-
PDF
- Split View
-
Views
-
Cite
Cite
Alessandro Della Corte, Federica Lo Presti, Wael Saade, Antonino Salvatore Rubino, Lucrezia Palmieri, Francesco Patanè, Fabio Miraldi, Marisa De Feo, Acute type A aortic dissection in bicuspid versus tricuspid aortic valve patients: focus on geometrical features of the aorta, European Journal of Cardio-Thoracic Surgery, Volume 63, Issue 2, February 2023, ezac576, https://doi.org/10.1093/ejcts/ezac576
Close - Share Icon Share
Abstract
This retrospective observational study aimed to assess the geometrical features, including diameters, length and angulation, of the ascending aorta with bicuspid and tricuspid aortic valve and to identify imaging markers potentially predicting whether aortopathy is likely to evolve chronically or to complicate with acute type A dissection.
Angio-computed-tomography scans of 354 patients (from 3 centres) with non-dilated (n = 97), aneurysmal (n = 100) or dissected aorta (n = 157) were reviewed. Diameters were measured at root, sinotubular junction, ascending, brachio-cephalic trunk origin; centreline lengths of the root and tubular tract and ascending-arch angle (between the ascending tubular tract axis and the proximal arch axis) were also measured. For 12 dissection patients, pre-dissection scans were available to investigate predisposing aortic geometry. Statistical analysis included: tricuspid versus bicuspid comparisons in each subgroup; univariate and multivariate analyses of the predictors of ascending-arch angle narrowing; and estimation of diagnostic accuracy of the angle parameter.
Diameters and lengths were similar between aneurysms and dissections, whereas dissections showed a significant ascending-arch angle narrowing (117 ± 13° in tricuspid, 115 ± 14° in bicuspid) compared to non-dilated and aneurysmal aortas (all P < 0.001). The best angle cut-off to discriminate dissection patients was 131° (96% sensitivity). In patients with a pre-dissection scan, Asc-Arch narrowing was already present before dissection. In non-dissected aortas over-angulation was predicted by root phenotype dilatation both in bicuspid and tricuspid patients. Bicuspid patients with non-dilated aorta showed elongated root (P = 0.027), a feature significantly correlated with Asc-Arch angle narrowing (P = 0.008).
The ascending-arch angle is promising as a risk marker for dissection to be used along with diameter. Its narrowing seems to be associated with elongation of the root, a feature that bicuspid patients can show even without significant dilatation. Root phenotype aortopathy may be at higher risk also with tricuspid aortic valve.
INTRODUCTION
Congenital bicuspid aortic valve (BAV) is today considered to be a valvulo-aortopathy, in view of the remarkable increase in the risk of both aortic valve disease and aortic aneurysm development that it implies [1]. Acute type A aortic dissection (ATAAD) is a rare but threatening complication of aortopathies: although BAV is contemplated among the conditions predisposing to ATAAD, the incremental risk of this event is lower than the one related to other aortopathies (e.g. genetically-determined connective tissue diseases). The discrepancy between the high risk of aneurysmal evolution and the much lower one of developing ATAAD in the long-term follow-up after BAV diagnosis is remarkable [2] but its reasons are unknown. Indeed, also for aortopathies with tricuspid aortic valve (TAV), what determines the fate of the ascending aorta is unknown, i.e. whether it continues to dilate becoming an aneurysm and requiring elective replacement or it abruptly suffers mechanical failure of the wall developing ATAAD.
Following recognition of the limited prognostic value of the aortic diameter for ATAAD risk, several alternative dimensional criteria have been explored [3] encompassing indexed cross-sectional dimensions, aortic length, aortic volume and others. We recently focused on the elongation of the aorta that can be observed in aortopathies [4] and on the chronic geometrical changes that accompany elongation [5]: being the supra-aortic branches and the heart the respective upper and lower boundaries, the ascending aorta cannot but increase its curvature and angulation while it elongates.
In the present study, we aimed to expand our previous analysis, now focusing on the differences in aortic geometry between BAV and TAV patients, and also to assess whether the increased risk of ATAAD in BAV aortopathy might be related to aorta geometry peculiarities.
PATIENTS AND METHODS
Ethical statement
The present study conforms to the Declaration of Helsinki. It was approved by our Institutional Review Board for Human Research (December 2018, prot. 8/2018): patients gave consent to the treatment of their clinical data for research purposes. Specific consent to this study was waived according to our Institutional Review Board, due to the retrospective observational nature of the investigation.
Study population
At the Cardiac Surgery Unit of the Monaldi Hospital, Naples, Italy, a previous pilot investigation on this topic was performed including 180 patients [5]: in the present continuation study, further 174 patients were added in the analysis, to validate the previous results and expand the focus to the comparison between BAV and TAV aortopathies. At 3 centres in 3 different Italian regions, electrocardiography-gated angio-computed-tomography (CT) scans of the thoracic or thoraco-abdominal aorta (routinely performed before either transcatheter aortic valve replacement or before cardiac surgery for ascending aortic aneurysm or ATAAD, plus other chest CT scans performed for any reason in patients admitted in cardiac surgery ward or outpatient clinic) were collected and reviewed. Possibly confounding conditions for the native geometry and angulation of the ascending aorta, e.g. previous aortic interventions, were reasons for exclusion from the study (see [5] for details). The resulting 354 eligible patients were divided into: normal aorta group (maximum diameter ≤45 mm, no sign of dissection: 97 patients), aortic aneurysm group (maximum diameter >45 mm, no sign of dissection: 100 patients) and ATAAD group (157 patients). According to echocardiography, CT scan and surgical observation, the aortic valves of all included patients were diagnosed as TAV (292 patients) or BAV (62 patients). In all BAV patients, the valvular morphotype (right–left fusion: RL; right–noncoronary fusion: RN) was defined.
For 120 non-ATAAD patients with aortic dilatation of any degree (including those between 40 and 45 mm diameter), the aortic phenotype was defined as previously established [6, 7]: ascending phenotype (diameter >40 mm at the tubular tract exceeding the diameter at the root) in 95, root phenotype (diameter >40 mm at the root equal to or exceeding the diameter at the tubular tract) in 25 patients.
Image analysis
In all CT scans of the aorta, in multiplanar reconstruction (MPR), the outer-outer diameters were re-measured, using common DICOM viewers including OsiriX (Pixmeo Ltd, Genève, CH) and Horos (Horosproject.org), at the following levels, orthogonally to the vessel’s centreline: root (at the level of the maximum bulging of the sinuses, commissure-to-sinus); sinotubular junction (STJ); mid-ascending tract (at the level of its maximum diameter); and proximal arch (at the most proximal point of the brachio-cephalic trunk take-off). In curved-MPR modality, the following curvilinear aortic length parameters were taken: root length by centreline method (from the ventriculo-aortic junction to the STJ), ascending tubular length at centreline (from the STJ to the origin of the brachio-cephalic trunk), tubular tract measured along its greater curvature (so-called ‘convexity’)—modifying the method reported in [8] by using curved MPR—total length of the ascending (root + tubular tract at centreline). Indexing the ascending length at the convexity to the ascending length at centreline we obtained the ‘deformation index’, a measure of the asymmetry of aortic bulging [5]. Supra-aortic vessels’ anatomy was assessed in the same angio-CT scans to define the presence of bovine arch. To quantify the angulation of the proximal aorta that accompanies elongation, the ‘Root-Asc’ angle, (angle between the coronal projections of the axes of the ventriculo-aortic junction plane and of the mid-ascending aorta cross-section) and the ‘Asc-Arch’ angle (between the coronal projections of the axes of the mid-ascending aorta and of the arch cross-section at the BCT take-off) were measured in 2D thick-slab mode with volume rendering, in the standard coronal view (see [5] and Fig. 1 for further details on the method of angle measurements). For angle measurements, good interobserver and intra-observer reproducibility had been already ascertained in our previous study [5].
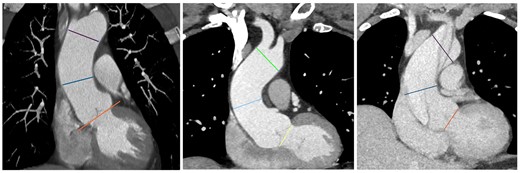
In 3 examples of standard coronal views (left: normal aorta; centre: root phenotype dilatation; right: acute type A aortic dissection), 2D thick-slab mode with volume rendering, the 3 landmark planes that were drawn manually are highlighted (ventriculo-aortic junction—root plane; mid-ascending aorta, level of the pulmonary trunk centre—ascending plane; origin of the brachio-cephalic trunk—arch plane): the angles between their axes (root-ascending angle; ascending-arch angle) were measured by using the Cobb’s angle plug-in.
Of the ATAAD patients, those who were alive in their follow-up were contacted and interviewed, in search for possible CT scan examinations performed before ATAAD occurrence: these were acquired and pre-dissection diameters, lengths and angles were measured, knowing that abrupt changes in aortic geometry occur with ATAAD onset [4, 9–11]. In ATAAD patients with no available pre-dissection CT imaging (145), the pre-dissection diameters were calculated according to the literature, using the weighted mean of percentage increase in diameters—from 4 studies [4, 9–11]—and length—from 2 studies [4, 9]—reported in the literature to occur acutely with ATAAD.
Statistical analysis
A central database was set, to collect data from all 3 centres. All continuous study variables were tested for normality of distribution and, since normal, were consistently presented as mean ± SD and analysed through parametric methods. Comparisons between groups for categorical variables were performed by chi-square with the exact test. Continuous variable comparisons between BAV and TAV subgroups (within each group: normal aorta, aneurysm, ATAAD) were performed by unpaired T-test. Continuous variable comparisons among 3 subgroups (normal aorta, aneurysm and ATAAD, within each of the 2 groups TAV and BAV) were performed by one-way ANOVA with Bonferroni post hoc analysis. Receiver operating characteristic (ROC) curve for the Asc-Arch angle was generated, in the whole study population and in TAV and BAV patients separately. The Youden test was used to identify the optimal value of the Asc-Arch angle predicting patient belonging to the ATAAD group. Correlations were tested by Pearson’s r correlation coefficient. A multivariable linear regression analysis, with stepwise method, was performed to identify the independent Asc-Arch angle predictors in non-ATAAD patients: only factors significantly (P < 0.05) associated with Asc-Arch angle in the univariate analysis were included in the regression model. The SPSS software ver 24.0 was used for the analysis (SPSS, IBM Corp., Armonk, NY).
All relevant data are within the manuscript and its supporting information files.
RESULTS
Geometrical features of the BAV versus TAV aorta
Table 1 shows the comparisons between TAV and BAV patients in each of the 3 groups (normal, aneurysmal, dissected aorta) in terms of anthropometrics, clinical data and geometric features of the aorta (diameters, lengths, angles). The non-dilated aorta with BAV showed significantly greater diameter at the tubular tract (P = 0.035), a trend of longer aorta, significant only for the root (P = 0.027) and similar angles compared to TAV. The aneurysmal aorta with BAV showed similar diameters, significantly longer ascending tract as measured at the convexity (P = 0.026) and a narrower Root-Asc angle compared to TAV (P = 0.038). There was a significantly higher prevalence of aortic valve stenosis in BAV compared to TAV in the aneurysm group. The dissecting aorta with BAV showed greater prevalence of aortic valve regurgitation, longer aortic root tract (P = 0.001) and greater diameters compared to TAV, although this latter difference did not reach significance for the low numbers in this group.
Comparisons between tricuspid aortic valve and bicuspid aortic valve patients in each of the 3 groups (normal aorta, aneurysms, acute type A aortic dissections)
| . | Normal . | Aneurysm . | ATAAD . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| TAV (n = 79) . | BAV (n = 18) . | P-Value* . | TAV (n = 71) . | BAV (n = 29) . | P-Value* . | TAV (n = 142) . | BAV (n = 15) . | P-Value* . | |
| Age (years), mean ± SD | 71 ± 11 | 63 ± 16 | 0.021 | 65 ± 10 | 60 ± 12 | 0.031 | 67 ± 12 | 59 ± 13 | 0.015 |
| Height (cm), mean ± SD | 165 ± 9 | 166 ± 8 | 0.82 | 169 ± 14 | 173 ± 9 | 0.20 | 170 ± 9 | 173 ± 8 | 0.16 |
| Gender (F) | 39% | 28% | 0.43 | 25% | 28% | 0.50 | 38% | 20% | 0.26 |
| Hypertension | 56% | 33% | 0.078 | 84% | 69% | 0.083 | 91% | 87% | 0.60 |
| AV stenosis | 56% | 72% | 0.19 | 13% | 34% | 0.012 | 4% | 0 | 0.66 |
| AV regurgitation | 20% | 39% | 0.17 | 42% | 52% | 0.39 | 25% | 80% | 0.001 |
| Root diameter, mean ± SD | 33 ± 4 | 34 ± 5 | 0.40 | 41 ± 7 | 40 ± 6 | 0.43 | 39 ± 7 | 43 ± 9 | 0.061 |
| STJ diameter, mean ± SD | 30 ± 4 | 31 ± 4 | 0.22 | 39 ± 7 | 37 ± 5 | 0.11 | 42 ± 9 | 46 ± 5 | 0.11 |
| Asc diameter, mean ± SD | 36 ± 4 | 38 ± 4 | 0.035 | 48 ± 7 | 50 ± 4 | 0.16 | 51 ± 11 | 53 ± 7 | 0.69 |
| Diameter at BCT, mean ± SD | 33 ± 4 | 33 ± 4 | 0.97 | 38 ± 4 | 39 ± 4 | 0.30 | 44 ± 8 | 41 ± 4 | 0.17 |
| Root length, mean ± SD | 20 ± 4 | 22 ± 3 | 0.027 | 25 ± 6 | 23 ± 6 | 0.075 | 26 ± 5 | 30 ± 6 | 0.005 |
| Asc length—centreline, mean ± SD | 72 ± 10 | 76 ± 12 | 0.20 | 87 ± 12 | 91 ± 14 | 0.16 | 90 ± 15 | 92 ± 13 | 0.76 |
| Asc length—convexity, mean ± SD | 94 ± 14 | 100 ± 11 | 0.11 | 117 ± 16 | 124 ± 13 | 0.026 | 126 ± 22 | 126 ± 17 | 0.95 |
| Total length (root + asc), mean ± SD | 92 ± 12 | 98 ± 13 | 0.065 | 112 ± 12 | 114 ± 15 | 0.52 | 116 ± 16 | 121 ± 14 | 0.23 |
| Deformation index, mean ± SD | 1.31 ± 0.1 | 1.43 ± 0.1 | 0.42 | 1.35 ± 0.1 | 1.39 ± 0.1 | 0.094 | 1.39 ± 0.1 | 1.39 ± 0.1 | 0.92 |
| Root-Asc angle (°), mean ± SD | 146 ± 16 | 142 ± 15 | 0.35 | 140 ± 17 | 132 ± 17 | 0.038 | 149 ± 14 | 150 ± 20 | 0.86 |
| Asc-Arch angle (°), mean ± SD | 134 ± 16 | 132 ± 17 | 0.59 | 134 ± 16 | 137 ± 18 | 0.40 | 117 ± 13 | 115 ± 14 | 0.41 |
| Bovine arch | 19% | 22% | 0.49 | 21% | 21% | 0.96 | 24% | 27% | 0.50 |
| Asc-Arch <131° | 47% | 33% | 0.43 | 42% | 38% | 0.82 | 96% | 100% | 0.56 |
| . | Normal . | Aneurysm . | ATAAD . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| TAV (n = 79) . | BAV (n = 18) . | P-Value* . | TAV (n = 71) . | BAV (n = 29) . | P-Value* . | TAV (n = 142) . | BAV (n = 15) . | P-Value* . | |
| Age (years), mean ± SD | 71 ± 11 | 63 ± 16 | 0.021 | 65 ± 10 | 60 ± 12 | 0.031 | 67 ± 12 | 59 ± 13 | 0.015 |
| Height (cm), mean ± SD | 165 ± 9 | 166 ± 8 | 0.82 | 169 ± 14 | 173 ± 9 | 0.20 | 170 ± 9 | 173 ± 8 | 0.16 |
| Gender (F) | 39% | 28% | 0.43 | 25% | 28% | 0.50 | 38% | 20% | 0.26 |
| Hypertension | 56% | 33% | 0.078 | 84% | 69% | 0.083 | 91% | 87% | 0.60 |
| AV stenosis | 56% | 72% | 0.19 | 13% | 34% | 0.012 | 4% | 0 | 0.66 |
| AV regurgitation | 20% | 39% | 0.17 | 42% | 52% | 0.39 | 25% | 80% | 0.001 |
| Root diameter, mean ± SD | 33 ± 4 | 34 ± 5 | 0.40 | 41 ± 7 | 40 ± 6 | 0.43 | 39 ± 7 | 43 ± 9 | 0.061 |
| STJ diameter, mean ± SD | 30 ± 4 | 31 ± 4 | 0.22 | 39 ± 7 | 37 ± 5 | 0.11 | 42 ± 9 | 46 ± 5 | 0.11 |
| Asc diameter, mean ± SD | 36 ± 4 | 38 ± 4 | 0.035 | 48 ± 7 | 50 ± 4 | 0.16 | 51 ± 11 | 53 ± 7 | 0.69 |
| Diameter at BCT, mean ± SD | 33 ± 4 | 33 ± 4 | 0.97 | 38 ± 4 | 39 ± 4 | 0.30 | 44 ± 8 | 41 ± 4 | 0.17 |
| Root length, mean ± SD | 20 ± 4 | 22 ± 3 | 0.027 | 25 ± 6 | 23 ± 6 | 0.075 | 26 ± 5 | 30 ± 6 | 0.005 |
| Asc length—centreline, mean ± SD | 72 ± 10 | 76 ± 12 | 0.20 | 87 ± 12 | 91 ± 14 | 0.16 | 90 ± 15 | 92 ± 13 | 0.76 |
| Asc length—convexity, mean ± SD | 94 ± 14 | 100 ± 11 | 0.11 | 117 ± 16 | 124 ± 13 | 0.026 | 126 ± 22 | 126 ± 17 | 0.95 |
| Total length (root + asc), mean ± SD | 92 ± 12 | 98 ± 13 | 0.065 | 112 ± 12 | 114 ± 15 | 0.52 | 116 ± 16 | 121 ± 14 | 0.23 |
| Deformation index, mean ± SD | 1.31 ± 0.1 | 1.43 ± 0.1 | 0.42 | 1.35 ± 0.1 | 1.39 ± 0.1 | 0.094 | 1.39 ± 0.1 | 1.39 ± 0.1 | 0.92 |
| Root-Asc angle (°), mean ± SD | 146 ± 16 | 142 ± 15 | 0.35 | 140 ± 17 | 132 ± 17 | 0.038 | 149 ± 14 | 150 ± 20 | 0.86 |
| Asc-Arch angle (°), mean ± SD | 134 ± 16 | 132 ± 17 | 0.59 | 134 ± 16 | 137 ± 18 | 0.40 | 117 ± 13 | 115 ± 14 | 0.41 |
| Bovine arch | 19% | 22% | 0.49 | 21% | 21% | 0.96 | 24% | 27% | 0.50 |
| Asc-Arch <131° | 47% | 33% | 0.43 | 42% | 38% | 0.82 | 96% | 100% | 0.56 |
Mean differences and confidence intervals for continuous variables are reported in Supplementary Material, Table S2. Lengths and diameters are expressed in mm.
P: T-test TAV versus BAV.
Asc: ascending; ATAAD: acute type A aortic dissection; AV: aortic valve; BAV: bicuspid aortic valve; BCT: brachio-cephalic trunk; F: female; SD: standard deviation; STJ: sinotubular junction; TAV: tricuspid aortic valve.
Sinificant p-values are in bold.
Comparisons between tricuspid aortic valve and bicuspid aortic valve patients in each of the 3 groups (normal aorta, aneurysms, acute type A aortic dissections)
| . | Normal . | Aneurysm . | ATAAD . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| TAV (n = 79) . | BAV (n = 18) . | P-Value* . | TAV (n = 71) . | BAV (n = 29) . | P-Value* . | TAV (n = 142) . | BAV (n = 15) . | P-Value* . | |
| Age (years), mean ± SD | 71 ± 11 | 63 ± 16 | 0.021 | 65 ± 10 | 60 ± 12 | 0.031 | 67 ± 12 | 59 ± 13 | 0.015 |
| Height (cm), mean ± SD | 165 ± 9 | 166 ± 8 | 0.82 | 169 ± 14 | 173 ± 9 | 0.20 | 170 ± 9 | 173 ± 8 | 0.16 |
| Gender (F) | 39% | 28% | 0.43 | 25% | 28% | 0.50 | 38% | 20% | 0.26 |
| Hypertension | 56% | 33% | 0.078 | 84% | 69% | 0.083 | 91% | 87% | 0.60 |
| AV stenosis | 56% | 72% | 0.19 | 13% | 34% | 0.012 | 4% | 0 | 0.66 |
| AV regurgitation | 20% | 39% | 0.17 | 42% | 52% | 0.39 | 25% | 80% | 0.001 |
| Root diameter, mean ± SD | 33 ± 4 | 34 ± 5 | 0.40 | 41 ± 7 | 40 ± 6 | 0.43 | 39 ± 7 | 43 ± 9 | 0.061 |
| STJ diameter, mean ± SD | 30 ± 4 | 31 ± 4 | 0.22 | 39 ± 7 | 37 ± 5 | 0.11 | 42 ± 9 | 46 ± 5 | 0.11 |
| Asc diameter, mean ± SD | 36 ± 4 | 38 ± 4 | 0.035 | 48 ± 7 | 50 ± 4 | 0.16 | 51 ± 11 | 53 ± 7 | 0.69 |
| Diameter at BCT, mean ± SD | 33 ± 4 | 33 ± 4 | 0.97 | 38 ± 4 | 39 ± 4 | 0.30 | 44 ± 8 | 41 ± 4 | 0.17 |
| Root length, mean ± SD | 20 ± 4 | 22 ± 3 | 0.027 | 25 ± 6 | 23 ± 6 | 0.075 | 26 ± 5 | 30 ± 6 | 0.005 |
| Asc length—centreline, mean ± SD | 72 ± 10 | 76 ± 12 | 0.20 | 87 ± 12 | 91 ± 14 | 0.16 | 90 ± 15 | 92 ± 13 | 0.76 |
| Asc length—convexity, mean ± SD | 94 ± 14 | 100 ± 11 | 0.11 | 117 ± 16 | 124 ± 13 | 0.026 | 126 ± 22 | 126 ± 17 | 0.95 |
| Total length (root + asc), mean ± SD | 92 ± 12 | 98 ± 13 | 0.065 | 112 ± 12 | 114 ± 15 | 0.52 | 116 ± 16 | 121 ± 14 | 0.23 |
| Deformation index, mean ± SD | 1.31 ± 0.1 | 1.43 ± 0.1 | 0.42 | 1.35 ± 0.1 | 1.39 ± 0.1 | 0.094 | 1.39 ± 0.1 | 1.39 ± 0.1 | 0.92 |
| Root-Asc angle (°), mean ± SD | 146 ± 16 | 142 ± 15 | 0.35 | 140 ± 17 | 132 ± 17 | 0.038 | 149 ± 14 | 150 ± 20 | 0.86 |
| Asc-Arch angle (°), mean ± SD | 134 ± 16 | 132 ± 17 | 0.59 | 134 ± 16 | 137 ± 18 | 0.40 | 117 ± 13 | 115 ± 14 | 0.41 |
| Bovine arch | 19% | 22% | 0.49 | 21% | 21% | 0.96 | 24% | 27% | 0.50 |
| Asc-Arch <131° | 47% | 33% | 0.43 | 42% | 38% | 0.82 | 96% | 100% | 0.56 |
| . | Normal . | Aneurysm . | ATAAD . | ||||||
|---|---|---|---|---|---|---|---|---|---|
| TAV (n = 79) . | BAV (n = 18) . | P-Value* . | TAV (n = 71) . | BAV (n = 29) . | P-Value* . | TAV (n = 142) . | BAV (n = 15) . | P-Value* . | |
| Age (years), mean ± SD | 71 ± 11 | 63 ± 16 | 0.021 | 65 ± 10 | 60 ± 12 | 0.031 | 67 ± 12 | 59 ± 13 | 0.015 |
| Height (cm), mean ± SD | 165 ± 9 | 166 ± 8 | 0.82 | 169 ± 14 | 173 ± 9 | 0.20 | 170 ± 9 | 173 ± 8 | 0.16 |
| Gender (F) | 39% | 28% | 0.43 | 25% | 28% | 0.50 | 38% | 20% | 0.26 |
| Hypertension | 56% | 33% | 0.078 | 84% | 69% | 0.083 | 91% | 87% | 0.60 |
| AV stenosis | 56% | 72% | 0.19 | 13% | 34% | 0.012 | 4% | 0 | 0.66 |
| AV regurgitation | 20% | 39% | 0.17 | 42% | 52% | 0.39 | 25% | 80% | 0.001 |
| Root diameter, mean ± SD | 33 ± 4 | 34 ± 5 | 0.40 | 41 ± 7 | 40 ± 6 | 0.43 | 39 ± 7 | 43 ± 9 | 0.061 |
| STJ diameter, mean ± SD | 30 ± 4 | 31 ± 4 | 0.22 | 39 ± 7 | 37 ± 5 | 0.11 | 42 ± 9 | 46 ± 5 | 0.11 |
| Asc diameter, mean ± SD | 36 ± 4 | 38 ± 4 | 0.035 | 48 ± 7 | 50 ± 4 | 0.16 | 51 ± 11 | 53 ± 7 | 0.69 |
| Diameter at BCT, mean ± SD | 33 ± 4 | 33 ± 4 | 0.97 | 38 ± 4 | 39 ± 4 | 0.30 | 44 ± 8 | 41 ± 4 | 0.17 |
| Root length, mean ± SD | 20 ± 4 | 22 ± 3 | 0.027 | 25 ± 6 | 23 ± 6 | 0.075 | 26 ± 5 | 30 ± 6 | 0.005 |
| Asc length—centreline, mean ± SD | 72 ± 10 | 76 ± 12 | 0.20 | 87 ± 12 | 91 ± 14 | 0.16 | 90 ± 15 | 92 ± 13 | 0.76 |
| Asc length—convexity, mean ± SD | 94 ± 14 | 100 ± 11 | 0.11 | 117 ± 16 | 124 ± 13 | 0.026 | 126 ± 22 | 126 ± 17 | 0.95 |
| Total length (root + asc), mean ± SD | 92 ± 12 | 98 ± 13 | 0.065 | 112 ± 12 | 114 ± 15 | 0.52 | 116 ± 16 | 121 ± 14 | 0.23 |
| Deformation index, mean ± SD | 1.31 ± 0.1 | 1.43 ± 0.1 | 0.42 | 1.35 ± 0.1 | 1.39 ± 0.1 | 0.094 | 1.39 ± 0.1 | 1.39 ± 0.1 | 0.92 |
| Root-Asc angle (°), mean ± SD | 146 ± 16 | 142 ± 15 | 0.35 | 140 ± 17 | 132 ± 17 | 0.038 | 149 ± 14 | 150 ± 20 | 0.86 |
| Asc-Arch angle (°), mean ± SD | 134 ± 16 | 132 ± 17 | 0.59 | 134 ± 16 | 137 ± 18 | 0.40 | 117 ± 13 | 115 ± 14 | 0.41 |
| Bovine arch | 19% | 22% | 0.49 | 21% | 21% | 0.96 | 24% | 27% | 0.50 |
| Asc-Arch <131° | 47% | 33% | 0.43 | 42% | 38% | 0.82 | 96% | 100% | 0.56 |
Mean differences and confidence intervals for continuous variables are reported in Supplementary Material, Table S2. Lengths and diameters are expressed in mm.
P: T-test TAV versus BAV.
Asc: ascending; ATAAD: acute type A aortic dissection; AV: aortic valve; BAV: bicuspid aortic valve; BCT: brachio-cephalic trunk; F: female; SD: standard deviation; STJ: sinotubular junction; TAV: tricuspid aortic valve.
Sinificant p-values are in bold.
Among BAV patients there were no significant differences between the 2 valve morphotypes in terms of geometry of the aorta: only, in RN-BAVs, the diameter at proximal arch tended to be greater (40 ± 5 vs 37 ± 5 mm; P = 0.054) than in RL-BAVs.
Aortic geometrical parameters in ATAADs versus aneurysms
As expected, both aneurysmal aortas and ATAADs showed significantly greater lengths than non-dilated aortas. When compared to TAV aneurysms, TAV-ATAADs showed greater diameters (see diameter values in Table 1) only at the STJ (P = 0.034 at Bonferroni post hoc test for ANOVA), at tubular tract (P = 0.011) and proximal arch (P < 0.001). Differences in length between TAV-ATAADs and TAV aneurysms were not significant.
In BAV patients, among diameters, only the STJ differed significantly between ATAADs and aneurysms (46 ± 5 vs 37 ± 5 mm; P = 0.001) and as length measurements are concerned the root tract was significantly more elongated in ATAADs than in aneurysms (30 ± 6 vs 23 ± 6 mm; P < 0.001), with similar length of the ascending tubular tract. Aneurysms showed a consistently narrower Root-Asc angle (values in Table 1) compared to normal aortas and ATAADs; ATAADs showed a significantly narrower Asc-Arch angle compared to normal and aneurysms, both with TAV and BAV (Fig. 2).
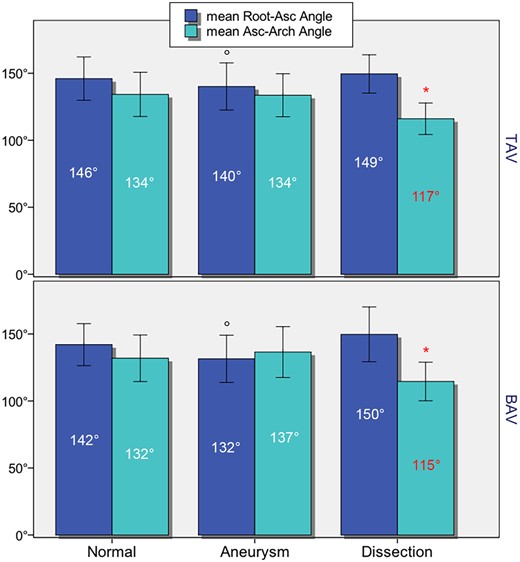
Bar graph showing mean Root-Asc angles and mean Asc-Arch angles in the 3 subgroups (normal aorta, aneurysms, ATAADs) for tricuspid aortic valve and bicuspid aortic valve patients; *P < 0.001 ATAADs versus aneurysms and non-dilated aortas; °P < 0.001 aneurysms versus ATAADs and non-dilated aortas. ATAADs: acute type A aortic dissections.
Pre-dissection observed and estimated measurements
In the 12 ATAAD patients (10 TAV, 2 BAV) whose pre-dissection CT scans were found, the mean time interval between pre- and post-dissection scans was 14 ± 8 months and the mean pre-dissection maximum diameter was 43 ± 7 mm: the mean acute increase in diameter from pre-dissection to post-dissection scans was 20%. The mean pre-dissection length was 105 ± 14 mm showing an acute increase in length of 5%. The mean pre-dissection Asc-Arch angle was narrowed in all 12 (mean 120 ± 8°), showing that after ATAAD occurrence the angle had decreased by 3% on average. The difference in diameters and length between pre- and post-dissection images in those 12 patients was similar to those reported in the literature [4, 9–11] (Supplementary Material, Table S2). In the other 145 ATAAD patients, the mean estimated pre-dissection diameter in the BAV-ATAAD subgroup (46.5 ± 6 mm) was greater than in the TAV-ATAAD subgroup (41.5 ± 6 mm; P = 0.054).
Discriminating ability of the Asc-Arch angle parameter
Since narrowing of the Asc-Arch angle was unique of the ATAAD group, the diagnostic ability of this parameter for ATAAD was tested. ROC curve in the whole study population is shown in Fig. 3 [area under the curve (AUC) 0.815; 95% confidence interval (CI) = 0.77–0.86]. For TAV patients only, the AUC was 0.809 (95% CI = 0.76–0.86), and for BAV 0.843 (95% CI = 0.74–0.94). The Youden test identified 131° as the best cut-off value in the whole study population, with a sensitivity of 96% and a specificity of 58%.
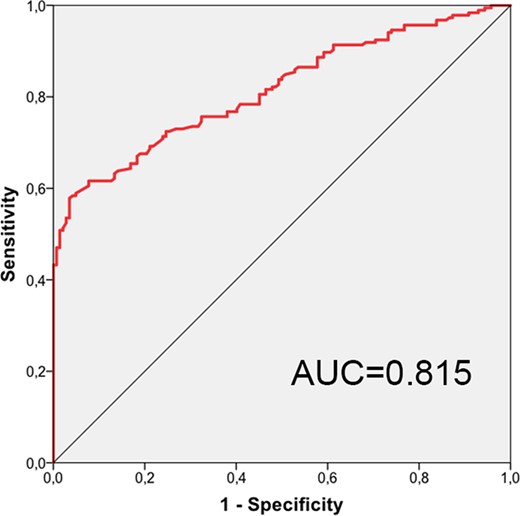
Receiver operating characteristic curve showing diagnostic accuracy of Asc-Arch angle for prediction of patient belonging to the acute type A aortic dissection group. AUC: area under the curve.
Phenotype of aortic dilatation
In the overall population, the prevalence of either aortic phenotype (ascending: 80%; root: 20%) was identical between BAV and TAV patients. In patients with aneurysm, an ascending phenotype was significantly more frequent with BAV (93%) than with TAV (75%, P = 0.029); conversely, in ATAADs, BAV was associated with the higher prevalence of root phenotype (40%) than TAV (16%, P = 0.037) (Fig. 4).
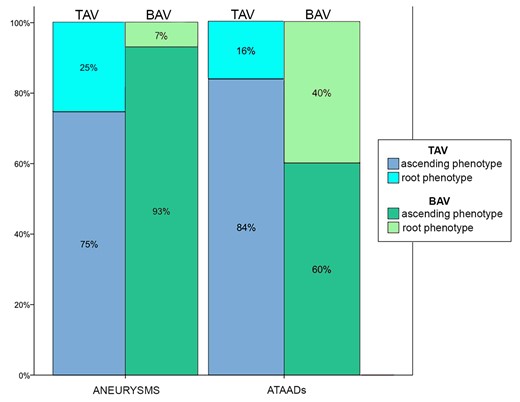
Bar graph showing the prevalence of ascending phenotype and root phenotype in each of 4 patient subgroups: TAV aneurysms; BAV aneurysms; TAV-ATAADs; and BAV-ATAADs (percentages are out of the subgroup total). There was a significant association of root phenotype with ATAADs in BAV patients (40% vs 7%; P = 0.013), not with TAV (16% vs 25%; P = 0.14). Significance of the comparisons BAV-ATAADs versus TAV-ATAADs and BAV aneurysm versus TAV aneurysms are reported in the text. ATAADs: acute type A aortic dissections; BAV: bicuspid aortic valve; TAV: tricuspid aortic valve.
Predictors of aortic angulation
Once ATAAD patients were excluded from the analysis, those with a root phenotype dilatation had a mean Asc-Arch angle significantly narrower (122 ± 17° vs 137 ± 17°) than those with ascending phenotype dilatation (P < 0.001). Correlations of the Asc-Arch angle with aortic dimensions in non-ATAAD patients are shown in Table 2.
Significant correlations between aortic dimensions and Asc-Arch angle in tricuspid aortic valve (n = 150) and bicuspid aortic valve (n = 47) non-acute type A aortic dissection subpopulations are shown
| . | Root diameter . | Root length . | Total length . | Deformation index . |
|---|---|---|---|---|
| Asc-Arch in TAV | r = −0.21; P = 0.042 | r = −0.39; P < 0.001 | – | r = −0.26; P = 0.002 |
| Asc-Arch in BAV | – | r = −0.39; P = 0.008 | r = −0.18; P = 0.034 | r = −0.44; P = 0.002 |
| . | Root diameter . | Root length . | Total length . | Deformation index . |
|---|---|---|---|---|
| Asc-Arch in TAV | r = −0.21; P = 0.042 | r = −0.39; P < 0.001 | – | r = −0.26; P = 0.002 |
| Asc-Arch in BAV | – | r = −0.39; P = 0.008 | r = −0.18; P = 0.034 | r = −0.44; P = 0.002 |
Correlations with age, gender, anthropometrics and ascending diameter and length were weak both for tricuspid aortic valve and bicuspid aortic valve patients (r < 0.2; P > 0.05).
BAV: bicuspid aortic valve; TAV: tricuspid aortic valve.
Significant correlations between aortic dimensions and Asc-Arch angle in tricuspid aortic valve (n = 150) and bicuspid aortic valve (n = 47) non-acute type A aortic dissection subpopulations are shown
| . | Root diameter . | Root length . | Total length . | Deformation index . |
|---|---|---|---|---|
| Asc-Arch in TAV | r = −0.21; P = 0.042 | r = −0.39; P < 0.001 | – | r = −0.26; P = 0.002 |
| Asc-Arch in BAV | – | r = −0.39; P = 0.008 | r = −0.18; P = 0.034 | r = −0.44; P = 0.002 |
| . | Root diameter . | Root length . | Total length . | Deformation index . |
|---|---|---|---|---|
| Asc-Arch in TAV | r = −0.21; P = 0.042 | r = −0.39; P < 0.001 | – | r = −0.26; P = 0.002 |
| Asc-Arch in BAV | – | r = −0.39; P = 0.008 | r = −0.18; P = 0.034 | r = −0.44; P = 0.002 |
Correlations with age, gender, anthropometrics and ascending diameter and length were weak both for tricuspid aortic valve and bicuspid aortic valve patients (r < 0.2; P > 0.05).
BAV: bicuspid aortic valve; TAV: tricuspid aortic valve.
Multivariable linear regression analyses showed that the Asc-Arch angle was predicted by root phenotype (P < 0.001) and deformation index (P = 0.027) in TAV patients (Rsquare of the model = 0.28) and by root phenotype (P = 0.042) and root length (P = 0.028) in BAV patients; Rsquare of the model = 0.56).
DISCUSSION
The present multicentre investigation represents the continuation and expansion of our recent single-centre pilot study [5]. There we highlighted, in a smaller population, that both dilated and dissected aortas are elongated compared to normal, however with 2 different modes of aortic elongation: (i) in ascending aneurysms, the increasing length of the aorta forces it to accentuate its curvature by horizontalization of the root segment (narrowing of the Root-Asc angle) and (ii) in ATAADs, conversely, the angulation between the ascending tract and the proximal arch is exacerbated (narrowing of the Asc-Arch angle). The analysis of the present series, including an ATAAD patient-group more than four-fold larger than in that previous study, confirmed the above evidence, thus corroborating the hypothesis that a geometrical configuration unique of the aorta with a higher risk of dissection can be defined. Moreover, the small sample of pre-dissection CT scans available showed that the Asc-Arch angle was already importantly narrowed before dissection, suggesting that this phenomenon is not just a consequence of the acute changes in geometry accompanying dissection development [9].
Distal ascending aortic over-angulation may predict ATAAD
Importantly, the difference observed between aneurysmal aortas, with narrowing of the Root-Asc angle (proximal ascending over-angulation), and ATAADs, with narrowing of the Asc-Arch angle (distal ascending over-angulation) [5] was here confirmed for both TAV and BAV patients. It is known that in BAV aortopathy, when the ascending phenotype is the case, the aorta tends to dilate asymmetrically, for predominant dilatation of the greater curvature of the ascending tubular tract (convexity) [12, 13]. When aneurysm subgroups were analysed, BAV presented greater elongation of the tubular tract than TAV when measured at the convexity, but not at centreline. It is intuitive that with a predominant elongation of the convexity, BAV aneurysms show a more marked dislocation and horizontalization of the root segment: consistently, the Root-Asc angle was more narrowed in BAV than in TAV aneurysms (Fig. 2). Conversely, the Asc-Arch angle in ATAADs showed a similar degree of narrowing in TAV and BAV patients; when the discriminating accuracy of this parameter in identifying ATAADs was verified by ROC curves, the AUC was similar (between 0.8 and 0.84) for both valve type groups. Therefore, the Asc-Arch angle is confirmed to hold potential for risk prediction of aortic dissection, since its narrowing is strongly associated with ATAAD; it seems to be a predisposing factor instead of simply an epiphenomenon, and it shows very good sensitivity, with modest specificity. Considering that the maximum diameter, which is the main criterion used today to indicate elective surgery for the ascending aorta, is a highly specific but scarcely sensitive risk marker for ATAAD [14, 15], the Asc-Arch angle could be the optimal synergistic risk factor to consider together with diameter and possibly length, to improve overall prognostic accuracy and prevent a higher number of ATAAD cases.
Root phenotype and root elongation are signs of more malignant aortopathy
Another important finding was the relevance of root segment disease to the narrowing of the Asc-Arch angle (Fig. 5). The angle showed a significant inverse correlation with the length of the root, not the tubular tract, in both TAV and BAV patients without ATAAD (Table 2): also, root phenotype was an independent predictor of the Asc-Arch angle in both TAV and BAV non-ATAAD patients in multivariable analysis. In BAV aortopathy, it has been already thoroughly demonstrated that the root phenotype represents a more dreadful form of the disease: several clinical features testify this, from faster rate of annual dilatation growth [7] to higher prevalence of aortopathy among relatives [16], from greater risk of acute complications of the aorta following aortic valve replacement [17] to root aneurysm prevalence enrichment in BAV-ATAAD series [18]. Strikingly, 2 recent large mixed series including TAV patients with non-genetical aortic diseases reported a greater risk of ATAAD [19] as well as its occurrence at smaller diameters [20], in those with predominant root location of the aortopathy, even without BAV. This agrees with our present observations and may confirm the hypothesis that, regardless of valve type, a narrow Asc-Arch angle, as observed in root phenotype, predisposes to ATAAD. Future guidelines should probably put due emphasis on the greater malignancy of all ‘root phenotype’ aortopathies, like the American Association for Thoracic Surgery 2018 consensus guidelines already did for BAV aortopathy only [13].
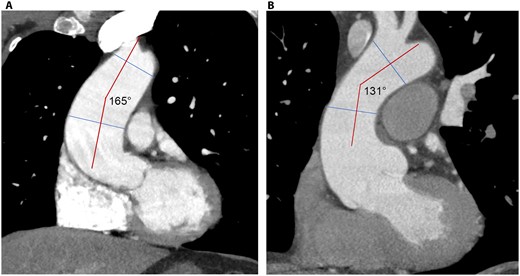
Two examples of aortic dilatations with bicuspid aortic valve: (A) ascending phenotype without Asc-Arch angle narrowing and (B) root phenotype with Asc-Arch angle narrowing.
Bicuspid aortic valve-associated changes in ascending aorta geometry
Even in the subgroup without aneurysm or dissection, the bicuspid aorta showed unique geometrical features, i.e. greater ascending diameters (as already known from the literature [21, 22]) and significantly longer root segment (an unprecedented finding) compared to TAV, albeit in younger subjects. In light of the association of root elongation with Asc-Arch narrowing, the longer root tract in BAV patients with normal aortic diameter seems to fit with the long-known 9-fold higher risk of dissection compared to the general population [2]. As discussed above, the geometry of the BAV aorta with aneurysmal enlargement was completely different: since the ascending phenotype accounted for more than 90% of cases, the mean root length was not increased compared to normal whereas the tubular tract greater curvature was significantly elongated (length at the convexity), with normal Asc-Arch angle (Fig. 5).
In BAV patients with ATAAD, there was a relatively high prevalence of root phenotype instead: estimated pre-dissection diameters were greater than with TAV, consistent with several reports in literature [23]. In summary, BAV aortopathy presents a starker dichotomy than TAV between 2 geometrical patterns: 1 unique of aneurysmal dilatation (diameters and lengths: ascending > root; wide Asc-Arch) and 1 characterized by root dilatation and elongation, which is typically observed in ATAADs (diameters and lengths: root > ascending; narrow Asc-Arch).
Is Asc-Arch angle narrowing a surrogate measure for aortic elongation?
Finding an explanation for the observed link between root elongation, Asc-Arch angle narrowing and ATAAD falls beyond the present study objectives and design. Distal ascending over-angulation accompanying elongation of the root segment may be merely a sign of intrinsic more severe derangement of aortic wall structure or also play a mechanistic role through alteration of biomechanical forces in the ascending aorta.
In the absence of pathogenetic explanations, it may be deemed uncertain whether the Asc-Arch angle or the root length should be considered as the real predictor of ATAAD. From a practical viewpoint, measuring root length might be hampered by difficult definition of the STJ, especially when this level is involved in dilatation [4]: however, compared to echocardiography, CT carries the advantage of allowing precise visualization of the coronary origins which may help defining the STJ level. Nevertheless, we believe the Asc-Arch angle, with its good interobserver and intra-observer variability [5] is to be preferred: notably, in ROC curve analyses, it showed higher AUC (0.815) than root length (AUC = 0.706, see Supplementary Material, Fig. S1).
Limitations
The main limitation of the present analysis lies in the relatively small number of BAV patients included: this was likely to affect the comparisons between TAV and BAV subgroups (e.g. BAV-ATAADs versus TAV-ATAADs). However, the fact that the main findings (association of Asc-Arch narrowing with ATAAD and correlation of root length with Asc-Arch angle) were statistically significant even with relatively small BAV patient numbers can attest the robustness of the observation. The analysis was indeed exploratory in nature, so P-values are not confirmatory but rather descriptive.
The only way to ultimately verify the predictive power of Asc-Arch, being prospective studies on ATAAD practically impossible, would be through retrospective analysis of a large amount of paired pre-dissection and post-dissection angio-CT scans. We have faced major difficulties in searching for pre-dissection exams in the present study population, being able to obtain them in only <8% patients. Our number of pre-dissection scans, however, compares well with the literature, where only 4 studies collected pre-dissection scans [4, 9–11], obtaining a number of pre-dissection studies ranging from 10 to 63 patients).
CONCLUSIONS
The present study confirmed the previous suggestion that Asc-Arch angle narrowing, related to the elongation of the aortic root, may represent a risk marker for ATAAD. If further validated, it might be used in combination with the diameter, to which it appears to be an optimal complement, for more accurate risk stratification of both TAV- and BAV-associated aortopathies. The root phenotype dilatation, initially identified as a more malignant form of BAV aortopathy [7] and today suggested to represent a riskier disease also for non-bicuspid patients [19, 20], was associated with narrowing of the Asc-Arch angle in non-dissected aortas. Whether root elongation can be an early warning sign may deserve further investigation: if confirmed, this may represent one of the mechanisms underlying the risk of dissection in BAV patients, here showing elongated root even when the aorta was not dilated.
SUPPLEMENTARY MATERIAL
Supplementary material is available at EJCTS online.
Conflict of interest: none declared.
Author contributions
Alessandro Della Corte: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Writing—original draft. Federica Lo Presti: Data curation; Investigation; Methodology; Writing—original draft. Wael Saade: Data curation; Investigation; Resources; Validation. Antonino Salvatore Rubino: Data curation; Formal analysis; Methodology; Validation. Lucrezia Palmieri: Investigation; Software. Francesco Patanè: Investigation; Software; Visualization. Fabio Miraldi: Investigation; Supervision; Visualization. Marisa De Feo: Resources; Supervision; Visualization.
Reviewer information
European Journal of Cardio-Thoracic Surgery thanks Tobias Krüger and the other, anonymous reviewer(s) for their contribution to the peer review process of this article.
Presented at the 36th EACTS Annual Meeting, Milan, Italy, 6 October 2022.
REFERENCES
ABBREVIATIONS
- ATAAD
Acute type A aortic dissection
- AUC
Area under the curve
- BAV
Bicuspid aortic valve
- CI
Confidence interval
- MPR
Multiplanar reconstruction
- ROC
Receiver operating characteristic
- STJ
Sinotubular junction
- TAV
Tricuspid aortic valve





