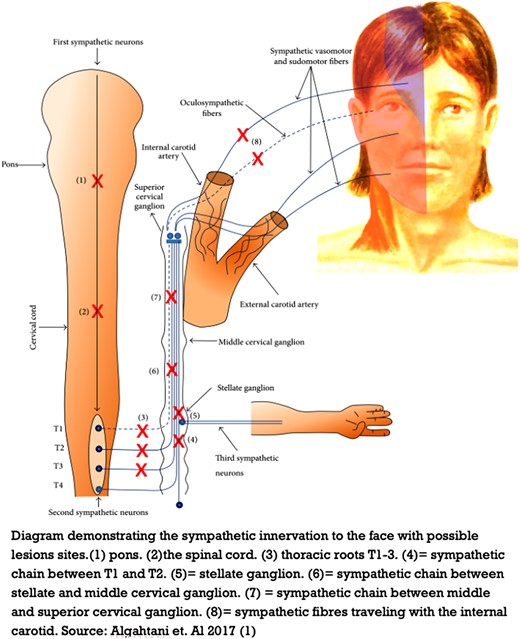
Pathophysiology of Harlequin syndrome. The copyright license permits use, as long as the original work is acknowledged. See below. PMC full text: Case Rep Med. 2017;2017:5342593. Published online 2017 Feb 21. doi: 10.1155/2017/5342593. Copyright/License Request permission to reuse Copyright © 2017 Hussein Algahtani et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
CASE REPORT
A 33-year-old female underwent an L4–L5 epidural anaesthetic for childbirth. She was later taken to theatre for removal of retained products at which point she received a spinal anaesthetic. She was discharged with a short course of antibiotics for post-partum fever but was otherwise well. Following discharge, she developed persistent right-sided Harlequin syndrome, without Horner’s syndrome or ophthalmic manifestation (Fig. 1) prompting review by neurology. Magnetic resonance imaging (MRI) and MRI angiography of her brain, neck and spine were unremarkable. No intervention was made by neurology, and the Harlequin syndrome was attributed to the anaesthetic administration. After 5 years of persistent Harlequin syndrome causing significant psychological stress, in light of working as a primary school teacher, she was referred for a sympathectomy at the age of 39.
A right-sided T2–T3 VATS sympathectomy was performed, utilizing a two-port technique and a 5-mm camera. Single lung ventilation and CO2 insufflation of the chest allowed for the identification of the sympathetic chain. The anatomy was normal and no aberrant accessory nerve was observed. The sympathetic chain was divided at the level of T2 and T3. The lung was re-inflated and the CO2 was drained from the chest using an underwater seal technique. The port sites were closed primarily without placing an intercostal catheter.
The patient had immediate resolution of the Harlequin syndrome, which has been sustained at 10 months follow-up.
DISCUSSION
The pathophysiology of Harlequin syndrome is poorly understood and given its many causes it likely varies. Harlequin syndrome can be a primarily idiopathic pathology and develop secondary manifestation of another condition/procedure. Secondary causes fall into two main categories; lesions of mass effect/anatomical lesions (i.e. apical lung cancer, cervical nerve sheath tumours, carotid dissection and thoracic syrinx) or a post-procedural/surgical complication (i.e. loco-regional anaesthetic blocks, Veno-Arterial Extracorporeal Membrane Oxygenation (VA-ECMO), carotid endarterectomy, thyroidectomy, anterior cervical discectomy and cervical/mediastinal mass excision). Fundamentally, it is believed to be due to excessive sympathetic stimulation of the dermal sweat glands and blood vessels of the face, through disruption/dysregulation of the sympathetic nervous system outflow tract (as described in Fig. 2) [1–4].
Harlequin syndrome has previously been attributed to paravertebral and thoracic epidural anaesthetics. The role of these agents in the absence of another cause in this case is contentious. Anaesthetic agents in theory should produce a transient Harlequin syndrome that resolves as the body metabolizes the anaesthetic agent. Furthermore, it usually coincides immediately with anaesthetic administration [3]. MRI of this patient demonstrated no other cause for Harlequin syndrome, so it could be argued that this was an idiopathic case of Harlequin syndrome.
Medical therapies including oxybutynin with propranolol or the use of botulim injections have been described in the past, with variable efficacy [4]. The use of these agents does not come without risk or side-effect, and in our institution, we have had no experience with the utilization of these for this condition. Consequently, surgical interventions were considered. Previously, a costotransversectomy and concurrent sympathectomy have been utilized to effectively treat Harlequin syndrome and, however, produced T1 radicular pain [5]. Reviewing the sympathetic nervous system outflow described in Fig. 2, disruption of the sympathetic chain at the level between T1 and T3 should be sufficient to block the sympathetic simulation to the face. However, examining this tract closely, ligation of T1 poses significant risk of the development of Horner’s syndrome and as such should be avoided (Fig. 2). Therefore, after careful discussion with the patient, we performed a T2–T3 sympathectomy based on the previous experience and theorized pathophysiology. Successfully treating our case of Harlequin syndrome, with VATS T2–T3 sympathectomy. While the underlying aetiology for Harlequin syndrome in our case remains unclear given it was temporally related to an epidural and spinal anaesthetic, the underling pathology was likely central/spinal. Consequently, we postulate by disrupting the sympathetic change at T2–T3 in the chest distal to the underlying central/spinal cause, the excessive sympathetic stimulation of the dermal blood vessels and sweat glands ceased and lead to the resolution of the condition.
Although only a single case report, this demonstrates that thoracic sympathectomy is beneficial in the management of Harlequin syndrome.
ETHICAL CONSIDERATIONS
Patient provided written consent for publishing. This study was approved by Gold Coast Hospital and Health Service, HREC Reference Number: EX/2022/QGC/81839.
Funding
No funding was supplied for this project.
Data Availability
The data underlying this article cannot be shared publicly for the privacy of individuals that participated in the study. The data will be shared on reasonable request to the corresponding author.
Conflict of interest: Nil to declare.
Reviewer information
European Journal of Cardio-Thoracic Surgery thanks Larry R Kaiser, Tevfik Kaplan and the other, anonymous reviewer(s) for their contribution to the peer review process of this article.
Presented at the E-Poster & Oral ISMICS Annual Scientific Meeting, Warsaw, Poland, 18 June 2022.




